Chapter 2: CARDIOVASCULAR SYSTEM
Introduction
Blood Cells A single drop of blood contains millions of red blood cells. These cells have no nucleus so that they efficiently carry oxygen and carbon dioxide whilst being able to fit through extremely small spaces.
Chapter Objectives
After studying this chapter, you will be able to:
- Discuss the structure and function of erythrocytes and leukocytes
- Describe the internal and external anatomy of the heart
- Trace the pathway of oxygenated and deoxygenated blood through the heart, to examine the relationship between the chambers of the heart and the pulmonary and systemic circulations
- Compare and contrast the microscopic structure of arteries, arterioles, capillaries, venules, and veins
- Label the major blood vessels of the pulmonary and systemic circulations
- Identify and describe the hepatic portal system
Single-celled organisms do not need blood. They obtain nutrients directly from and excrete wastes directly into their environment. The human organism cannot do that. Our large, complex bodies need blood to deliver nutrients to and remove wastes from our trillions of cells. The heart pumps blood throughout the body in a network of blood vessels. Together, these three components—blood, heart, and vessels—make up the cardiovascular system.
Blood Cells
Learning Objectives
By the end of this section, you will be able to:
- Describe the anatomy of erythrocytes
- Describe the general characteristics of leukocytes
- Classify leukocytes according to their lineage, their main structural features, and their primary functions
The erythrocyte, commonly known as a red blood cell (or RBC), is by far the most common component of blood: A single drop of blood contains millions of erythrocytes and just thousands of leukocytes. In fact, erythrocytes are estimated to make up about 25% of the total cells in the body. As you can imagine, they are quite small cells, with a mean diameter of only about 7–8 micrometers (µm) (Figure 18.8). The primary functions of erythrocytes are to pick up inhaled oxygen from the lungs and transport it to the body’s tissues, and to pick up some (about 24%) carbon dioxide waste at the tissues and transport it to the lungs for exhalation. Erythrocytes remain within the vascular network. Although leukocytes typically leave the blood vessels to perform their defensive functions, movement of erythrocytes from the blood vessels is abnormal.
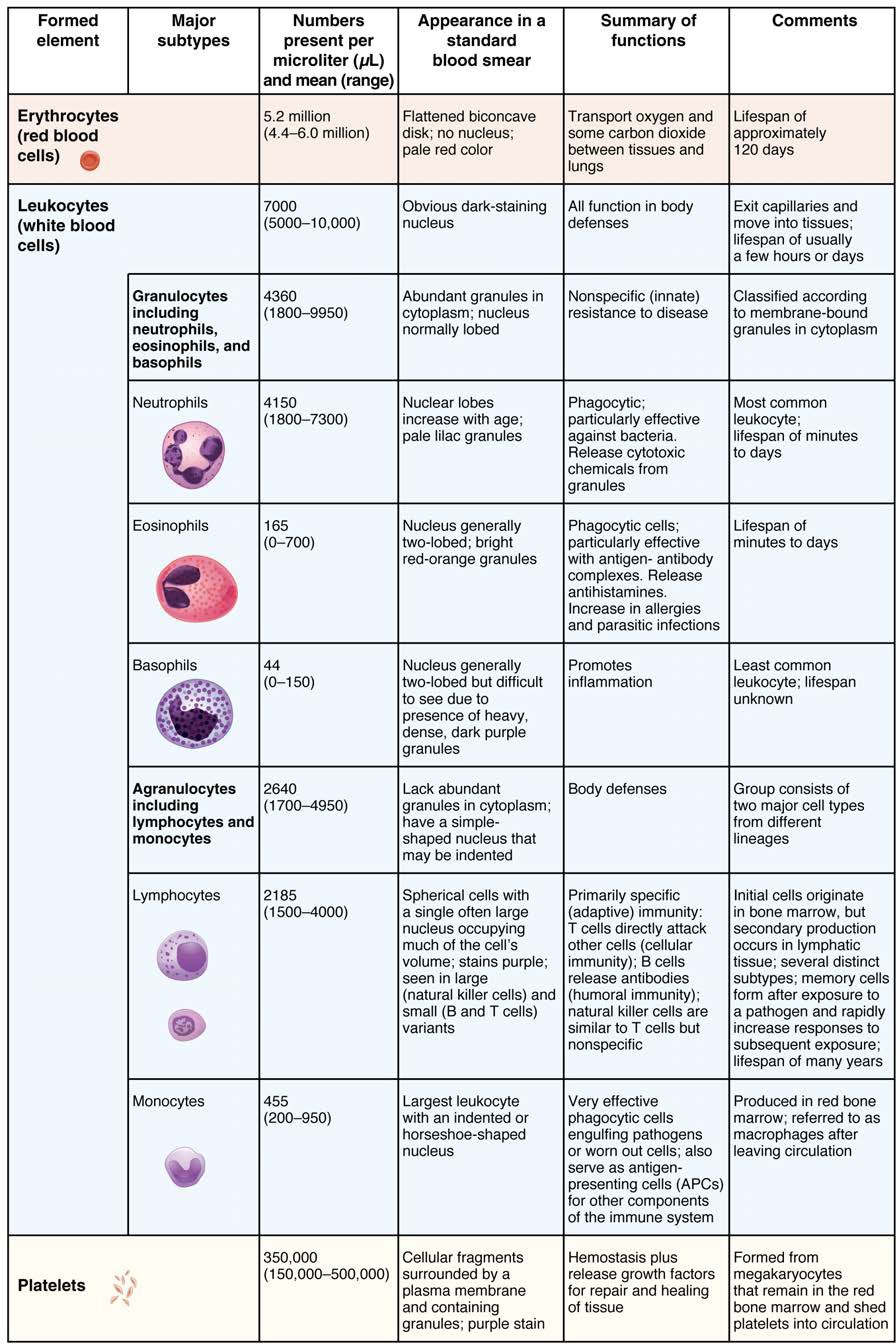
Figure 18.8 Summary of Formed Elements in Blood
Erythrocytes
As an erythrocyte matures in the red bone marrow, it extrudes its nucleus and most of its other organelles. Lacking mitochondria (the energy producing organelle in a cell), for example, they rely on anaerobic respiration. This means that they do not utilise any of the oxygen they are transporting, so they can deliver it all to the tissues. Erythrocytes do, however, contain some structural proteins that help the blood cells maintain their unique structure and enable them to change their shape to squeeze through capillaries.
Erythrocytes are biconcave disks; that is, they are plump at their periphery and very thin in the centre (Figure 18.9). Since they lack most organelles, there is more interior space for the presence of the hemoglobin molecules that transport gases. The biconcave shape also provides a greater surface area across which gas exchange can occur, relative to its volume; a sphere of a similar diameter would have a lower surface area-to-volume ratio. In the capillaries, the oxygen carried by the erythrocytes can diffuse into the plasma and then through the capillary walls to reach the cells, whereas some of the carbon dioxide produced by the cells as a waste product diffuses into the capillaries to be picked up by the erythrocytes. Capillary beds are extremely narrow, slowing the passage of the erythrocytes and providing an extended opportunity for gas exchange to occur. However, the space within capillaries can be so minute that, despite their own small size, erythrocytes may have to fold in on themselves if they are to make their way through. Fortunately, their structural proteins are flexible, allowing them to bend over themselves to a surprising degree, then spring back again when they enter a wider vessel. In wider vessels, erythrocytes may stack up much like a roll of coins, forming a rouleaux, from the French word for “roll.”
Figure 18.9 Shape of Erythrocytes Erythrocytes are biconcave discs with very shallow centres. This shape optimises the ratio of surface area to volume, facilitating gas exchange. It also enables them to fold up as they move through narrow blood vessels.
Leukocytes
The leukocyte, commonly known as a white blood cell (or WBC), is a major component of the body’s defenses against disease. Leukocytes protect the body against invading microorganisms and body cells with mutated DNA, and they clean up debris. Platelets are essential for the repair of blood vessels when damage to them has occurred; they also provide growth factors for healing and repair. See Figure 18.7 for a summary of leukocytes and platelets.
Although leukocytes and erythrocytes both originate from hematopoietic stem cells in the bone marrow, they are very different from each other in many significant ways. For instance, leukocytes are far less numerous than erythrocytes, they are larger than erythrocytes and they possess a nucleus and organelles. And although there is just one type of erythrocyte, there are many types of leukocytes. Most of these types have a much shorter lifespan than that of erythrocytes, some as short as a few hours or even a few minutes in the case of acute infection.
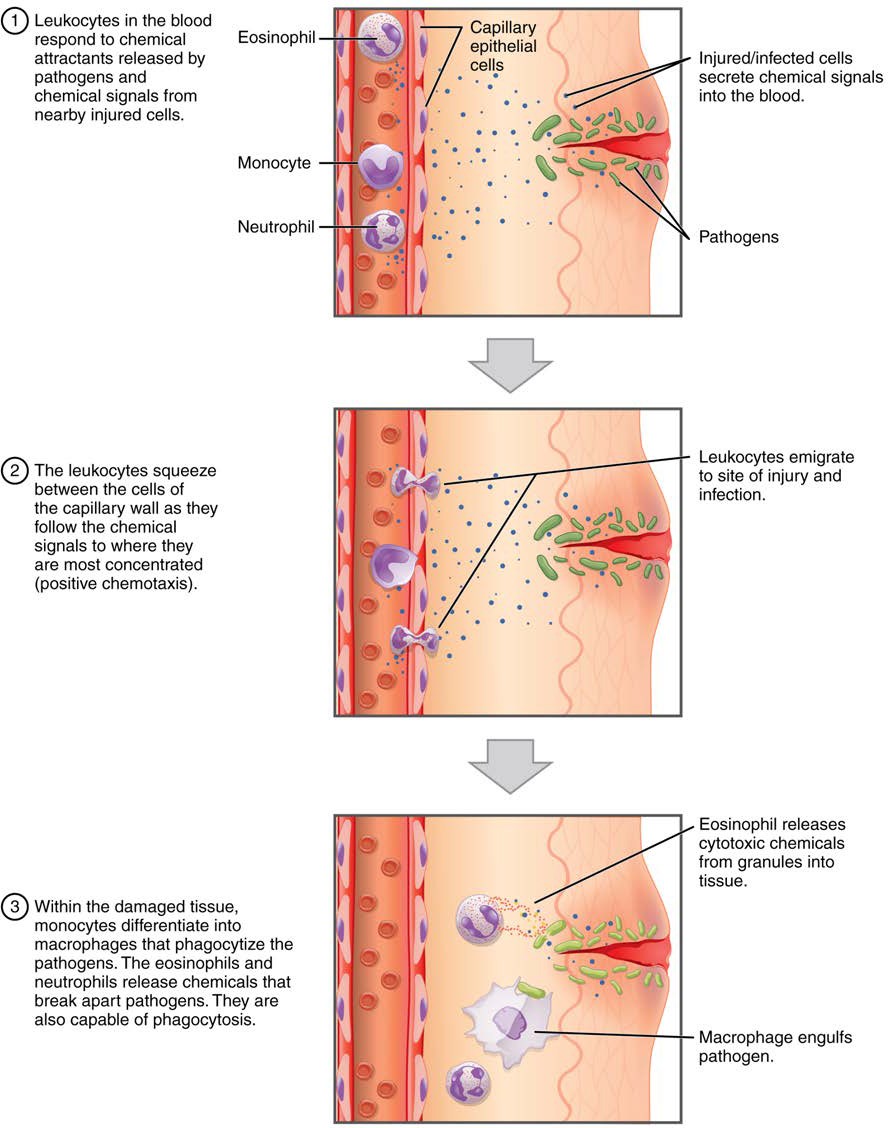
One of the most distinctive characteristics of leukocytes is their movement. Whereas erythrocytes spend their days circulating within the blood vessels, leukocytes routinely leave the bloodstream to perform their defensive functions in the body’s tissues. For leukocytes, the vascular network is simply a highway they travel and soon exit to reach their true destination. When they arrive, they are often given distinct names, such as macrophage or microglia, depending on their function (Figure 18.13). Once they have exited the capillaries, some leukocytes will take up fixed positions in lymphatic tissue, bone marrow, the spleen, the thymus, or other organs. Others will move about through the tissue spaces, continuously extending their plasma membranes, sometimes wandering freely, and sometimes moving toward the direction in which they are drawn by chemical signals. This attracting of leukocytes occurs because of positive chemotaxis (literally “movement in response to chemicals”), a phenomenon in which injured or infected cells and nearby leukocytes emit the equivalent of a chemical “911” call, attracting more leukocytes to the site. In clinical medicine, the differential counts of the types and percentages of leukocytes present are often key indicators in making a diagnosis and selecting a treatment.
Figure 18.13 Emigration (diapedesis) Leukocytes exit the blood vessel and then move through the connective tissue of the dermis toward the site of a wound. Some leukocytes, such as the eosinophil and neutrophil, are characterised as granular leukocytes. They release chemicals from their granules that destroy pathogens; they are also capable of phagocytosis. The monocyte, an agranular leukocyte, differentiates into a macrophage that then phagocytoses the pathogens.
Classification of Leukocytes
When scientists first began to observe stained blood slides, it quickly became evident that leukocytes could be divided into two groups, according to whether their cytoplasm contained highly visible granules:
- Granular leukocytes (granulocytes) contain abundant granules within the cytoplasm. They include neutrophils, eosinophils and basophils.
- While granules are not totally lacking in agranular leukocytes (agranulocytes), they are far fewer and less obvious. Agranular leukocytes include monocytes, which mature into macrophages that are phagocytic, and lymphocytes, which arise from the lymphoid stem cell line.
Granular Leukocytes
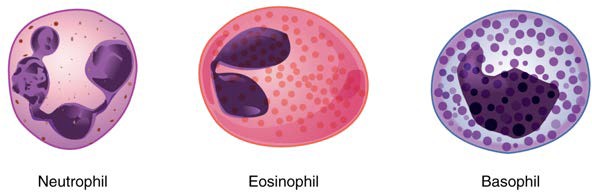
We will consider the granular leukocytes in order from most common to least common. All of these are produced in the red bone marrow and have a short lifespan of hours to days. They typically have a lobed nucleus and are classified according to which type of stain best highlights their granules (Figure 18.14).
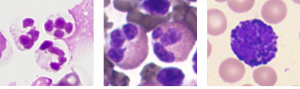
Figure 18.14 Granular Leukocytes A neutrophil has small granules that stain light lilac and a nucleus with two to five lobes. The granules of eosinophils are slightly larger and stain reddish-orange, and its nucleus has two to three lobes. A basophil has large granules that stain dark blue to purple and a two-lobed nucleus. [Micrographs attributed to Dr Paul Shield, Queensland University of Technology]
Agranular Leukocytes
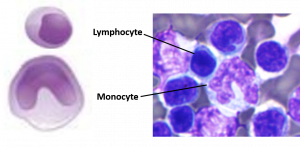
Agranular leukocytes contain smaller, less-visible granules in their cytoplasm than do granular leukocytes. The nucleus is simple in shape, sometimes with an indentation but without distinct lobes. There are two major types of agranulocytes: lymphocytes and monocytes (see Figure 18.15).
Figure 18.15 Agranular Leukocytes Agranulocytes lack cytoplasmic granules. The lymphocyte has a large prominent nucleus, with little to no visible cytoplasm. Monocytes are the largest leukocytes and contain a horseshoe shaped nucleus. [Micrographs attributed to Dr Paul Shield, Queensland University of Technology]
INTERACTIVE ACTIVITY
(a) Classify the two granulocytes that you identified by their subtype.
(b) Identify examples of agranulocytes in this blood smear. Name each example and describe their morphological features.
Platelets
A platelet is not a cell but rather a fragment of the cytoplasm of a cell called a megakaryocyte that is surrounded by a plasma membrane. Megakaryocytes are large, typically 50–100 µm in diameter, and contain an enlarged, lobed nucleus. Megakaryocytes remain within bone marrow tissue (Figure 18.16) and ultimately form platelet-precursor extensions that extend through the walls of bone marrow capillaries to release into the circulation thousands of cytoplasmic fragments, each enclosed by a bit of plasma membrane. These enclosed fragments are platelets.
Platelets are relatively small, 2–4 µm in diameter, but numerous, with typically 150,000–160,000 per µL of blood. After entering the circulation, approximately one-third migrate to the spleen for storage for later release in response to any rupture in a blood vessel. They then become activated to perform their primary function, which is to limit blood loss. Platelets remain only about 10 days, then are phagocytosed by macrophages. Platelets are critical to hemostasis, the stoppage of blood flow following damage to a vessel. They also secrete a variety of growth factors essential for growth and repair of tissue, particularly connective tissue. Infusions of concentrated platelets are now being used in some therapies to stimulate healing.
Heart Anatomy
Learning Objectives
By the end of this section, you will be able to:
- Describe the location and orientation of the heart within the body, including the relationship between the chambers of the heart and the great vessels
- Describe the internal and external anatomy of the heart, and be able to explain how the muscles and valves of the heart contribute to its function as a pump
- Describe the coronary circulation system
- Trace the pathway of oxygenated and deoxygenated blood through the heart, to examine the relationship between the chambers of the heart and the pulmonary and systemic circulations
There is no single better word to describe the function of the heart other than “pump”, since its contraction develops the pressure that ejects blood into the major vessels: the aorta and pulmonary trunk. From these vessels, the blood is distributed to the remainder of the body. The vital importance of the heart is obvious. If one assumes an average rate of contraction of 75 contractions per minute, a human heart would contract approximately 108,000 times in one day, more than 39 million times in one year, and nearly 3 billion times during a 75-year lifespan. Each of the major pumping chambers of the heart ejects approximately 70 mL blood per contraction in a resting adult. This would be equal to 5.25 litres of fluid per minute and approximately 14,000 liters per day. Over one year, that would equal 10,000,000 liters or 2.6 million gallons of blood sent through roughly 60,000 miles of vessels. In order to understand how that happens, it is necessary to first understand the anatomy of the heart.
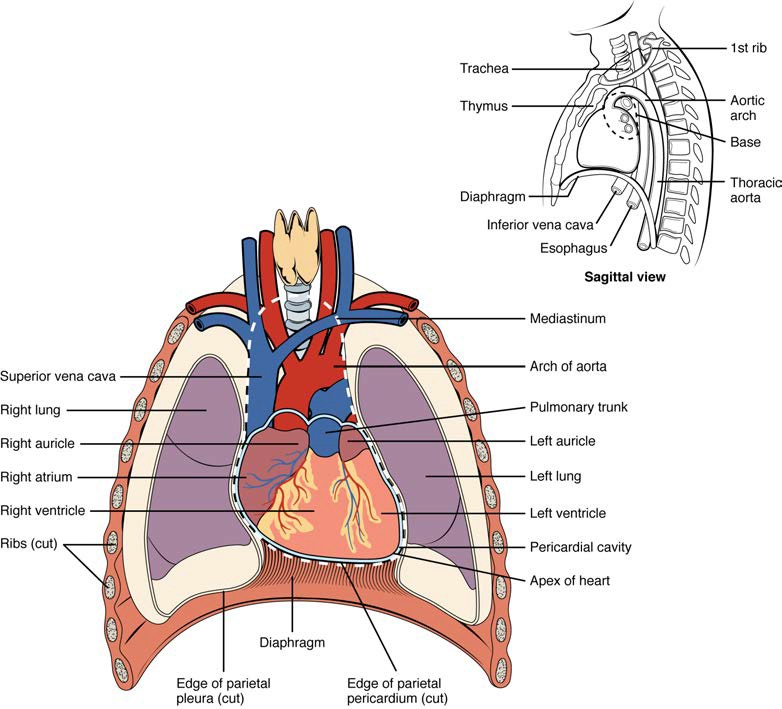
Location of the Heart
The human heart is located within the thoracic cavity, medially between the lungs in the space known as the mediastinum. Figure 19.2 shows the position of the heart within the thoracic cavity. Within the mediastinum, the heart is separated from the other mediastinal structures by a tough membrane known as the pericardium, or pericardial sac, and sits in its own space called the pericardial cavity. The posterior surface of the heart lies near the bodies of the vertebrae, and its anterior surface sits deep to the sternum and costal cartilages. The great veins, the superior and inferior venae cavae, and the great arteries, the aorta and pulmonary trunk, are attached to the superior surface of the heart, called the base. The base of the heart is located at the level of the third costal cartilage, as seen in Figure 19.2. The inferior tip of the heart, the apex, lies just to the left of the sternum between the junction of the fourth and fifth ribs near their articulation with the costal cartilages. The right side of the heart is deflected anteriorly, and the left side is deflected posteriorly. It is important to remember the position and orientation of the heart when placing a stethoscope on the chest of a patient and listening for heart sounds, and also when looking at images taken from a midsagittal perspective.
Figure 19.2 Position of the Heart in the Thorax The heart is located within the thoracic cavity, medially between the lungs in the mediastinum. It is about the size of a fist, is broad superiorly, and tapers inferiorly.
Shape and Size of the Heart
The shape of the heart is similar to a pinecone, rather broad at the superior surface and tapering to the apex (see Figure 19.2). A typical heart is approximately the size of your fist: 12 cm in length, 8 cm wide, and 6 cm in thickness. Given the size difference between most members of the sexes, the weight of a female heart is approximately 250–300 grams, and the weight of a male heart is approximately 300–350 grams.
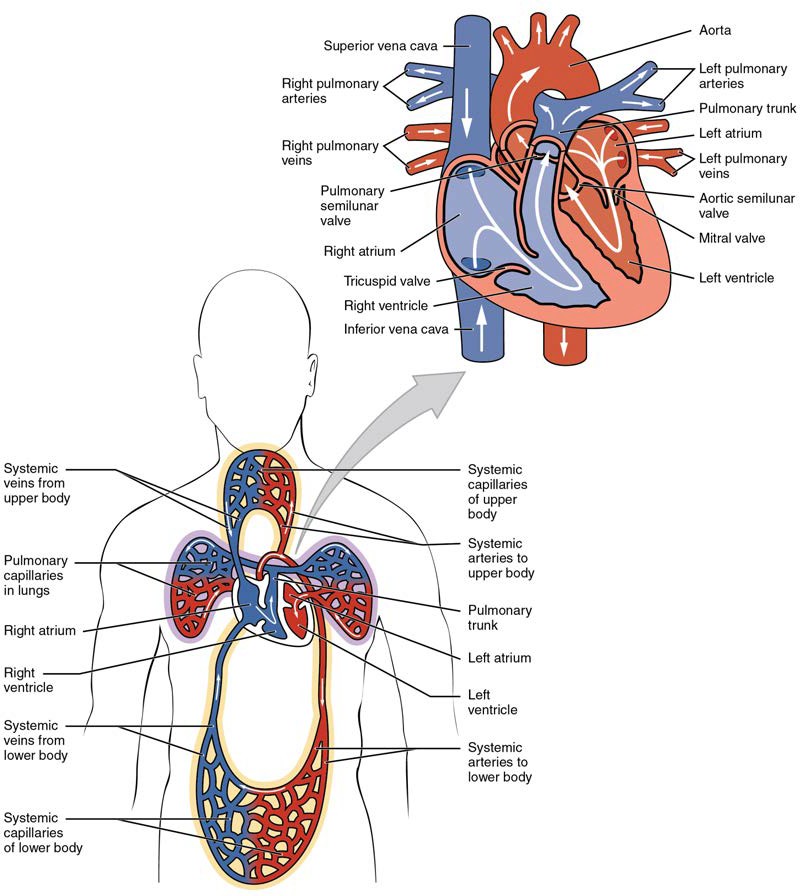
Chambers and Circulation through the Heart
The human heart consists of four chambers: The left side and the right side each have one atrium and one ventricle. Each of the superior chambers, the right atrium (plural = atria) and the left atrium, act as a receiving chamber and contract to push blood into the inferior chambers, the right ventricle and the left ventricle. The ventricles serve as the primary pumping chambers of the heart, propelling blood to the lungs or to the rest of the body.
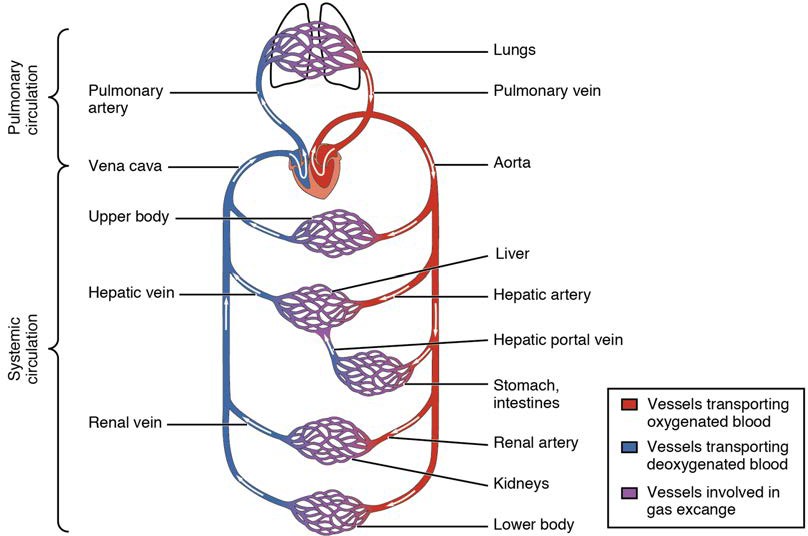
There are two distinct but linked circuits in the human circulation called the pulmonary and systemic circuits. Although both circuits transport blood and everything it carries, we can initially view the circuits from the point of view of gases. The pulmonary circuit transports blood to and from the lungs, where it picks up oxygen and delivers carbon dioxide for exhalation. The systemic circuit transports oxygenated blood to virtually all of the tissues of the body and returns relatively deoxygenated blood and carbon dioxide to the heart to be sent back to the pulmonary circulation.
INTERACTIVE VIDEO
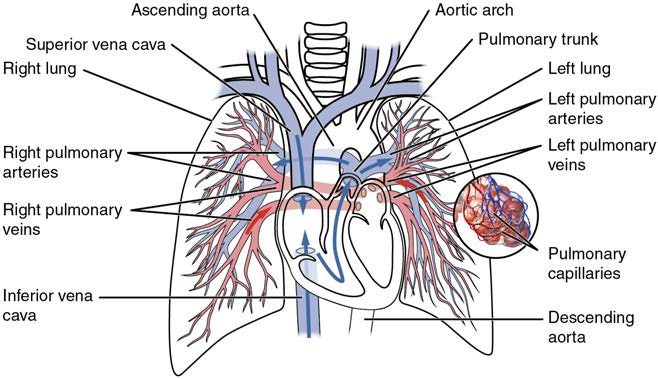
The right ventricle pumps deoxygenated blood into the pulmonary trunk, which leads toward the lungs and bifurcates into the left and right pulmonary arteries. These vessels in turn branch many times before reaching the pulmonary capillaries, where gas exchange occurs: Carbon dioxide exits the blood and oxygen enters. The pulmonary trunk and their branches are the only arteries in the post-natal body that carry relatively deoxygenated blood. Highly oxygenated blood returning from the pulmonary capillaries in the lungs passes through a series of vessels that join together to form the pulmonary veins—the only post-natal veins in the body that carry highly oxygenated blood. The pulmonary veins (typically four; two left and two right) conduct blood into the left atrium, which pumps the blood into the left ventricle, which in turn pumps oxygenated blood into the aorta and on to the many branches of the systemic circuit. Eventually, these vessels will lead to the systemic capillaries, where exchange with the tissue fluid and cells of the body occurs. In this case, oxygen and nutrients exit the systemic capillaries to be used by the cells in their metabolic processes, and carbon dioxide and waste products will enter the blood.
The blood exiting the systemic capillaries is lower in oxygen concentration than when it entered. The capillaries will ultimately unite to form venules, joining to form ever-larger veins, eventually flowing into the two major systemic veins, the superior vena cava and the inferior vena cava, which return blood to the right atrium. The superior vena cava drains blood from regions superior to the thoracic diaphragm: the head, neck, upper limbs and the thoracic region. The inferior vena cava drains blood from areas inferior to the thoracic diaphragm: the lower limbs and abdominopelvic region of the body. The blood in the superior and inferior venae cavae flows into the right atrium, which pumps blood into the right ventricle (Figure 19.4).
The great vessels of the heart is a term used to describe the major arteries and veins that carry blood directly to and from the heart. They include the superior and inferior venae cavae, ascending aorta, pulmonary trunk and pulmonary veins.
Figure 19.4 Dual System of the Human Blood Circulation Blood flows from the right atrium to the right ventricle, where it is pumped into the pulmonary circuit. The blood in the pulmonary artery branches is low in oxygen but relatively high in carbon dioxide. Gas exchange occurs in the pulmonary capillaries (oxygen into the blood, carbon dioxide out), and blood high in oxygen and low in carbon dioxide is returned to the left atrium. From here, blood enters the left ventricle, which pumps it into the systemic circuit via the aorta. Following exchange in the systemic capillaries (oxygen and nutrients out of the capillaries and carbon dioxide and wastes in), blood returns to the right atrium via the venae cavae and the cycle is repeated.
Membranes, Surface Features, and Layers
Membranes
The membrane that directly surrounds the heart and defines the pericardial cavity is called the pericardium or pericardial sac, which literally translates as “around the heart”. It also surrounds the “roots” of the major vessels, or the areas of closest proximity to the heart. The pericardial cavity is filled with lubricating serous fluid to reduce friction between the heart and pericardial sac during heart contractions.
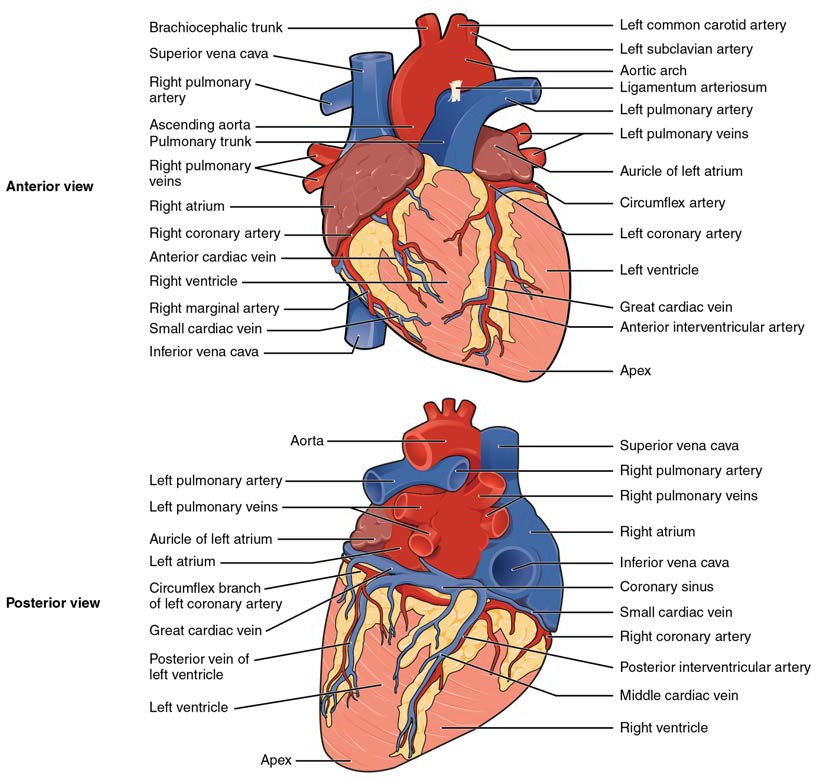
Surface Features of the Heart
Inside the pericardium, the surface features of the heart are visible, including the four chambers. There is a superficial leaf-like extension of the atria near the superior surface of the heart, one on each side, called an auricle—a name that means “ear like”—because its shape resembles the external ear of a human (Figure 19.6). Auricles are relatively thin-walled structures that can fill with blood and empty into the atria (superior chambers) of the heart. You may also hear them referred to as atrial appendages. Also prominent is a series of fat-filled grooves, each of which is known as a sulcus (plural = sulci), along the superior surfaces of the heart. Major coronary blood vessels are located in these sulci. The deep atrioventricular sulcus is located between the atria and ventricles. Located between the left and right ventricles are two additional sulci that are not as deep as the atrioventricular sulcus. The anterior interventricular sulcus is visible on the anterior surface of the heart, whereas the posterior interventricular sulcus is visible on the posterior surface of the heart. Figure 19.6 illustrates anterior and posterior views of the surface of the heart.
Figure 19.6 External Anatomy of the Heart Inside the pericardium, the surface features of the heart are visible.
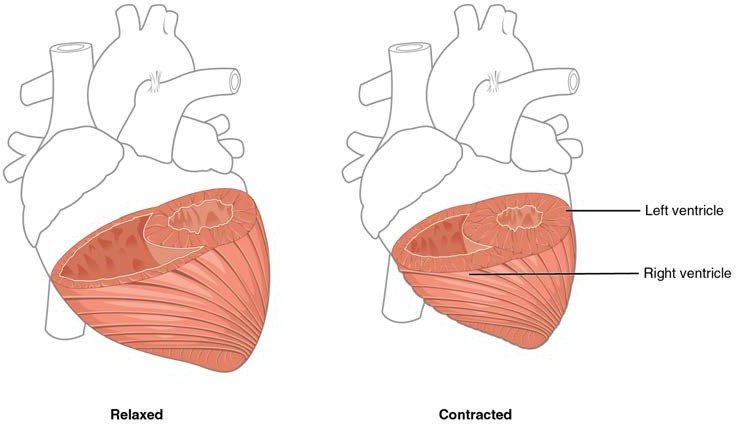
Layers
The heart is composed of multiple tissue layers; the one of most importance is the middle and thickest layer called the myocardium, made largely of cardiac muscle cells. Compared to the giant cylinders of skeletal muscle, cardiac muscle cells, or cardiomyocytes, are considerably shorter with much smaller diameters. Cardiac muscle also demonstrates striations, virtually identical to skeletal muscle. Typically, cardiomyocytes have a single, central nucleus, but two or more nuclei may be found in some cells. Cardiac muscle cells branch freely. A junction between two adjoining cells is marked by a critical structure called an intercalated disc, which helps support the synchronised contraction of the muscle. It is built upon a framework of collagenous fibres, plus the blood vessels that supply the myocardium and the nerve fibres that help regulate the heart. It is the contraction of the myocardium that pumps blood through the heart and into the major arteries. The muscle pattern is elegant and complex, as the muscle cells swirl and spiral around the chambers of the heart.
Although the ventricles on the right and left sides pump the same volume of blood per contraction, the myocardium of the left ventricle is much thicker and better developed than that of the right ventricle. In order to overcome the high resistance required to pump blood into the long systemic circuit, the left ventricle must generate a greater amount of pressure. The right ventricle does not need to generate as much pressure, since the pulmonary circuit is shorter and provides less resistance. Figure 19.8 illustrates the differences in muscular thickness needed for each of the ventricles.
Figure 19.8 Differences in Ventricular Muscle Thickness The myocardium in the left ventricle is significantly thicker than that of the right ventricle. Both ventricles pump the same volume of blood, but the left ventricle must generate a much greater pressure to overcome greater resistance in the systemic circuit. The ventricles are shown in both relaxed and contracted states. Note the differences in the relative size of the lumina, the region inside each ventricle where the blood is contained.
Internal Structure of the Heart
Septa of the Heart
Located between the two atria is the interatrial septum. Normally in an adult heart, the interatrial septum bears an oval-shaped depression known as the fossa ovalis, a remnant of an opening in the foetal heart. Between the two ventricles is a second septum known as the interventricular septum. The interventricular septum is substantially thicker than the interatrial septum, since the ventricles generate far greater pressure when they contract.
Valves of the Heart
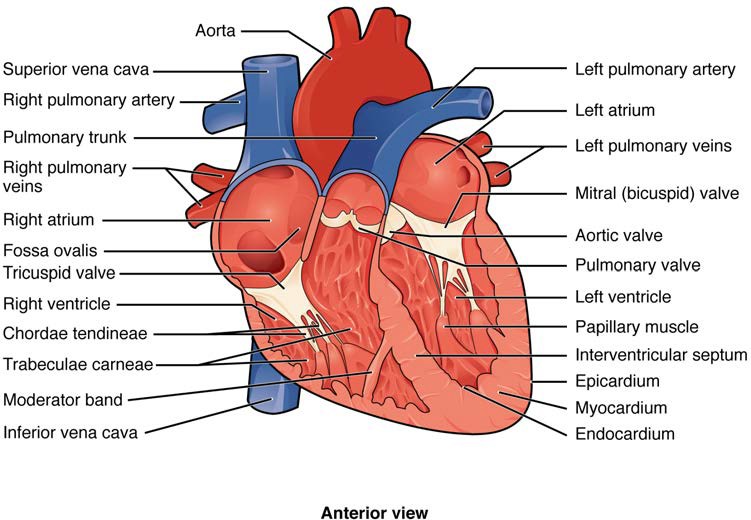
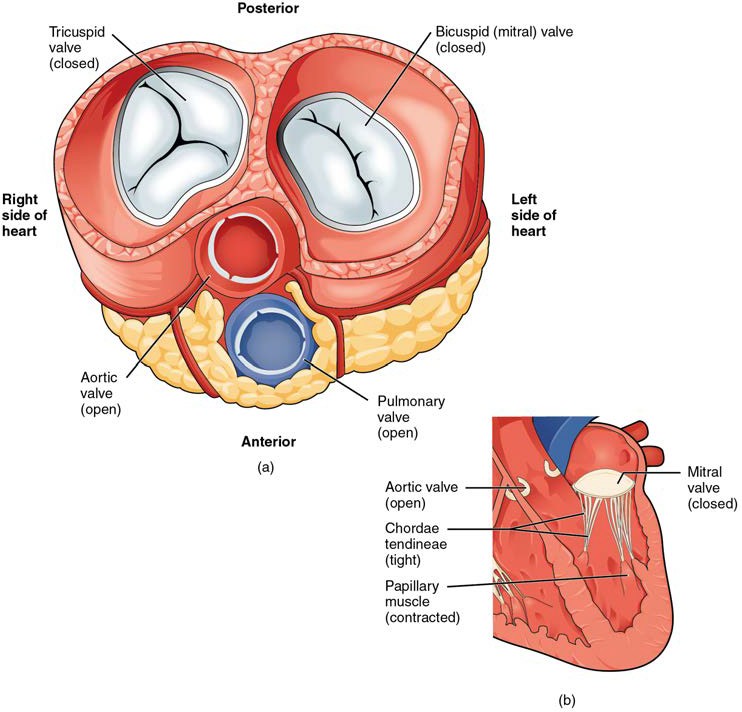
Valves ensure one-way flow of blood through the chambers of the heart and into the pulmonary and systemic circuits. The valves between the atria and ventricles are known generically as the right and left atrioventricular valves. The right atrioventricular valve is more specifically known as the tricuspid valve; and the left atrioventricular valve is more specifically known as the bicuspid or mitral valve. The valves at the openings that lead to the pulmonary trunk and ascending aorta are known as the pulmonary semilunar valve and aortic semilunar valve, respectively (Figure 19.9).
Figure 19.9 Internal Structures of the Heart This anterior view of the heart shows the four chambers, the major vessels and their early branches, as well as the valves. The presence of the pulmonary trunk and aorta covers the interatrial septum, and the atrioventricular septum is cut away to show the atrioventricular valves.
Right Atrium
The right atrium serves as the receiving chamber for blood returning to the heart from the systemic circulation. The two major systemic veins, the superior and inferior venae cavae, and the large coronary vein called the coronary sinus that drains the heart myocardium empty into the right atrium. The majority of the internal heart structures discussed in this and subsequent sections are illustrated in Figure 19.9.
While the bulk of the internal surface of the right atrium is smooth, the depression of the fossa ovalis can be seen medially on the interatrial septum, and the anterior surface demonstrates prominent ridges of muscle called the pectinate muscles. The right auricle also has pectinate muscles. The left atrium does not have pectinate muscles except in the auricle.
The atria receive venous blood on a nearly continuous basis, preventing venous flow from stopping while the ventricles are contracting. While most ventricular filling occurs passively while the atria are relaxed, they do demonstrate a contractile phase and actively pump blood into the ventricles just prior to ventricular contraction. The opening between the right atrium and right ventricle is guarded by the tricuspid valve.
Right Ventricle
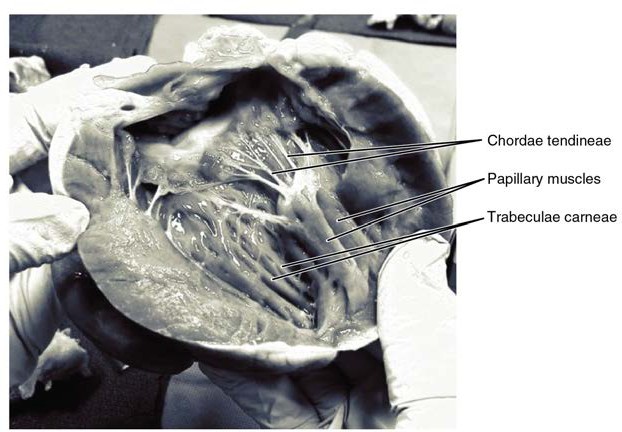
The right ventricle receives blood from the right atrium through the tricuspid valve. Each flap of the valve is attached to strong strands of connective tissue, the chordae tendineae, literally “tendinous cords,” or sometimes more poetically referred to as “heart strings”. There are several chordae tendineae associated with each of the flaps. They connect each of the valve flaps to a papillary muscle that extends from the trabeculae carneae muscles of the inferior ventricular surface. The trabeculae carneae are ridges of cardiac muscle that line the walls of the ventricle. There are three papillary muscles in the right ventricle, which correspond to the three flaps of the valves.
When the myocardium of the ventricle contracts, pressure within the ventricular chamber rises. Blood, like any fluid, flows from higher pressure to lower pressure areas, in this case, toward the pulmonary trunk and the right atrium. To prevent any potential backflow, the papillary muscles contract, generating tension on the chordae tendineae. This prevents the flaps of the valves from being forced into the atria and regurgitation of the blood back into the atria during ventricular contraction. Figure 19.10 shows papillary muscles and chordae tendineae attached to the tricuspid valve.
Figure 19.10 Chordae Tendineae and Papillary Muscles In this coronal section of the right ventricle, you can see papillary muscles attached to the tricuspid valve via chordae tendineae. (credit: modification of work by “PV KS”/flickr.com)
When the right ventricle contracts, it ejects blood into the pulmonary trunk, which branches into the left and right pulmonary arteries that carry it to each lung. The superior surface of the right ventricle begins to taper as it approaches the pulmonary trunk. At the base of the pulmonary trunk is the pulmonary semilunar valve that prevents backflow from the pulmonary trunk into the right ventricle. The semilunar valves close when blood begins to pool in their cusps following backflow of blood towards the ventricle. Therefore the semilunar valves operate through a passive non-muscular action.
Left Atrium
After exchange of gases in the pulmonary capillaries, blood returns to the left atrium high in oxygen via one of the four pulmonary veins (this is the typical configuration, however the veins vary in number between individuals). While the left atrium does not contain pectinate muscles, it does have an auricle that includes these pectinate ridges. Most blood flows passively into the heart while both the atria and ventricles are relaxed, but toward the end of the ventricular relaxation period, the left atrium will contract, pumping blood into the ventricle. This atrial contraction accounts for approximately 20 percent of ventricular filling. The opening between the left atrium and left ventricle is guarded by the mitral valve or bicuspid valve.
Left Ventricle
Recall that, although both sides of the heart will pump the same volume of blood, the myocardium is much thicker in the left ventricle compared to the right (see Figure 19.8). Like the right ventricle, the left also has trabeculae carneae. The bicuspid valve is connected to papillary muscles via chordae tendineae. There are two papillary muscles on the left as opposed to three on the right. This explains why the right atrioventricular valve is known as the tricuspid valve (for 3 papillary muscles) compared to the left atrioventricular valve which is known as the bicuspid valve (for 2 papillary muscles). The left ventricle is the major pumping chamber for the systemic circuit; it ejects blood into the ascending aorta through the aortic semilunar valve.
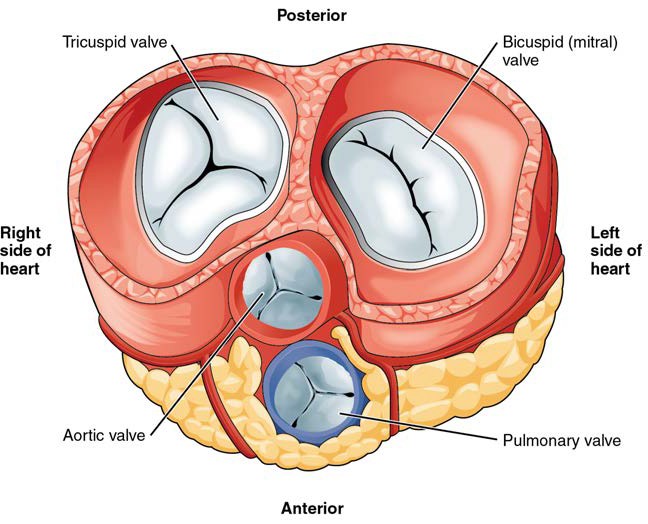
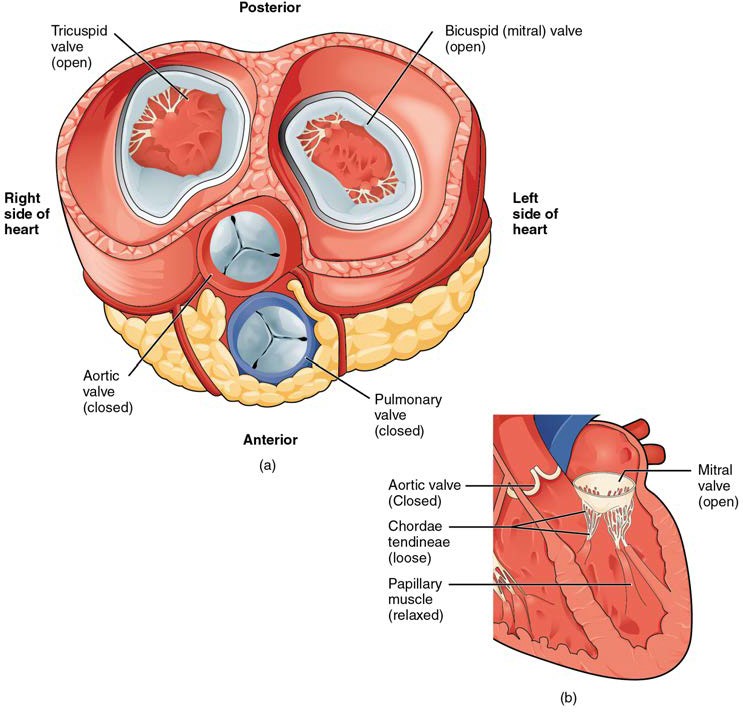
Heart Valve Structure and Function
A transverse section through the heart through the atria reveals all four heart valves along the same plane (Figure 19.11). The valves ensure unidirectional blood flow through the heart. Between the right atrium and the right ventricle is the right atrioventricular valve, or tricuspid valve. It typically consists of three flaps, or leaflets. The flaps are connected by chordae tendineae to the papillary muscles, which control the opening and closing of the valves.
Figure 19.11 Heart Valves Superior view with the atria and major vessels removed, all four valves are clearly visible.
Emerging from the right ventricle at the base of the pulmonary trunk is the pulmonary semilunar valve. The pulmonary semilunar valve is comprised of three small flaps. When the ventricle relaxes, the pressure differential causes blood to flow back into the ventricle from the pulmonary trunk. This flow of blood fills the pocket-like flaps of the pulmonary valve, causing the valve to close and producing an audible sound. Unlike the atrioventricular valves, there are no muscles or chordae tendineae associated with the pulmonary semilunar valve.
Located at the opening between the left atrium and left ventricle is the mitral valve, also called the bicuspid valve or the left atrioventricular valve. Structurally, this valve consists of two cusps, compared to the three cusps of the tricuspid valve. The two cusps of the mitral valve are attached by chordae tendineae to two papillary muscles that project from the wall of the ventricle.
At the base of the aorta is the aortic semilunar valve, which prevents backflow from the aorta. It normally is composed of three flaps. When the left ventricle relaxes and blood attempts to flow back into the left ventricle from the aorta, blood will fill the cusps of the valve, causing it to close and produces an audible sound.
In Figure 19.12a, the two atrioventricular valves are open and the two semilunar valves are closed. This occurs when both atria and ventricles are relaxed and when the atria contract to pump blood into the ventricles. Figure 19.12b shows a coronal view through the heart. Although only the left side of the heart is illustrated, the process is virtually identical on the right.
Figure 19.12 Blood Flow from the Left Atrium to the Left Ventricle (a) A transverse section through the heart illustrates the four heart valves. The two atrioventricular valves are open; the two semilunar valves are closed. (b) A coronal section through the heart illustrates blood flow through the mitral valve. When the mitral valve is open, it allows blood to move from the left atrium to the left ventricle. The aortic semilunar valve is closed to prevent backflow of blood from the aorta to the left ventricle.
Figure 19.13a shows the atrioventricular valves closed while the two semilunar valves are open. This occurs when the ventricles contract to eject blood into the pulmonary trunk and aorta. Closure of the two atrioventricular valves prevents blood from being forced back into the atria. This stage can be seen from a coronal view in Figure 19.13b.
Figure 19.13 Blood Flow from the Left Ventricle into the Great Vessels (a) A transverse section through the heart illustrates the four heart valves during ventricular contraction. The two atrioventricular valves are closed, but the two semilunar valves are open. (b) A coronal view shows the closed mitral (bicuspid) valve that prevents backflow of blood into the left atrium. The aortic semilunar valve is open to allow blood to be ejected into the aorta.
When the ventricles begin to contract, pressure within the ventricles rises and blood flows toward the area of lowest pressure, which is initially in the atria. This backflow causes the cusps of the tricuspid and mitral (bicuspid) valves to close. These valves are tied down to the papillary muscles by chordae tendineae. During the relaxation phase of the cardiac cycle, the papillary muscles are also relaxed and the tension on the chordae tendineae is slight (see Figure 19.12b). However, as the myocardium of the ventricle contracts, so do the papillary muscles. This creates tension on the chordae tendineae (see Figure 19.13b), helping to hold the cusps of the atrioventricular valves in place and preventing them from being blown back into the atria.
The aortic and pulmonary semilunar valves lack the chordae tendineae and papillary muscles associated with the atrioventricular valves. Instead, they consist of pocket-like folds of endocardium reinforced with additional connective tissue. When the ventricles relax and the change in pressure forces the blood toward the ventricles, the blood presses against these cusps and seals the openings.
INTERACTIVE ACTIVITY
Now review photos of the heart plastic model from anterior and posterior views by clicking the arrows beside each image, or the buttons below the image panel. Identify both internal and external features of the heart in each photo. Test your knowledge on the unlabelled photos before revealing the names of the main features in the labelled photo. [Created in Anatomy.TV, Primal Pictures]
Questions:
(a) Do the atrioventricular valves open or close when the papillary muscles contract?
(b) Which chamber of the heart has the thickest myocardium? Explain why.
Structure and Function of Blood Vessels
Learning Objectives
By the end of this section, you will be able to:
- Compare and contrast the three tunics that make up the walls of most blood vessels
- Distinguish between elastic arteries, muscular arteries, and arterioles on the basis of structure, location, and function
- Describe the basic structure of a capillary bed, from the supplying metarteriole to the venule into which it drains
- Explain the structure and function of venous valves in the large veins of the extremities
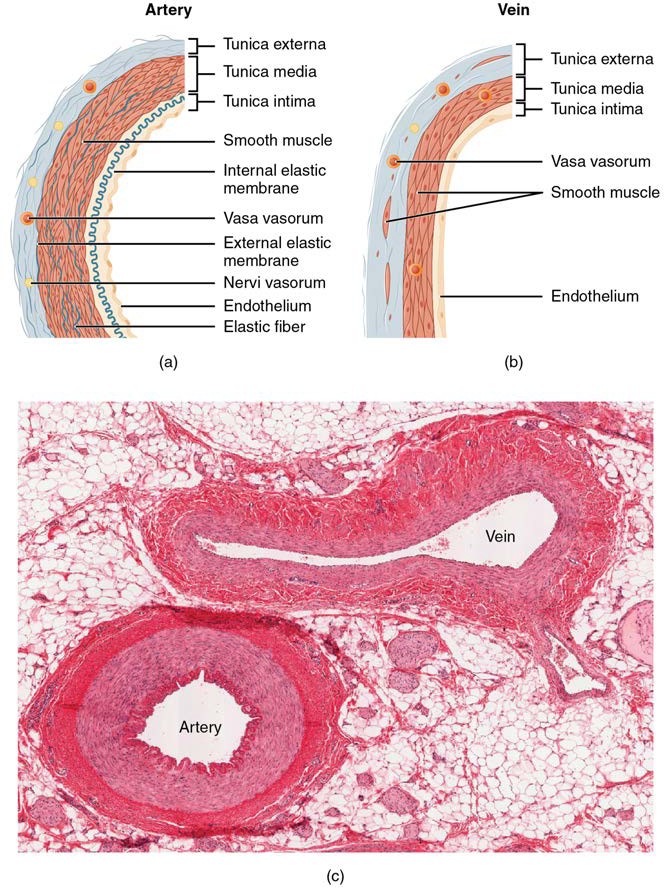
Blood is carried through the body via blood vessels. An artery is a blood vessel that carries blood away from the heart, where it branches into ever-smaller vessels. Eventually, the smallest arteries, vessels called arterioles, further branch into tiny capillaries, where nutrients and wastes are exchanged, and then combine with other vessels that exit capillaries to form venules, small blood vessels that carry blood to a vein, a larger blood vessel that returns blood to the heart.
Arteries and veins transport blood in two distinct circuits: the systemic circuit and the pulmonary circuit (Figure 20.2). Systemic arteries provide blood rich in oxygen to the body’s tissues. The blood returned to the heart through systemic veins has less oxygen, since much of the oxygen carried by the arteries has been delivered to the cells. In contrast, in the pulmonary circuit, arteries carry blood low in oxygen exclusively to the lungs for gas exchange. Pulmonary veins then return freshly oxygenated blood from the lungs to the heart to be pumped back out into systemic circulation. Although arteries and veins differ structurally and functionally, they share certain features.
Figure 20.2 Cardiovascular Circulation The pulmonary circuit moves blood from the right side of the heart to the lungs and back to the heart. The systemic circuit moves blood from the left side of the heart to the head and body and returns it to the right side of the heart to repeat the cycle. The arrows indicate the direction of blood flow, and the colours show the relative levels of oxygen concentration.
Blood Vessel Wall
Different types of blood vessels vary slightly in their structures, but they share the same general features. Arteries and arterioles have thicker walls than veins and venules because they are closer to the heart and receive blood that is surging at a far greater pressure (Figure 20.3). Each type of vessel has a lumen—a hollow passageway through which blood flows. Arteries have smaller lumina than veins, a characteristic that helps to maintain the pressure of blood moving through the system. Together, their thicker walls and smaller diameters give arterial lumina a more rounded appearance in cross section than the lumina of veins.
Figure 20.3 Structure of Blood Vessels (a) Arteries and (b) Veins share the same general features, but the walls of arteries are much thicker because of the higher pressure of the blood that flows through them. (c) Muscular or medium sized artery and companion vein. [Michigan Histology and Virtual Microscopy Learning Resources]
By the time blood has passed through capillaries and entered venules, the pressure initially exerted upon it by heart contractions has diminished. In other words, in comparison to arteries, venules and veins withstand a much lower pressure from the blood that flows through them. Their walls are considerably thinner and their lumina are correspondingly larger in diameter, allowing more blood to flow with less vessel resistance. In addition, many veins of the body, particularly those of the limbs, contain valves that assist the unidirectional flow of blood toward the heart. This is critical because blood flow becomes sluggish in the extremities, as a result of the lower pressure and the effects of gravity.
Both arteries and veins have the same three distinct tissue layers, called tunics (from the Latin term tunica, for the garments first worn by ancient Romans). From the most interior layer to the most external, these tunics are the tunica intima, the tunica media, and the tunica adventitia (see Figure 20.3). Table 20.1 compares and contrasts the tunics of the arteries and veins.
Table 20.1 Comparison of Tunics in Arteries and Veins
| Arteries | Veins | |
| General appearance | Thick walls with small lumens Generally appear rounded |
Thin walls with large lumens Generally appear flattened |
| Tunica intima | Endothelium usually appears wavy due to constriction of smooth muscle Internal elastic membrane present in larger vessels |
Endothelium appears smooth Internal elastic membrane absent |
| Tunica media | Normally the thickest layer in arteries Smooth muscle cells and elastic fibres predominate (the proportions of these vary with distance from the heart) External elastic membrane present in larger vessels |
Normally thinner than the tunica externa Smooth muscle cells and collagenous fibres predominate Nerves and vasa vasorum present External elastic membrane absent |
| Tunica externa | Normally thinner than the tunica media in all but the largest arteries Collagenous and elastic fibres Nerves and vasa vasorum present |
Normally the thickest layer in veins Collagenous and smooth fibres predominate Some smooth muscle fibers Nerves and vasa vasorum present |
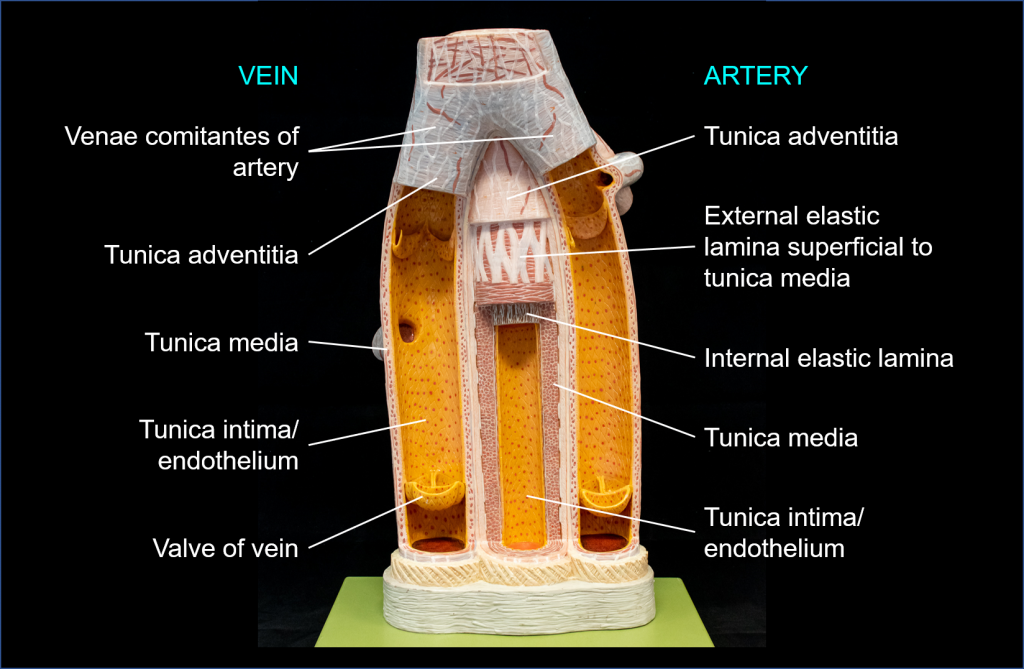
Figure 20.3 Blood vessel model This model represents the relationship between an artery and deep veins in the distal parts of the upper or lower limbs. Note the pairing of veins that accompany the artery (venae comitantes relationship). Both arteries and veins consist of the same three tunics: tunica intima, tunica media and tunica adventitia. Note the position and different thickness of these tunics in the artery and vein of this model.
Arteries
An artery is a blood vessel that conducts blood away from the heart. All arteries have relatively thick walls that can withstand the high pressure of blood ejected from the heart. However, those close to the heart have the thickest walls, containing a high percentage of elastic fibres in all three of their tunics. This type of artery is known as an elastic artery (Figure 20.4). Vessels larger than 10 mm in diameter are typically elastic. Their abundant elastic fibres allow them to expand, as blood pumped from the ventricles passes through them, and then to recoil after the surge has passed. If artery walls were rigid and unable to expand and recoil, their resistance to blood flow would greatly increase and blood pressure would rise to even higher levels, which would in turn require the heart to pump harder to increase the volume of blood expelled by each pump and maintain adequate pressure and flow. Artery walls would have to become even thicker in response to this increased pressure. The elastic recoil of the vascular wall helps to maintain the pressure gradient that drives the blood through the arterial system.
Farther from the heart, where the surge of blood has dampened, the percentage of elastic fibres in an artery’s tunica intima decreases and the amount of smooth muscle in its tunica media increases. The artery at this point is described as a muscular artery. The diameter of muscular arteries typically ranges from 0.1 mm to 10 mm. Their thick tunica media allows muscular arteries to play a leading role in vasoconstriction. In contrast, their decreased quantity of elastic fibres limits their ability to expand. Fortunately, because the blood pressure has eased by the time it reaches these more distant vessels, elasticity has become less important.
Notice that although the distinctions between elastic and muscular arteries are important, there is no “line of demarcation” where an elastic artery suddenly becomes muscular. Rather, there is a gradual transition as the vascular tree repeatedly branches. In turn, muscular arteries branch to distribute blood to the vast network of arterioles. For this reason, a muscular artery is also known as a distributing artery.
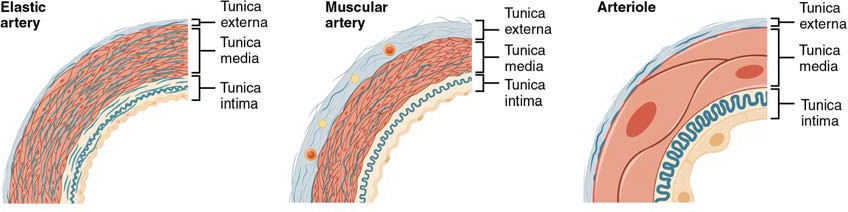
Figure 20.4 Types of Arteries and Arterioles Comparison of the walls of an elastic artery, a muscular artery, and an arteriole is shown. In terms of scale, the diameter of an arteriole is measured in micrometers compared to millimeters for elastic and muscular arteries.
Arterioles
An arteriole is a very small artery that leads to a capillary. Arterioles have the same three tunics as the larger vessels, but the thickness of each is greatly diminished. The critical endothelial lining of the tunica intima is intact. The tunica media is restricted to one or two smooth muscle cell layers in thickness. The tunica externa remains but is very thin (see Figure 20.4). With a lumen averaging 30 micrometers or less in diameter, arterioles are critical in slowing down—or resisting—blood flow and, thus, causing a substantial drop in blood pressure. Because of this, you may see them referred to as resistance vessels.
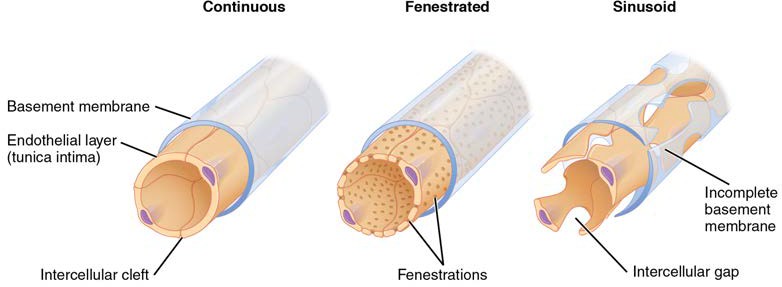
Capillaries
A capillary is a microscopic channel that supplies blood to the tissues themselves, a process called perfusion. Exchange of gases and other substances occurs in the capillaries between the blood and the surrounding cells and their tissue fluid (interstitial fluid). The diameter of a capillary lumen ranges from 5–10 micrometers; the smallest are just barely wide enough for an erythrocyte to squeeze through.
The wall of a capillary consists of the endothelial layer surrounded by a basement membrane with occasional smooth muscle fibres. There is some variation in wall structure: In a large capillary, several endothelial cells bordering each other may line the lumen; in a small capillary, there may be only a single cell layer that wraps around to contact itself.
For capillaries to function, their walls must be leaky, allowing substances to pass through. There are three major types of capillaries, which differ according to their degree of “leakiness:” continuous, fenestrated and sinusoidal capillaries (Figure 20.5).
Figure 20.5 Types of Capillaries The three major types of capillaries: continuous, fenestrated, and sinusoidal.
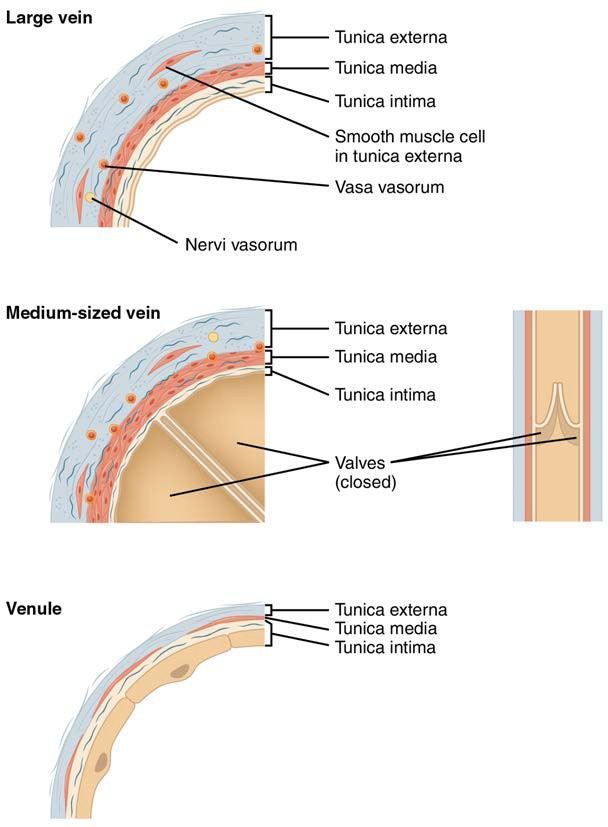
Veins
A venule is an extremely small vein, generally 8–100 micrometers in diameter. Postcapillary venules join multiple capillaries exiting from a capillary bed. Multiple venules join to form veins. The walls of venules consist of endothelium, a thin middle layer with a few muscle cells and elastic fibers, plus an outer layer of connective tissue fibers that constitute a very thin tunica adventitia (Figure 20.7). Venules as well as capillaries are the primary sites for leucocyte migration from the blood into the tissues. They do this by squeezing through adjacent endothelial cells to enter the tissue fluid.
A vein is a blood vessel that conducts blood toward the heart. Compared to arteries, veins are thin-walled vessels with large and irregular lumina (see Figure 20.7). Because they are low-pressure vessels, larger veins are commonly equipped with valves that promote the unidirectional flow of blood toward the heart and prevent backflow toward the capillaries caused by the inherent low blood pressure in veins as well as the pull of gravity. Table 20.2 compares the features of arteries and veins.
Figure 20.7 Comparison of Veins and Venules Many veins have valves to prevent backflow of blood, whereas venules do not. In terms of scale, the diameter of a venule is measured in micrometers compared to millimeters for veins.
Table 20.2 Comparison of Arteries and Veins
| Arteries | Veins | |
| Direction of blood flow | Conducts blood away from the heart | Conducts blood toward the heart |
| General appearance | Rounded | Irregular, often collapsed |
| Pressure | High | Low |
| Wall thickness | Thick | Thin |
| Relative oxygen concentration | Higher in systemic arteries. Lower in pulmonary arteries | Lower in systemic veins. Higher in pulmonary veins |
| Valves | Not present | Present most commonly in limbs and in veins inferior to the heart |
Blood vessels of the Pulmonary and Systemic Circulations
Learning Objectives
By the end of this section, you will be able to:
- Identify the vessels through which blood travels within the pulmonary circuit, beginning from the right ventricle of the heart and ending at the left atrium
- Create a flow chart showing the major systemic arteries through which blood travels from the aorta and its major branches, to the most significant arteries feeding into the right and left upper and lower limbs
- Create a flow chart showing the major systemic veins through which blood travels from the feet to the right atrium of the heart
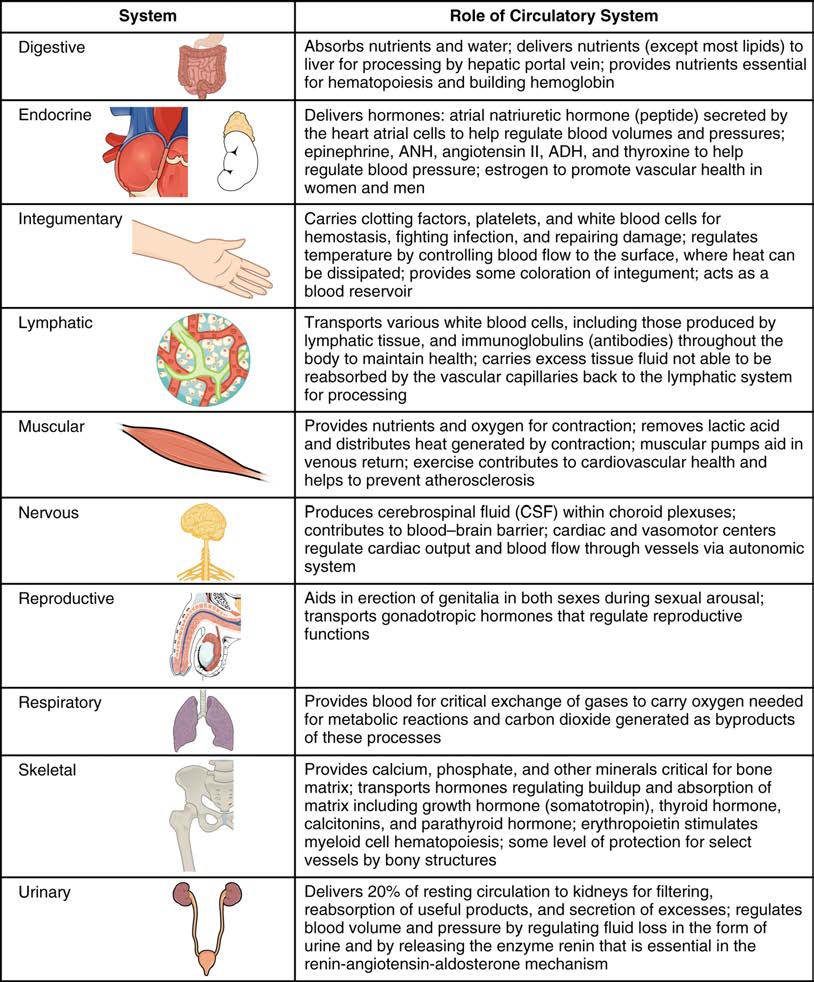
Virtually every cell, tissue, organ, and system in the body is impacted by the circulatory system. This includes the generalised and more specialised functions of transport of materials, capillary exchange, maintaining health by transporting white blood cells and various immunoglobulins (antibodies), hemostasis, regulation of body temperature, and helping to maintain acid-base balance. In addition to these shared functions, many systems enjoy a unique relationship with the circulatory system. Figure 20.22 summarises these relationships.
Figure 20.22 Interaction of the Circulatory System with Other Body Systems
As you learn about the vessels of the systemic and pulmonary circuits, notice that many arteries and veins share the same names, parallel one another throughout the body, and are very similar on the right and left sides of the body. These pairs of vessels will be traced through only one side of the body. Where differences occur in branching patterns or when vessels are singular, this will be indicated. For example, you will find a pair of femoral arteries and a pair of femoral veins, with one vessel on each side of the body. In contrast, some vessels closer to the midline of the body, such as the aorta, are unique. Moreover, some superficial veins, such as the great saphenous vein in the femoral region, have no arterial counterpart. Another phenomenon that can make the study of vessels challenging is that names of vessels can change with location. Like a street that changes name as it passes through an intersection, an artery or vein can change names as it passes an anatomical landmark. For example, the left subclavian artery becomes the axillary artery as it passes through the body wall and into the axillary region, and then becomes the brachial artery as it flows from the axillary region into the brachium.
A blood vessel can be described based on its direction of blood flow and how it connects with other blood vessels. The origin of a blood vessel is the point where blood first enters the blood vessel. The termination of a blood vessel is where blood leaves the named blood vessel. Arteries can have many branches, of which there are two main categories: collateral branches which arise from the side of the main blood vessel; and terminal branches where the named blood vessel ends and branches into two or more other vessels. As blood is flowing into veins, we describe vessels that join a main vein tributaries and where a vein forms from multiple smaller veins, this is called a confluence. In the case where a blood vessel changes names as it passes a landmark, this is known as a ‘continuation‘ of the vessel. We will be using these terms throughout this section to describe the anatomy of the major blood vessels of the body.
Pulmonary Circulation
Recall that blood returning from the systemic circuit enters the right atrium (Figure 20.23) via the superior and inferior venae cavae and the coronary sinus, which drains the blood of the myocardium of the heart. These vessels will be described more fully later in this section. This blood is relatively low in oxygen and relatively high in carbon dioxide, since much of the oxygen has been extracted for use by the tissues and the waste gas carbon dioxide was picked up to be transported to the lungs for elimination. From the right atrium, blood moves into the right ventricle, which pumps it to the lungs for gas exchange. This system of vessels is referred to as the pulmonary circuit.
The single vessel exiting the right ventricle is the pulmonary trunk. At the base of the pulmonary trunk is the pulmonary semilunar valve, which prevents backflow of blood into the right ventricle during ventricular diastole. As the pulmonary trunk reaches the superior surface of the heart, it curves posteriorly and terminally branches into a left and a right pulmonary artery. To prevent confusion between these vessels, it is important to refer to the vessel exiting the heart as the pulmonary trunk, rather than also calling it a pulmonary artery. The pulmonary arteries in turn branch many times within the lung, forming a series of smaller arteries and arterioles that eventually lead to the pulmonary capillaries. The pulmonary capillaries surround lung structures known as alveoli that are the sites of oxygen and carbon dioxide exchange.
Once gas exchange is completed, oxygenated blood flows from the pulmonary capillaries into a series of pulmonary venules that eventually lead to a series of larger pulmonary veins. Typically four pulmonary veins, two on the left and two on the right, return blood to the left atrium. At this point, the pulmonary circuit is complete. Table 20.4 defines the major arteries and veins of the pulmonary circuit discussed in the text.
Figure 20.23 Pulmonary Circuit Blood exiting from the right ventricle flows into the pulmonary trunk, which bifurcates into the two pulmonary arteries. These vessels branch to supply blood to the pulmonary capillaries, where gas exchange occurs within the lung alveoli. Blood returns via the pulmonary veins to the left atrium.
Table 20.4 Pulmonary Arteries and Veins
| Vessel | Description |
| Pulmonary trunk | Single large vessel exiting the right ventricle that divides to form the right and left pulmonary arteries |
| Pulmonary arteries | Left and right vessels that form from the pulmonary trunk and lead to smaller arterioles and eventually to the pulmonary capillaries |
| Pulmonary veins | Typically two sets of paired vessels—one pair on each side—that are formed from the small venules, leading away from the pulmonary capillaries to flow into the left atrium |
Overview of Systemic Arteries
Blood relatively high in oxygen concentration is returned from the pulmonary circuit to the left atrium via the pulmonary veins. From the left atrium, blood moves into the left ventricle, which pumps blood into the aorta. The aorta and its branches—the systemic arteries—send blood to virtually every organ of the body in the systemic circulation (Figure 20.24).
The Aorta
The aorta is the largest artery in the body (Figure 20.25). The aorta consists of the ascending aorta, the aortic arch, and the descending aorta, which passes through the thoracic diaphragm, a landmark that divides into the descending aorta into the superior thoracic and inferior abdominal parts. At the base of the aorta is the aortic semilunar valve that prevents backflow of blood into the left ventricle while the heart is relaxing. After exiting the heart, the ascending aorta moves in a superior direction for approximately 5 cm and ends at the sternal angle. Following this ascent, it reverses direction, forming a graceful arc to the left, and changes names to the aortic arch. The aortic arch descends toward the inferior portions of the body and terminates at the level of the intervertebral disk between the fourth and fifth thoracic vertebrae. Beyond this point, the descending aorta continues close to the bodies of the vertebrae and passes through an opening in the thoracic diaphragm known as the aortic hiatus. Superior to the thoracic diaphragm, the aorta is called the thoracic aorta, and inferior to the thoracic diaphragm, it is called the abdominal aorta. The abdominal aorta terminates when it terminally branches into the two common iliac arteries at the level of the fourth lumbar vertebra.
See Figure 20.25 for an illustration of the ascending aorta, the aortic arch, and the initial segment of the descending aorta plus major branches; Table 20.5 summarises the structures of the aorta.
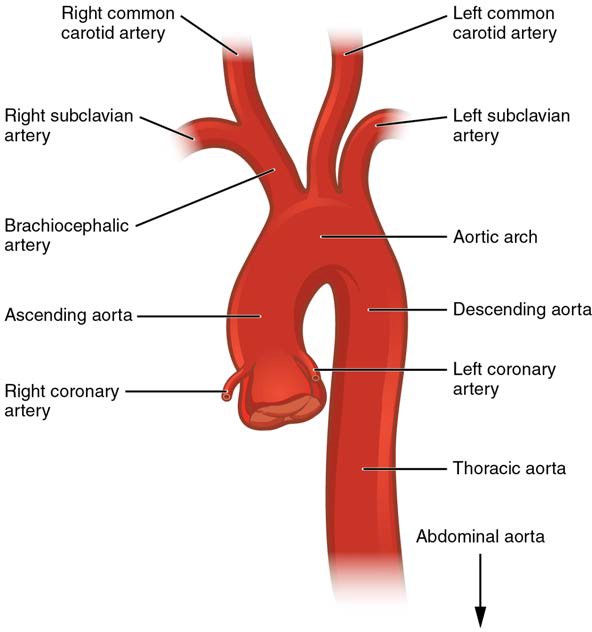
Figure 20.25 Aorta The aorta has distinct regions, including the ascending aorta, aortic arch, and the descending aorta, which includes the thoracic and abdominal regions.
Table 20.5 Components of the Aorta
| Vessel | Description |
| Aorta | Largest artery in the body, originating from the left ventricle and descending to the abdominal region, where it terminally branches into the common iliac arteries; arteries originating from the aorta distribute blood to virtually all tissues of the body |
| Ascending aorta | Proximal portion of the aorta, rising superiorly from the left ventricle for a distance of approximately 5 cm |
| Aortic arch | Graceful arc to the left that connects the ascending aorta to the descending aorta |
| Descending aorta | Portion of the aorta that continues inferiorly past the end of the aortic arch; subdivided into the thoracic aorta and the abdominal aorta by the thoracic diaphragm |
| Thoracic aorta | Portion of the descending aorta superior to the aortic hiatus of the thoracic diaphragm |
| Abdominal aorta | Portion of the aorta inferior to the aortic hiatus and superior to the common iliac arteries |
INTERACTIVE ACTIVITY
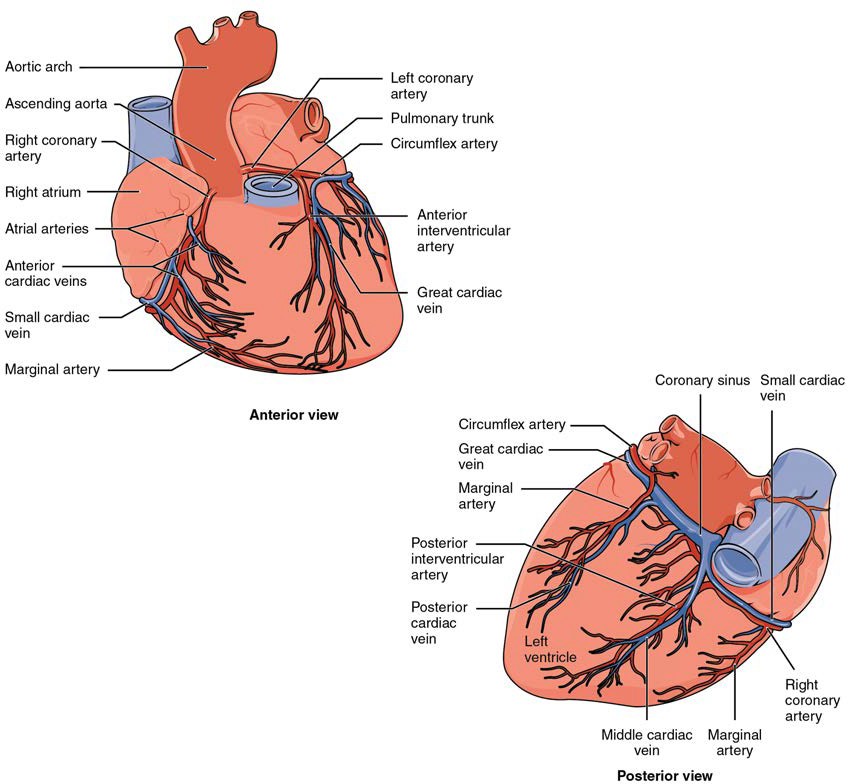
Coronary Circulation
Coronary arteries supply blood to the myocardium and other components of the heart. The first vessels that branch from the ascending aorta as collateral branches are the paired coronary arteries (see Figure 20.25), which arise just superior to the aortic semilunar valve. The right and left coronary arteries encircle the heart, forming a ring-like structure that divides into the next level of branches that supplies blood to the heart tissues. The left coronary artery distributes blood to the left side of the heart, the left atrium and ventricle, and the interventricular septum. The circumflex artery arises from the left coronary artery and follows the left atrioventricular sulcus. The larger anterior interventricular artery, also known as the left anterior descending artery (LAD), is the second major branch arising from the left coronary artery.
The right coronary artery proceeds along the right atrioventricular sulcus and distributes blood to the right atrium and portions of both ventricles. Normally, one or more marginal arteries arise from the right coronary artery inferior to the right atrium. On the posterior surface of the heart, the right coronary artery gives rise to the posterior interventricular artery, also known as the posterior descending artery. A number of connections may exist between and within the branches of the right and left coronary arteries, known as anastomoses. An anastomosis is an area where vessels unite to form interconnections that normally allow blood to circulate to a region even if there may be partial blockage in another branch. The anastomoses in the heart are very small. Therefore, this ability is somewhat restricted in the heart so a coronary artery blockage often results in death of the cells (myocardial infarction) supplied by the particular vessel. Cardiac veins drain the heart and generally parallel the large surface arteries. Figure 19.14 presents views of the coronary circulation from both the anterior and posterior views.
Figure 19.14 Coronary Circulation The anterior and posterior views of the heart show the course of prominent coronary arteries and their branches.
Aortic Arch Branches
There are three major collateral branches of the aortic arch: the brachiocephalic trunk, the left common carotid artery, and the left subclavian (literally “under the clavicle”) artery. As you would expect based upon proximity to the heart, each of these vessels is classified as an elastic artery. The brachiocephalic trunk is located only on the right side of the body; there is no corresponding artery on the left. The brachiocephalic trunk terminally branches into the right subclavian artery and the right common carotid artery. The left subclavian and left common carotid arteries arise independently from the aortic arch (as collateral branches) but otherwise follow a similar pattern and distribution to the corresponding arteries on the right side (see Figure 20.25).
Each subclavian artery supplies blood to the upper limb, thorax, shoulders, back, and central nervous system. An important branch of the subclavian artery is the vertebral artery, which passes through the vertebral foramen in the cervical vertebrae and then through the foramen magnum into the cranial cavity to supply blood to the brain and spinal cord. The paired vertebral arteries join together to form the large basilar artery at the base of the medulla oblongata.
The common carotid artery terminally branches into internal and external carotid arteries (see Figure 20.26). The right common carotid artery arises from the brachiocephalic trunk and the left common carotid artery arises directly from the aortic arch. The external carotid artery supplies blood to numerous structures within the face, lower jaw, neck, oesophagus and larynx. The internal carotid artery initially forms an expansion known as the carotid sinus, containing the carotid baroreceptors and chemoreceptors. The information provided by these receptors is critical to maintaining cardiovascular homeostasis.
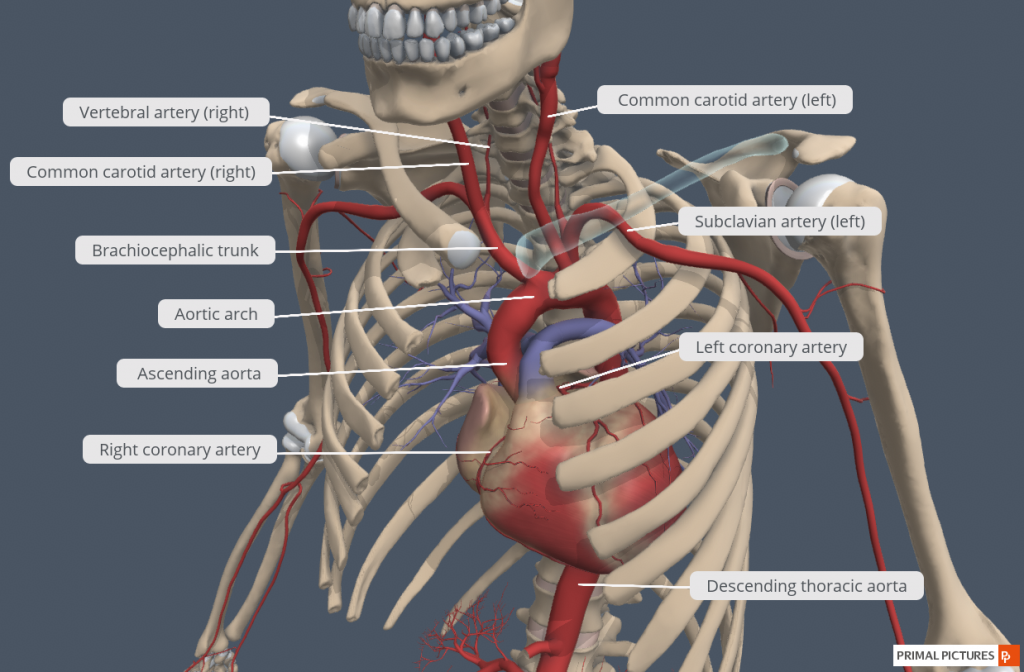
Figure XX Branches of the Aortic Arch in situ Note the relationship between the position of the heart, ascending aorta, aortic arch and descending aorta relative to the vertebral column and thoracic cage (note the sternum and costal cartilages have been removed to visualise these cardiovascular structures). The branches of the aortic arch display asymmetry between the right and left sides, where the right common carotid and right subclavian arteries arise from the brachiocephalic trunk in contrast to the left common carotid and left subclavian arteries which arise as direct collateral branches from the aortic arch. [Created in Anatomy.TV, Primal Pictures]
INTERACTIVE ACTIVITY
The common carotid artery gives rise to the external and internal carotid arteries. The external carotid artery remains superficial and gives rise to many arteries of the head [1st panel]. Both the internal carotid and vertebral arteries are responsible for the blood supply of the brain [2nd panel]. [Created in Anatomy.TV, Primal Pictures]
(a) Describe the course of the internal carotid artery into the cranial cavity (ie. name the bone and feature it passes through).
(b) Observe the course of the vertebral artery to explain why it has this name, and name the large space it passes through to enter the cranial cavity.
Table 20.6 Aortic Arch Branches and Brain Circulation
| Vessel | Description |
| Brachiocephalic trunk | Single vessel located on the right side of the body; the first vessel branching from the aortic arch; gives rise to the right subclavian artery and the right common carotid artery; supplies blood to the head, neck, upper limb and wall of the thoracic region |
| Subclavian artery | The right subclavian artery arises from the brachiocephalic trunk while the left subclavian artery arises from the aortic arch; gives rise to the vertebral artery; supplies blood to the upper limb, thorax, shoulders, back and central nervous system |
| Vertebral artery | Arises from the subclavian artery and passes through the vertebral foramen through the foramen magnum to the brain; joins with the internal carotid artery to form the cerebral arterial circle; supplies blood to the brain and spinal cord |
| Common carotid artery | The right common carotid artery arises from the brachiocephalic trunk and the left common carotid artery arises from the aortic arch; each gives rise to the external and internal carotid arteries; supplies the head and neck |
| External carotid artery | Arises from the common carotid artery; supplies blood to numerous structures within the face, lower jaw, neck, oesophagus and larynx |
| Internal carotid artery | Arises from the common carotid artery and begins with the carotid sinus; goes through the carotid canal of the temporal bone to the base of the brain; combines with the branches of the vertebral artery, forming the cerebral arterial circle; supplies blood to the brain |
INTERACTIVE ACTIVITY
Review photos of the plastic models displaying the blood vessels of the head and neck by clicking the arrows beside each image, or the buttons below the image panel. Identify both internal and external features of the heart in each photo. Test your knowledge on the unlabelled photos before revealing the names of the main features in the labelled photo. [Created in Anatomy.TV, Primal Pictures]
Question:
(a) Describe the origin of the vertebral artery
(b) Describe the origin of the internal carotid artery
Abdominal Aorta and Major Branches
After crossing through the thoracic diaphragm at the aortic hiatus, the descending aorta is called the abdominal aorta (see Figure 20.28). This vessel remains to the left of the vertebral column and is embedded in adipose tissue posterior to the peritoneal cavity in the retroperitoneal compartment. The abdominal aorta gives rise to several important branches. A single coeliac trunk emerges and divides into the left gastric artery to supply blood to the stomach and oesophagus, the splenic artery to supply blood to the spleen, and the common hepatic artery that supplies blood to the liver as well as several other supracolic organs. Two additional single vessels arise from the abdominal aorta. These are the superior and inferior mesenteric arteries. The superior mesenteric artery arises approximately 2.5 cm inferior to the coeliac trunk and branches into several major vessels that supply blood to the small intestine (duodenum, jejunum, and ileum), the pancreas and a majority of the large intestine. The inferior mesenteric artery supplies blood to the distal segment of the large intestine, including the rectum. It arises approximately 5 cm superior to the common iliac arteries.
In addition to these single branches, the abdominal aorta gives rise to several significant paired arteries along the way. These include the renal arteries and the gonadal arteries. Each renal artery branches approximately 2.5 cm inferior to the superior mesenteric arteries and supplies a kidney. Each gonadal artery supplies blood to the gonads, or reproductive organs, and is described as either an ovarian artery or a testicular artery, depending upon the sex of the individual. An ovarian artery supplies blood to an ovary, uterine tube and the uterus, and is located within the suspensory ligament of the uterus. It is considerably shorter than a testicular artery, which ultimately travels outside the body cavity to the testes, forming one component of the spermatic cord. The gonadal arteries arise inferior to the renal arteries and are generally retroperitoneal.
The aorta divides at approximately the level of vertebra L4 into a left and a right common iliac artery. The common iliac arteries provide blood to the pelvic region and ultimately to the lower limbs. They split into external and internal iliac arteries approximately at the level of the lumbar-sacral articulation. Each internal iliac artery sends branches to the urinary bladder, the walls of the pelvis, the external genitalia and the medial portion of the femoral region. In females, they also provide blood to the uterus and vagina. The much larger external iliac artery supplies blood to each of the lower limbs. Figure 20.29 shows the distribution of the major branches of the aorta into the thoracic and abdominal regions. Table 20.8 summarises the major branches of the abdominal aorta.
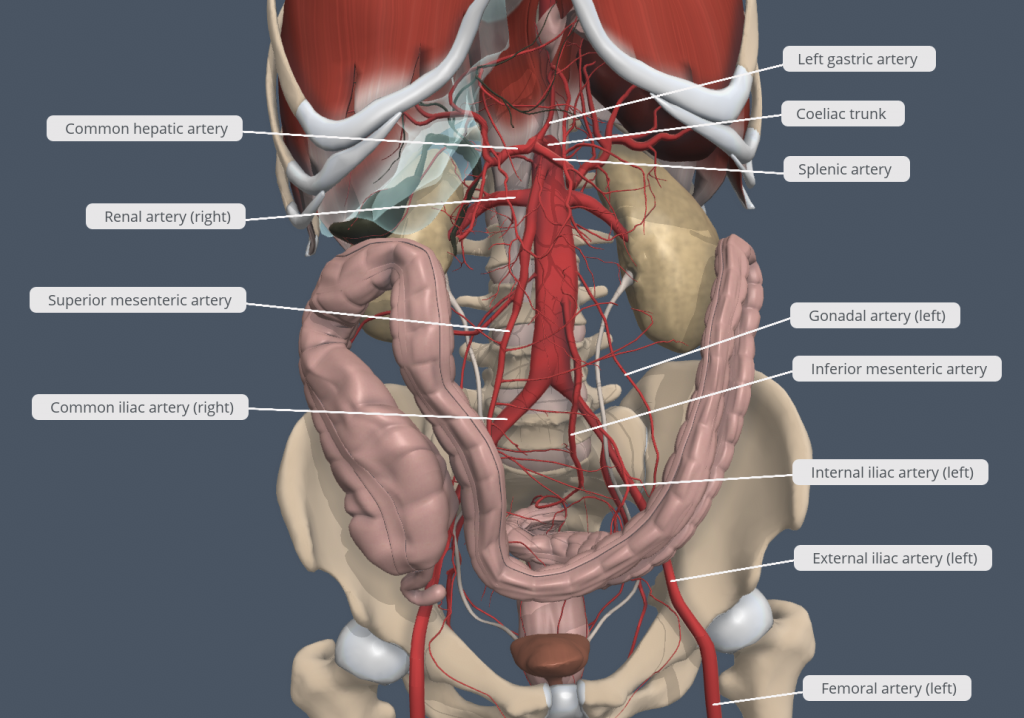
Figure XX: Major branches of Abdominal Aorta Three single collateral branches arise from the abdominal aorta: coeliac trunk, superior mesenteric artery and inferior mesenteric artery; and two paired collateral branches arise from the abdominal aorta: renal arteries and gonadal arteries. The abdominal aorta terminally branches into the right and left common iliac arteries which provide blood supply to the pelvis and lower limb. [Created in Anatomy.TV, Primal Pictures]
Table 20.8 Vessels of the Abdominal Aorta
| Vessel | Description |
| Coeliac trunk | A major branch of the abdominal aorta; gives rise to the left gastric artery, the splenic artery, and the common hepatic artery |
| Left gastric artery | Branch of the coeliac trunk; supplies blood to the stomach |
| Splenic artery | Branch of the coeliac trunk; supplies blood to the spleen |
| Common hepatic artery | Branch of the coeliac trunk that blood to the liver, stomach, gallbladder, duodenum and pancreas |
| Superior mesenteric artery | Branch of the abdominal aorta; supplies blood to the small intestine (duodenum, jejunum, and ileum), the pancreas, and a majority of the large intestine |
| Inferior mesenteric artery | Branch of the abdominal aorta; supplies blood to the distal segment of the large intestine including the rectum |
| Renal artery | Branch of the abdominal aorta; supplies each kidney |
| Gonadal artery | Branch of the abdominal aorta; supplies blood to the gonads or reproductive organs; also described as ovarian arteries or testicular arteries, depending upon the sex of the individual |
| Ovarian artery | Branch of the abdominal aorta; supplies blood to ovary, uterine tube and uterus |
| Testicular artery | Branch of the abdominal aorta; ultimately travels outside the body cavity to the testes and forms one component of the spermatic cord |
| Common iliac artery | Branch of the aorta that leads to the internal and external iliac arteries |
| Internal iliac artery | Branch from the common iliac arteries; supplies blood to the urinary bladder, walls of the pelvis, external genitalia and the medial portion of the femoral region; in females, also provides blood to the uterus and vagina |
| External iliac artery | Branch of the common iliac artery that leaves the body cavity and becomes a femoral artery; supplies blood to the lower limbs |
Arteries Serving the Upper Limbs
As the subclavian artery exits the thorax into the axillary region, it is renamed the axillary artery. Although it does branch and supply blood to the region near the head of the humerus, the majority of the vessel continues into the brachium and becomes the brachial artery (Figure 20.31). The brachial artery supplies blood to much of the brachial region and divides at the elbow into several smaller branches that supply blood to the antebrachium, carpus and hand. Figure 20.32 shows the distribution of systemic arteries from the heart into the upper limb. Table 20.9 summarises the main arteries serving the upper limbs.
The external iliac artery exits the body cavity and enters the femoral region of the lower limb. As it passes through the body wall deep to the inguinal ligament, it is renamed the femoral artery. The femoral artery provides all blood to the lower limb via its branches.
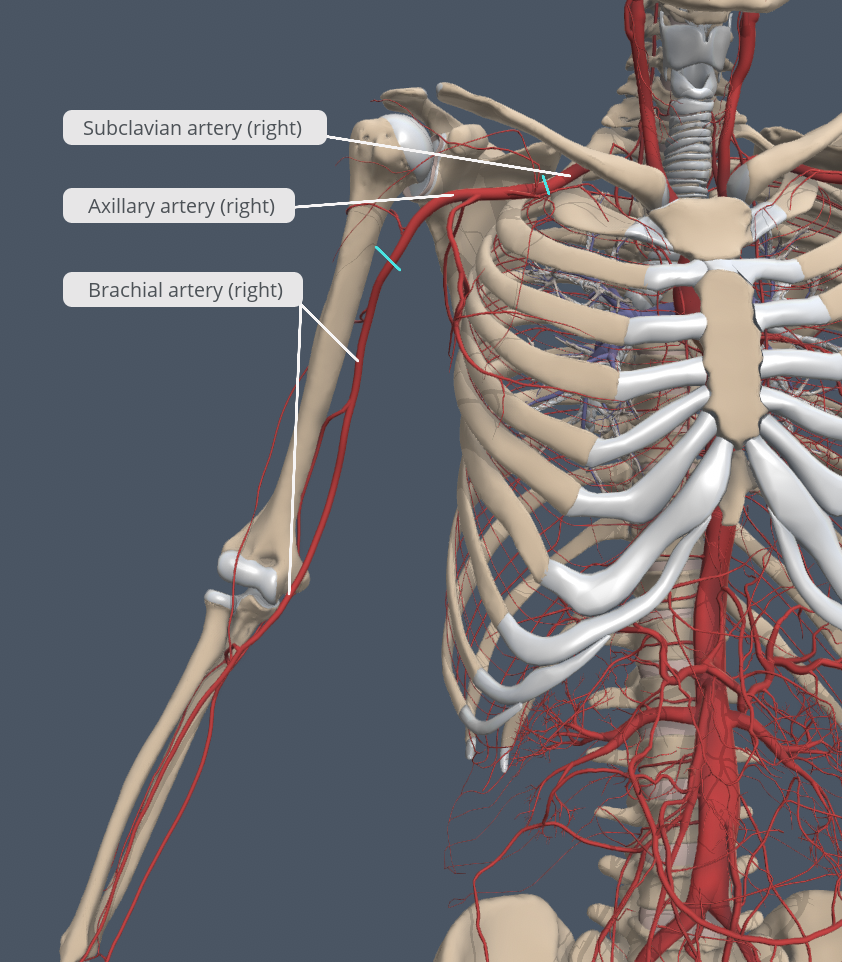
Figure 20.31 Major Arteries Serving the Upper Limb The arteries that supply blood to the upper limb are extensions of the subclavian arteries. Note the blue lines indicate the boundaries between the subclavian, axillary and brachial arteries. These vessels are continuations of each other, but change names as they move through different compartments of the body. [Created in Anatomy.TV, Primal Pictures]
Table 20.9 Arteries Serving the Limbs
| Vessel | Description |
| Axillary artery | Continuation of the subclavian artery as it penetrates the body wall and enters the axillary region; supplies blood to the region near the head of the humerus (humeral circumflex arteries); the majority of the vessel continues into the brachium and becomes the brachial artery |
| Brachial artery | Continuation of the axillary artery in the brachium; supplies blood to much of the brachial region; gives off several smaller branches that provide blood to the posterior surface of the arm in the region of the elbow; bifurcates into the radial and ulnar arteries at the coronoid fossa |
| Femoral artery | Continuation of the external iliac artery after it passes through the body cavity; divides into several smaller branches, the lateral deep femoral artery, and the genicular artery; becomes the popliteal artery as it passes posterior to the knee |
Systemic Veins
Systemic veins return blood to the right atrium. Since the blood has already passed through the systemic capillaries, it will be relatively low in oxygen concentration. In many cases, there will be veins draining organs and regions of the body with the same name as the arteries that supplied these regions and the two often parallel one another. This is often described as a “complementary” pattern. However, there is a great deal more variability in the venous circulation than normally occurs in the arteries. For the sake of brevity and clarity, this text will discuss only the most commonly encountered patterns. However, keep this variation in mind when you move from the classroom to clinical practice.
In both the neck and limb regions, there are often both superficial and deep levels of veins. The deep veins generally correspond to the complementary arteries. The superficial veins do not normally have direct arterial counterparts, but in addition to returning blood, they also make contributions to the maintenance of body temperature. When the ambient temperature is warm, more blood is diverted to the superficial veins where heat can be more easily dissipated to the environment. In colder weather, there is more constriction of the superficial veins and blood is diverted deeper where the body can retain more of the heat. Figure 20.35 outlines the path of the major systemic veins.
The right atrium receives all of the systemic venous return. Most of the blood flows into either the superior vena cava or inferior vena cava.
The Superior Vena Cava
The superior vena cava drains most of the body superior to the thoracic diaphragm, including the thoracic wall, head, neck and upper limbs (Figure 20.36). The subclavian vein carrying blood from the upper limbs forms a confluence with the internal jugular vein draining blood from the cranial cavity to form the brachiocephalic vein. The right and left brachiocephalic veins confluence to form the superior vena cava.
The remainder of the blood supply from the thorax drains into the larger right-sided azygos vein and the smaller left-sided hemiazygos vein (hemi- = “half”). The azygos vein drains into the superior vena cava at approximately the level of T2.
INTERACTIVE ACTIVITY
(a) Which artery runs parallel with the internal jugular vein in the neck?
(b) Describe the origin of the brachiocephalic vein.
(c) The median cubital vein is classified as a superficial vein. What does this mean and what is the significance of this specific vessel?
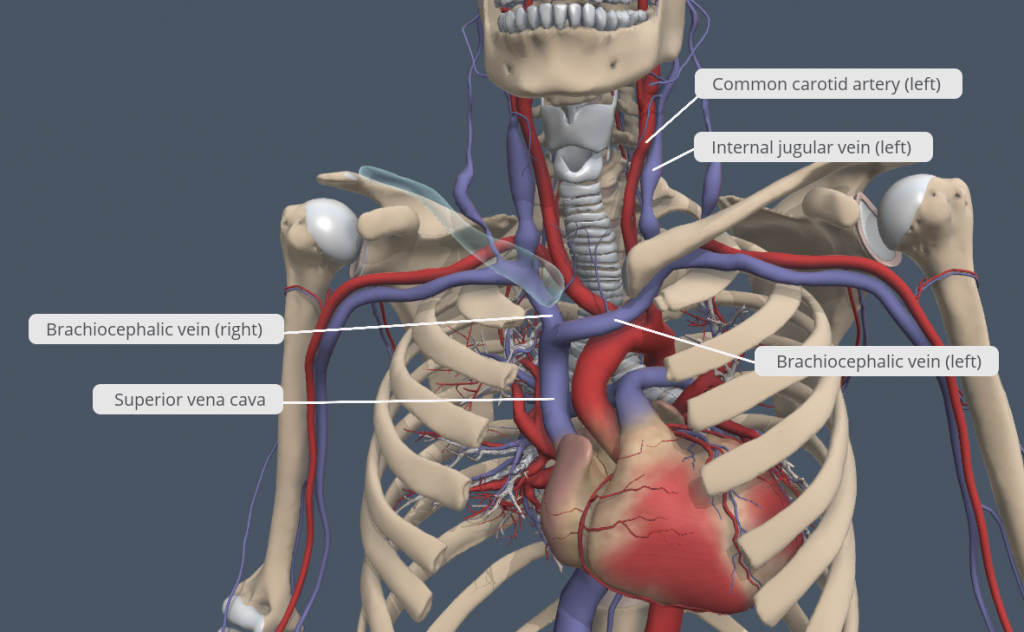
Figure 20.36 Tributaries of the Superior Vena Cava All blood from regions of the body superior to the thoracic diaphragm, travel in veins that return it to the right atrium via the superior vena cava. [Created in Anatomy.TV, Primal Pictures]
Table 20.11 summarises the veins of the thoracic region that flow into the superior vena cava.
Table 20.11 Veins of the Thoracic Region
| Vessel | Description |
| Superior vena cava | Large systemic vein; drains blood from most areas superior to the thoracic diaphragm; empties into the right atrium of the heart |
| Subclavian vein | Located deep in the thoracic cavity; formed as a continuation of the axillary vein as it enters the thoracic cavity from the axillary region; terminates by forming a confluence with the internal jugular vein to form the brachiocephalic vein |
| Internal jugular vein | Parallel to the common carotid artery, which is more or less its counterpart, and passes through the jugular foramen and canal; primarily drains blood from the brain; terminates as a confluence with the subclavian vein to form the brachiocephalic vein |
| Brachiocephalic veins | Pair of veins that form from a confluence of the internal jugular vein and the subclavian vein; drain the superior thoracic region and fuse together as a confluence to form the superior vena cava |
| Azygos vein | Located on the right side of the vertebral column; drains blood from the thoracic wall and terminates as a tributary into the superior vena cava |
| Hemiazygos vein | Smaller vein complementary to the azygos vein; located on the left side of the vertebral column; drains blood from the left side of the thoracic wall |
Venous Drainage of the Brain
Many small veins of the brainstem and cerebrum lead to larger vessels in the cranial cavity referred to as dural sinuses (Figure 20.37). Most of this venous blood flows into the largest of the sinuses, the superior sagittal sinus. It is located midsagittally between the meningeal and periosteal layers of the dura mater within the falx cerebri. Most reabsorption of cerebrospinal fluid occurs via the arachnoid granulations into the superior sagittal sinus. The superior sagittal sinus is continuous with the right and left transverse sinuses at a dilation called the confluence of the sinuses. The transverse sinuses in turn flow into the sigmoid sinuses that pass through the jugular foramen and into the internal jugular vein. The internal jugular vein flows parallel to the common carotid artery and is more or less its counterpart.
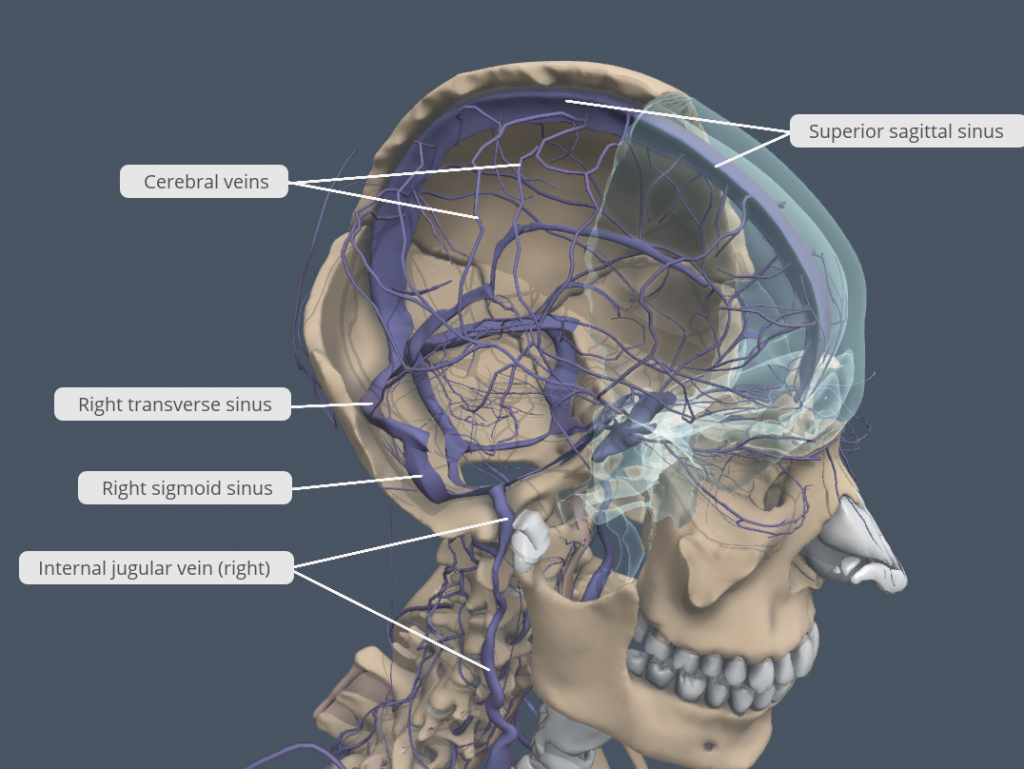
Figure 13.16 Dural Sinuses and Veins Blood drains from the brain through a series of sinuses formed in the walls of the dura mater that connect to the internal jugular veins. [Created in Anatomy.TV, Primal Pictures]
Veins Draining the Upper Limbs
The deep veins of the upper limb are named according to the artery they accompany (for example the brachial vein). A number of superficial veins also course through the upper limb including the median cubital vein that crosses at an angle in the antecubital fossa (anterior elbow). The median cubital vein is the most common site for drawing venous blood in humans.
Table 20.13 Major Veins of the Brain and Upper Limb
| Vessel | Description |
| Superior sagittal sinus | Enlarged vein located midsagittally between the meningeal and periosteal layers of the dura mater within the falx cerebri; receives most of the blood drained from the superior surface of the cerebrum and terminates by dividing into the right and left transverse sinuses |
| Transverse sinuses | Pair of enlarged veins near the lambdoidal suture that drains the superior sagittal sinus, and leads to the sigmoid sinuses |
| Sigmoid sinuses | Enlarged vein that receives blood from the transverse sinuses and terminates at the jugular foramen as the internal jugular vein |
| Brachial vein | Deeper vein of the arm that forms from the radial and ulnar veins in the lower arm; leads to the axillary vein |
| Median cubital vein | Superficial vessel located in the antecubital region; a frequent site from which to draw blood |
The Inferior Vena Cava
Lying just deep to the parietal peritoneum in the abdominal cavity in the retroperitoneal compartment, the inferior vena cava parallels the abdominal aorta, where it can receive blood from abdominal veins. The inferior vena cava is formed from the confluence of the paired common iliac veins at the vertebral level of L5.
Blood supply from the kidneys flows into each renal vein, normally the largest veins entering the inferior vena cava. From the male reproductive organs, each testicular vein flows from the scrotum, forming a portion of the spermatic cord. Each ovarian vein drains an ovary in females. Each of these veins is generically called a gonadal vein. The right gonadal vein empties directly into the inferior vena cava, and the left gonadal vein is a tributary of the left renal vein.
Veins Draining the Lower Limbs
The deep veins of the lower limb are named according to the artery they accompany (for example, the femoral vein). A number of superficial veins also course through the lower limb including the great saphenous vein that is a prominent surface vessel located on the medial surface of the leg and thigh that collects blood from the superficial portions of these areas.
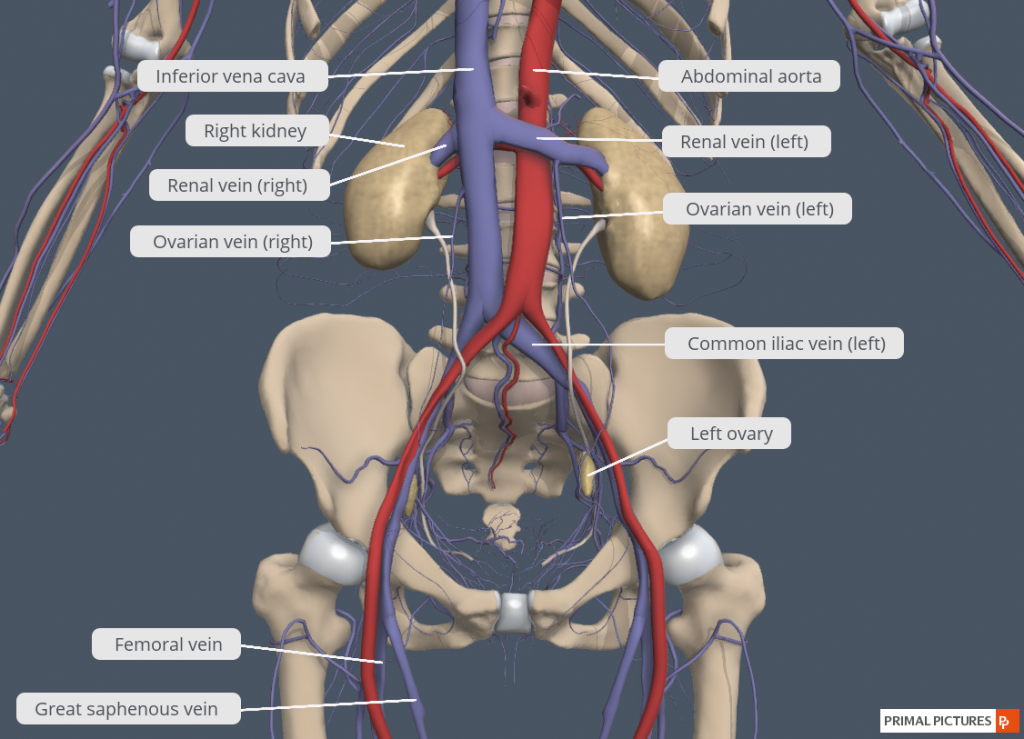
Figure 20.36 Tributaries of the Inferior Vena Cava Blood from the organs of the abdomen, pelvis and lower limb will eventually drain to the inferior vena cava. The inferior vena cava is formed from the confluence of the right and left common iliac veins that drain blood from the lower limbs. Direct tributaries of the inferior vena cava include the renal veins, gonadal veins and hepatic veins. The great saphenous vein is an example of a superficial vein. It is located medially from its origin at the tarsus to its termination as a tributary into the femoral vein. [Created in Anatomy.TV, Primal Pictures]
Table 20.15 summarises the major veins of the abdominal region and lower limb.
Table 20.15 Major Veins of the Abdominal Region and Lower Limb
| Vessel | Description |
| Inferior vena cava | Large systemic vein that drains blood from areas largely inferior to the thoracic diaphragm; empties into the right atrium |
| Renal vein | Largest vein entering the inferior vena cava; drains the kidneys and is a tributary of the inferior vena cava |
| Testicular vein | Drains the testes and forms part of the spermatic cord; the right testicular vein is a direct tributary of the inferior vena cava and the left testicular vein is a tributary of the left renal vein |
| Ovarian vein | Drains the ovary; the right ovarian vein empties is a direct tributary of the inferior vena cava and the left ovarian vein is a tributary of the left renal vein |
| Gonadal vein | Generic term for a vein draining a reproductive organ; may be either an ovarian vein or a testicular vein, depending on the sex of the individual |
| Common iliac vein | Flows into the inferior vena cava at the level of L5; the left common iliac vein drains the sacral region; formed from the union of the external and internal iliac veins near the inferior portion of the sacroiliac joint |
| Femoral vein | Drains the femoral region (thigh); becomes continuous with the external iliac vein when it crosses the body wall deep to the inguinal ligament |
| Great saphenous vein | Prominent superficial vein located on the medial surface of the lower limb; drains the superficial portions of these areas and is a tributary of the femoral vein |
INTERACTIVE ACTIVITY
Review photos of the torso models displaying the blood vessels of the abdomen, pelvis and femoral region by clicking the arrows beside each image, or the buttons below the image panel. Identify both internal and external features of the heart in each photo. Test your knowledge on the unlabelled photos before revealing the names of the main features in the labelled photo. [Created in Anatomy.TV, Primal Pictures]
Question:
(a) Review the blood supply and drainage of each of the labelled vessels
Venae Comitantes
Blood in the distal parts of the limbs have the furthest to travel to reach the right atrium of the heart. As veins have relatively thin muscular walls, these distal veins rely on surrounding structures to support the transport of blood against gravity across long distances. This includes the contraction of the muscle compartments they course through but also by travelling alongside the deep arteries. Veins in the most distal parts of the limbs are organised in venae comitantes, which are paired veins that lie on either side of an artery. These paired veins have small collateral veins that cross and connect between them over and under the artery. In this way the venae comitantes are compressed at the same time as the arteries when the tunica media of the arterial wall contracts, helping to push the blood through the most distal parts of the body.
INTERACTIVE ACTIVITY
Hepatic Portal System
The liver is a complex biochemical processing plant. It packages nutrients absorbed by the digestive system; produces plasma proteins, clotting factors, and bile; and disposes of worn-out cell components and waste products. Instead of entering the circulation directly, absorbed nutrients and certain wastes travel to the liver for processing. They do so via the hepatic portal system (Figure 20.43). Blood from the stomach, small intestine, large intestine and spleen lead to the hepatic portal vein and end in specialised capillaries within the liver, the hepatic sinusoids.
The hepatic portal system consists of the hepatic portal vein (or portal vein) and the veins that drain into it. The hepatic portal vein itself is relatively short, and typically arises in the abdomen as a confluence of the superior mesenteric and splenic veins. The superior mesenteric vein receives blood from the small intestine, two-thirds of the large intestine, and the stomach. The inferior mesenteric vein drains the distal third of the large intestine, including the descending colon, the sigmoid colon, and the rectum. The splenic vein is formed from branches from the spleen, pancreas, and portions of the stomach, and the inferior mesenteric vein. The hepatic portal vein delivers materials from these digestive and lymphatic organs directly to the liver for processing.
Because of the hepatic portal system, the liver receives its blood supply from two different sources: from normal systemic circulation via the common hepatic artery (terminal branch of the coeliac trunk) and from the hepatic portal vein. The liver processes the blood from the portal system to remove certain wastes and excess nutrients, which are stored for later use. This processed blood, as well as the systemic blood that came from the common hepatic artery, exits the liver in the hepatic veins, and flows into the inferior vena cava.
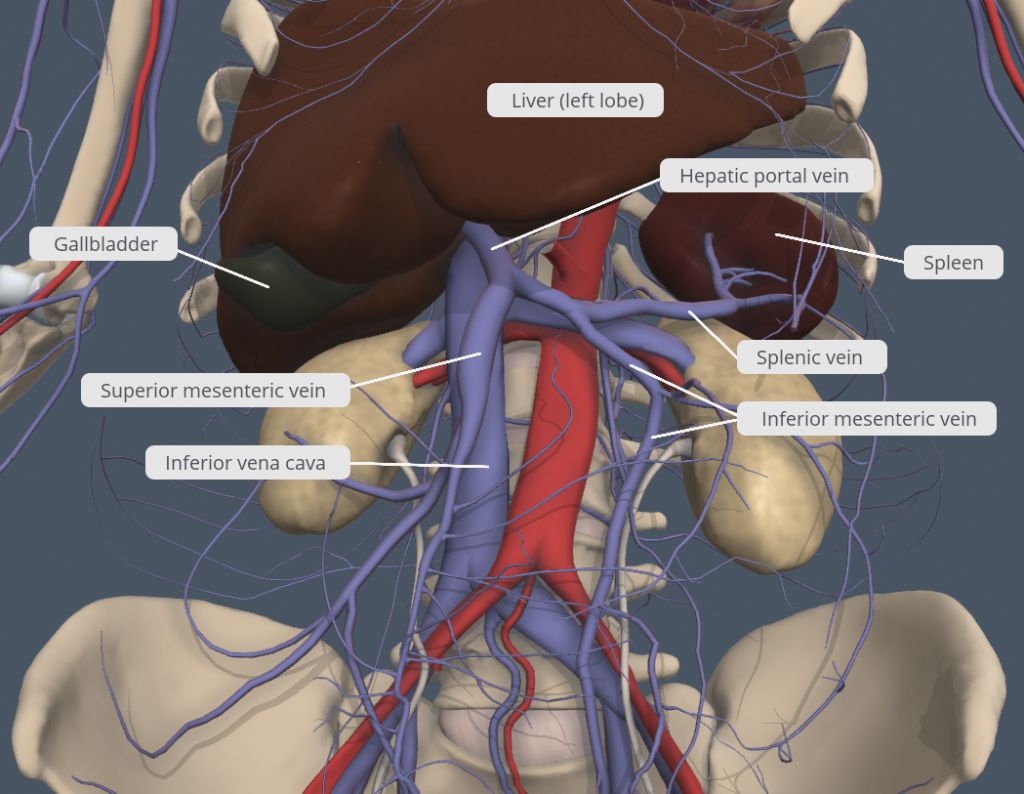
Figure 20.43 Hepatic Portal System The liver receives oxygenated blood from the normal systemic circulation via the common hepatic artery. It also receives and processes blood from other organs, delivered via the veins of the hepatic portal system. This blood is rich in absorbed nutrients from the intestine and waste products from the spleen. The hepatic portal system consists of the superior mesenteric and splenic veins which confluence to form the hepatic portal vein. All blood exits the liver via the hepatic veins, which delivers the blood to the inferior vena cava. [Created in Anatomy.TV, Primal Pictures]
Key Terms
abdominal aorta portion of the aorta inferior to the aortic hiatus and superior to the common iliac arteries
agranular leukocytes leukocytes with few granules in their cytoplasm; specifically, monocytes, lymphocytes, and NK cells
aorta largest artery in the body, originating from the left ventricle and descending to the abdominal region where it bifurcates into the common iliac arteries at the level of the fourth lumbar vertebra; arteries originating from the aorta distribute blood to virtually all tissues of the body
anastomosis (plural = anastomoses) area where vessels unite to allow blood to circulate even if there may be partial blockage in another branch
anterior interventricular artery (also, left anterior descending artery or LAD) major branch of the left coronary artery that follows the anterior interventricular sulcus
anterior interventricular sulcus heart sulcus located between the left and right ventricles on the anterior surface of the heart
aortic valve (also, aortic semilunar valve) valve located at the base of the aorta
antibodies (also, immunoglobulins or gamma globulins) antigen-specific proteins produced by specialized B lymphocytes that protect the body by binding to foreign objects such as bacteria and viruses
aortic arch arc that connects the ascending aorta to the descending aorta; ends at the intervertebral disk between the fourth and fifth thoracic vertebrae
aortic hiatus opening in the diaphragm that allows passage of the thoracic aorta into the abdominal region where it becomes the abdominal aorta
arteriole (also, resistance vessel) very small artery that leads to a capillary
artery blood vessel that conducts blood away from the heart; may be a conducting or distributing vessel
ascending aorta initial portion of the aorta, rising from the left ventricle for a distance of approximately 5 cm
atrioventricular valves one-way valves located between the atria and ventricles; the valve on the right is called the tricuspid valve, and the one on the left is the mitral or bicuspid valve
atrium (plural = atria) upper or receiving chamber of the heart that pumps blood into the lower chambers just prior to their contraction; the right atrium receives blood from the systemic circuit that flows into the right ventricle; the left atrium receives blood from the pulmonary circuit that flows into the left ventricle
auricle extension of an atrium visible on the superior surface of the heart
axillary artery continuation of the subclavian artery as it penetrates the body wall and enters the axillary region; supplies blood to the region near the head of the humerus (humeral circumflex arteries); the majority of the vessel continues into the brachium and becomes the brachial artery
axillary vein major vein in the axillary region; drains the upper limb and becomes the subclavian vein
azygos vein originates in the lumbar region and passes through the thoracic diaphragm into the thoracic cavity on the right side of the vertebral column; drains blood from the intercostal veins, esophageal veins, bronchial veins, and other veins draining the mediastinal region; leads to the superior vena cava
bicuspid valve (also, mitral valve or left atrioventricular valve) valve located between the left atrium and ventricle; consists of two flaps of tissue
B lymphocytes (also, B cells) lymphocytes that defend the body against specific pathogens and thereby provide specific immunity
basophils granulocytes that stain with a basic (alkaline) stain and store histamine and heparin
blood liquid connective tissue composed of formed elements—erythrocytes, leukocytes, and platelets—and a fluid extracellular matrix called plasma; component of the cardiovascular system
brachial artery continuation of the axillary artery in the brachium; supplies blood to much of the brachial region; gives off several smaller branches that provide blood to the posterior surface of the arm in the region of the elbow; bifurcates into the radial and ulnar arteries at the coronoid fossa
brachial vein deeper vein of the arm that forms from the radial and ulnar veins in the lower arm; leads to the axillary vein
brachiocephalic trunk single vessel located on the right side of the body; the first vessel branching from the aortic arch; gives rise to the right subclavian artery and the right common carotid artery; supplies blood to the head, neck, upper limb, and wall of the thoracic region
brachiocephalic vein one of a pair of veins that form from a fusion of the external and internal jugular veins and the subclavian vein; subclavian, external and internal jugulars, vertebral, and internal thoracic veins lead to it; drains the upper thoracic region and flows into the superior vena cava
capillary smallest of blood vessels where physical exchange occurs between the blood and tissue cells surrounded by interstitial fluid
cardiac veins vessels that drain the heart and generally parallel the large surface arteries
carotid sinuses small pockets near the base of the internal carotid arteries that are the locations of the baroreceptors and chemoreceptors that trigger a reflex that aids in the regulation of vascular homeostasis
coeliac trunk major branch of the abdominal aorta; gives rise to the left gastric artery, the splenic artery, and the common hepatic artery that forms the hepatic artery to the liver, the right gastric artery to the stomach, and the cystic artery to the gall bladder
cerebral arterial circle (also, circle of Willis) anastomosis located at the base of the brain that ensures continual blood supply; formed from branches of the internal carotid and vertebral arteries; supplies blood to the brain
chordae tendineae string-like extensions of tough connective tissue that extend from the flaps of the atrioventricular valves to the papillary muscles
circumflex artery branch of the left coronary artery that follows coronary sulcus
common carotid artery right common carotid artery arises from the brachiocephalic artery, and the left common carotid arises from the aortic arch; gives rise to the external and internal carotid arteries; supplies the respective sides of the head and neck
common hepatic artery branch of the celiac trunk that forms the hepatic artery, the right gastric artery, and the cystic artery
common iliac artery branch of the aorta that leads to the internal and external iliac arteries
common iliac vein one of a pair of veins that flows into the inferior vena cava at the level of L5; the left common iliac vein drains the sacral region; divides into external and internal iliac veins near the inferior portion of the sacroiliac joint
continuous capillary most common type of capillary, found in virtually all tissues except epithelia and cartilage; contains very small gaps in the endothelial lining that permit exchange
coronary arteries branches of the ascending aorta that supply blood to the heart; the left coronary artery feeds the left side of the heart, the left atrium and ventricle, and the interventricular septum; the right coronary artery feeds the right atrium, portions of both ventricles, and the heart conduction system
coronary sinus large, thin-walled vein on the posterior surface of the heart that lies within the atrioventricular sulcus and drains the heart myocardium directly into the right atrium
descending aorta portion of the aorta that continues downward past the end of the aortic arch; subdivided into the thoracic aorta and the abdominal aorta
elastic artery (also, conducting artery) artery with abundant elastic fibers located closer to the heart, which maintains the pressure gradient and conducts blood to smaller branches
eosinophils granulocytes that stain with eosin; they release antihistamines and are especially active against parasitic worms
erythrocyte (also, red blood cell) mature myeloid blood cell that is composed mostly of hemoglobin and functions primarily in the transportation of oxygen and carbon dioxide
external carotid artery arises from the common carotid artery; supplies blood to numerous structures within the face, lower jaw, neck, esophagus, and larynx
external elastic membrane membrane composed of elastic fibers that separates the tunica media from the tunica externa; seen in larger arteries
external iliac artery branch of the common iliac artery that leaves the body cavity and becomes a femoral artery; supplies blood to the lower limbs
external iliac vein formed when the femoral vein passes into the body cavity; drains the legs and leads to the common iliac vein
femoral artery continuation of the external iliac artery after it passes through the body cavity; divides into several smaller branches, the lateral deep femoral artery, and the genicular artery; becomes the popliteal artery as it passes posterior to the knee
femoral vein drains the upper leg; receives blood from the great saphenous vein, the deep femoral vein, and the femoral circumflex vein; becomes the external iliac vein when it crosses the body wall
fenestrated capillary type of capillary with pores or fenestrations in the endothelium that allow for rapid passage of certain small materials
fossa ovalis oval-shaped depression in the interatrial septum that marks the former location of the foramen ovale
gonadal artery branch of the abdominal aorta; supplies blood to the gonads or reproductive organs; also described as ovarian arteries or testicular arteries, depending upon the sex of the individual
gonadal vein generic term for a vein draining a reproductive organ; may be either an ovarian vein or a testicular vein, depending on the sex of the individual
granular leukocytes leukocytes with abundant granules in their cytoplasm; specifically, neutrophils, eosinophils, and basophils
great saphenous vein prominent surface vessel located on the medial surface of the leg and thigh; drains the superficial portions of these areas and leads to the femoral vein
haematopoiesis (hemopoiesis) production of the formed elements of blood
hemiazygos vein smaller vein complementary to the azygos vein; drains the esophageal veins from the esophagus and the left intercostal veins, and leads to the brachiocephalic vein via the superior intercostal vein
hepatic portal system specialized circulatory pathway that carries blood from digestive organs to the liver for processing before being sent to the systemic circulation
hepatic vein drains systemic blood from the liver and flows into the inferior vena cava
inferior vena cava large systemic vein that returns blood to the heart from the inferior portion of the body
inferior mesenteric artery branch of the abdominal aorta; supplies blood to the distal segment of the large intestine and rectum
inferior vena cava large systemic vein that drains blood from areas largely inferior to the diaphragm; empties into the right atrium
interatrial septum cardiac septum located between the two atria; contains the fossa ovalis after birth
internal carotid artery arises from the common carotid artery and begins with the carotid sinus; goes through the carotid canal of the temporal bone to the base of the brain; combines with branches of the vertebral artery forming the arterial circle; supplies blood to the brain
internal elastic membrane membrane composed of elastic fibers that separates the tunica intima from the tunica media; seen in larger arteries
internal iliac artery branch from the common iliac arteries; supplies blood to the urinary bladder, walls of the pelvis, external genitalia, and the medial portion of the femoral region; in females, also provide blood to the uterus and vagina
internal iliac vein drains the pelvic organs and integument; formed from several smaller veins in the region; leads to the common iliac vein
internal jugular vein one of a pair of major veins located in the neck region that passes through the jugular foramen and canal, flows parallel to the common carotid artery that is more or less its counterpart; primarily drains blood from the brain, receives the superficial facial vein, and empties into the subclavian vein
interventricular septum cardiac septum located between the two ventricles
interventricular sulcus (or groove) sulcus that marks the boundary between the atria and ventricles
left atrioventricular valve (also, mitral valve or bicuspid valve) valve located between the left atrium and ventricle; consists of two flaps of tissue
leukocyte (also, white blood cell) colorless, nucleated blood cell, the chief function of which is to protect the body from disease
lumen interior of a tubular structure such as a blood vessel or a portion of the alimentary canal through which blood, chyme, or other substances travel
lymphocytes agranular leukocytes of the lymphoid stem cell line, many of which function in specific immunity
macrophage phagocytic cell of the myeloid lineage; a matured monocyte
median cubital vein superficial vessel located in the antecubital region that links the cephalic vein to the basilic vein in the form of a v; a frequent site for a blood draw
megakaryocyte bone marrow cell that produces platelets
mitral valve (also, left atrioventricular valve or bicuspid valve) valve located between the left atrium and ventricle; consists of two flaps of tissue
monocytes agranular leukocytes of the myeloid stem cell line that circulate in the bloodstream; tissue monocytes are macrophages
muscular artery (also, distributing artery) artery with abundant smooth muscle in the tunica media that branches to distribute blood to the arteriole network
myocardium thickest layer of the heart composed of cardiac muscle cells built upon a framework of primarily collagenous fibers and blood vessels that supply it and the nervous fibers that help to regulate it
neutrophils granulocytes that stain with a neutral dye and are the most numerous of the leukocytes; especially active against bacteria
ovarian artery branch of the abdominal aorta; supplies blood to the ovary, uterine (Fallopian) tube, and uterus
ovarian vein drains the ovary; the right ovarian vein leads to the inferior vena cava and the left ovarian vein leads to the left renal vein
papillary muscle extension of the myocardium in the ventricles to which the chordae tendineae attach
pectinate muscles muscular ridges seen on the anterior surface of the right atrium
pericardial cavity cavity surrounding the heart filled with a lubricating serous fluid that reduces friction as the heart contracts
pericardial sac (also, pericardium) membrane that separates the heart from other mediastinal structures; consists of two distinct, fused sublayers: the fibrous pericardium and the parietal pericardium
pericardium (also, pericardial sac) membrane that separates the heart from other mediastinal structures
plasma in blood, the liquid extracellular matrix composed mostly of water that circulates the formed elements and dissolved materials throughout the cardiovascular system
platelets (also, thrombocytes) one of the formed elements of blood that consists of cell fragments broken off from megakaryocytes
pulmonary arteries left and right branches of the pulmonary trunk that carry deoxygenated blood from the heart to each of the lungs
pulmonary capillaries capillaries surrounding the alveoli of the lungs where gas exchange occurs: carbon dioxide exits the blood and oxygen enters
pulmonary circuit system of blood vessels that provide gas exchange via a network of arteries, veins, and capillaries that run from the heart, through the body, and back to the lungs
pulmonary trunk large arterial vessel that carries blood ejected from the right ventricle; divides into the left and right pulmonary arteries
pulmonary semilunar valve valve at the base of the pulmonary trunk that prevents backflow of blood into the right ventricle; consists of three flaps
pulmonary veins veins that carry highly oxygenated blood into the left atrium, which pumps the blood into the left ventricle, which in turn pumps oxygenated blood into the aorta and to the many branches of the systemic circuit
renal artery branch of the abdominal aorta; supplies each kidney
renal vein largest vein entering the inferior vena cava; drains the kidneys and leads to the inferior vena cava
right atrioventricular valve (also, tricuspid valve) valve located between the right atrium and ventricle; consists of three flaps of tissue
semilunar valves valves located at the base of the pulmonary trunk and at the base of the aorta
sigmoid sinuses enlarged veins that receive blood from the transverse sinuses; flow through the jugular foramen and into the internal jugular vein
sinusoid capillary rarest type of capillary, which has extremely large intercellular gaps in the basement membrane in addition to clefts and fenestrations; found in areas such as the bone marrow and liver where passage of large molecules occurs
skeletal muscle pump effect on increasing blood pressure within veins by compression of the vessel caused by the contraction of nearby skeletal muscle
splenic artery branch of the celiac trunk; supplies blood to the spleen
subclavian artery right subclavian arises from the brachiocephalic artery, whereas the left subclavian artery arises from the aortic arch; gives rise to the internal thoracic, vertebral, and thyrocervical arteries; supplies blood to the arms, chest, shoulders, back, and central nervous system
subclavian vein located deep in the thoracic cavity; becomes the axillary vein as it enters the axillary region; drains the axillary and smaller local veins near the scapular region; leads to the brachiocephalic vein
superior mesenteric artery branch of the abdominal aorta; supplies blood to the small intestine (duodenum, jejunum, and ileum), the pancreas, and a majority of the large intestine
superior sagittal sinus enlarged vein located midsagittally between the meningeal and periosteal layers of the dura mater within the falx cerebri; receives most of the blood drained from the superior surface of the cerebrum and leads to the inferior jugular vein and the vertebral vein
superior vena cava large systemic vein; drains blood from most areas superior to the thoracic diaphragm; empties into the right atrium
systemic circuit blood flow to and from virtually all of the tissues of the body
testicular artery branch of the abdominal aorta; will ultimately travel outside the body cavity to the testes and form one component of the spermatic cord
testicular vein drains the testes and forms part of the spermatic cord; the right testicular vein empties directly into the inferior vena cava and the left testicular vein empties into the left renal vein
thoracic aorta portion of the descending aorta superior to the aortic hiatus
T lymphocytes (also, T cells) lymphocytes that provide cellular-level immunity by physically attacking foreign or diseased cells
trabeculae carneae ridges of muscle covered by endocardium located in the ventricles
transverse sinuses pair of enlarged veins near the lambdoid suture that drain the occipital, sagittal, and straight sinuses, and leads to the sigmoid sinuses
tricuspid valve term used most often in clinical settings for the right atrioventricular valve
tunica externa (also, tunica adventitia) outermost layer or tunic of a vessel (except capillaries)
tunica intima (also, tunica interna) innermost lining or tunic of a vessel
tunica media middle layer or tunic of a vessel (except capillaries)
valve in the cardiovascular system, a specialized structure located within the heart or vessels that ensures one-way flow of blood
vein blood vessel that conducts blood toward the heart
ventricle one of the primary pumping chambers of the heart located in the lower portion of the heart; the left ventricle is the major pumping chamber on the lower left side of the heart that ejects blood into the systemic circuit via the aorta and receives blood from the left atrium; the right ventricle is the major pumping chamber on the lower right side of the heart that ejects blood into the pulmonary circuit via the pulmonary trunk and receives blood from the right atrium
venule small vessel leading from the capillaries to veins
vertebral artery arises from the subclavian artery and passes through the vertebral foramen through the foramen magnum to the brain; joins with the internal carotid artery to form the arterial circle; supplies blood to the brain and spinal cord