Chapter 5: RESPIRATORY SYSTEM
Introduction
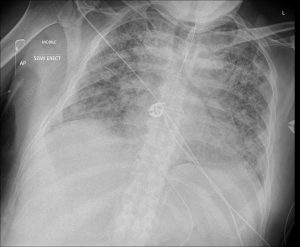
COVID-19 pneumonia This is a chest x-ray of a 55 year old patient suffering from COVID-19 pneumonia (day 24). Inflammation can be seen throughout the lungs as patches of white material. [Case courtesy of Dr Ian Bickle, Radiopaedia.org, rID: 75844].
Chapter Objectives
After studying this chapter, you will be able to:
- Describe and identify the macroscopic features of the major organs of the upper and lower respiratory tract
- Describe and identify the microscopic features of the bronchotracheal tree and lungs
- Describe the major functions of the respiratory system
Hold your breath. Really! See how long you can hold your breath as you continue reading… How long can you do it? Chances are you are feeling uncomfortable already. A typical human cannot survive without breathing for more than 3 minutes, and even if you wanted to hold your breath longer, your autonomic nervous system would take control. You may be surprised to learn that although oxygen is a critical need for cells, it is actually the accumulation of carbon dioxide that primarily drives your need to breathe. Carbon dioxide is exhaled and oxygen is inhaled through the respiratory system, which includes muscles to move air into and out of the lungs, passageways through which air moves, and microscopic gas exchange surfaces covered by capillaries. The circulatory system transports gases from the lungs to tissues throughout the body and vice versa. A variety of diseases can affect the respiratory system, such as asthma, emphysema, chronic obstruction pulmonary disorder (COPD), and lung cancer. All of these conditions affect the gas exchange process and result in laboured breathing and other difficulties.
Organs and Structures of the Respiratory System
Learning Objectives
By the end of this section, you will be able to:
- Identify and describe the the macroscopic features of the nose, nasal conchae, nasal meatuses and paranasal sinuses
- Identify and describe the three regions of the pharynx and their boundaries
- Identify and describe the cartilages and internal features of the larynx
- Identify and describe the macroscopic and microscopic anatomy of the trachea and bronchi
The major organs of the respiratory system function primarily to provide oxygen to body tissues for cellular respiration, remove the waste product carbon dioxide, and help to maintain acid-base balance. Portions of the respiratory system are also used for non-vital functions, such as sensing odours, speech production, and for straining, such as during childbirth or coughing.
INTERACTIVE ACTIVITY
Functionally, the respiratory system can be divided into a conducting zone and a respiratory zone. The conducting zone of the respiratory system includes the organs and structures not directly involved in gas exchange. The gas exchange occurs in the respiratory zone.
Conducting Zone
The major functions of the conducting zone are to provide a route for incoming and outgoing air, remove debris and pathogens from the incoming air, and warm and humidify the incoming air. Several structures within the conducting zone perform other functions as well. The epithelium of the nasal passages, for example, is essential to sensing odors, and the bronchial epithelium that lines the lungs can metabolise some airborne carcinogens. The conducting zone consists of the nose, pharynx, larynx, trachea and bronchial tree.
Respiratory Zone
In contrast to the conducting zone, the respiratory zone includes structures that are directly involved in gas exchange. Structures of the respiratory zone consist of respiratory bronchioles, alveolar ducts and alveoli.
The Nose and its Adjacent Structures
The major entrance and exit for the respiratory system is through the nose. When discussing the nose, it is helpful to divide it into two major sections: the external nose, and the nasal cavity or internal nose.
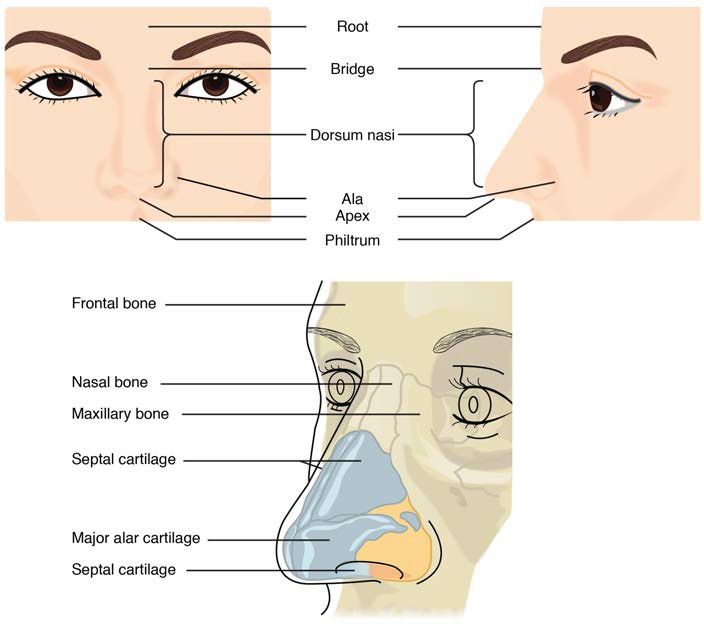
The external nose consists of the surface and skeletal structures that result in the outward appearance of the nose and contribute to its numerous functions (Figure 22.3). The root is the region of the nose located between the eyebrows. The bridge is the part of the nose that connects the root to the rest of the nose.
Figure 22.3 Nose This illustration shows features of the external nose (top) and skeletal features of the nose (bottom).
Deep to the thin skin of the nose are its skeletal features (see Figure 22.3, lower illustration). While the root and bridge of the nose consist of bone, the protruding portion of the nose is composed of hyaline cartilage. As a result, when looking at a skull, there are no bones visible in this inferior portion of the nose. The nasal bones are a pair of bones that lie under the root and bridge of the nose. The nasal bone articulates superiorly with the frontal bone and laterally with the maxillary bones.
The external nares (nostril opening) open into the nasal cavity, which is separated into left and right sections by the nasal septum. The nares and anterior portion of the nasal cavities are lined with mucous membranes, containing sebaceous glands and hair follicles that serve to prevent the passage of large debris, such as dirt, through the nasal cavity. An olfactory epithelium used to detect odors is found deeper in the nasal cavity.
The nasal septum is formed anteriorly by a portion of the septal cartilage (the flexible portion you can touch with your fingers) and posteriorly by the perpendicular plate of the ethmoid bone and the thin vomer bones (Figure XX).
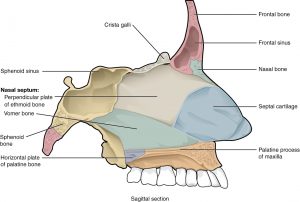
Figure XX Nasal Septum This illustration shows the cartilaginous and bony structures that make up the nasal septum.
Each lateral wall of the nasal cavity has three bony projections, called the superior, middle, and inferior nasal conchae. The inferior conchae are separate bones, whereas the superior and middle conchae are portions of the ethmoid bone. Conchae serve to increase the surface area of the nasal cavity and to disrupt the flow of air as it enters the nose, causing air to bounce along the epithelium, where it is cleaned and warmed. The conchae and meatuses also conserve water and prevent dehydration of the nasal epithelium by trapping water during exhalation (Figure XX). The floor of the nasal cavity is composed of the palate. The hard palate at the anterior region of the nasal cavity is composed of bone. The soft palate at the posterior portion of the nasal cavity consists of muscle tissue. Air exits the nasal cavities via the internal nares and moves into the nasopharynx (Figure XX).
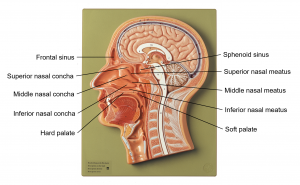
Figure XX Nasal Cavity This illustration shows the structures of the nasal cavity in a sagittal section of the head and neck.
Paranasal Sinuses
The paranasal sinuses are hollow, air-filled spaces located within certain bones of the skull (Figure 7.18). All of the sinuses communicate with the nasal cavity (para = alongside) and are lined with respiratory mucosa. They serve to reduce bone mass and thus lighten the skull, and they also add resonance to the voice. This second feature is most obvious when you have a cold or sinus congestion. These conditions produce swelling of the mucosa and excess mucus production, which can obstruct the narrow passageways between the sinuses and the nasal cavity, causing your voice to sound different to yourself and others. This blockage can also allow the sinuses to fill with fluid, with the resulting pressure producing pain and discomfort.
The paranasal sinuses are named for the skull bone that each occupies. The frontal sinus is located just superior to the eyebrows, within the frontal bone (see Figure 7.17). This irregular space may be divided at the midline into bilateral spaces, or these may be fused into a single sinus space. The frontal sinus is the most anterior of the paranasal sinuses. The largest sinus is the maxillary sinus. These are paired and located within the right and left maxillary bones, where they occupy the area just inferior to the orbits. The maxillary sinuses are most commonly involved during sinus infections. Because their connection to the nasal cavity is located relatively superior on their medial wall, they are difficult to drain. The sphenoid sinus is a single, midline sinus. It is located within the body of the sphenoid, just anterior and inferior to the sella turcica, thus making it the most posterior of the paranasal sinuses. The lateral aspects of the ethmoid contain multiple small spaces separated by very thin bony walls. Each of these spaces is called an ethmoid air cell. These are located on both sides of the ethmoid, between the superior nasal cavity and medial orbit, just posterior to the superior nasal conchae.
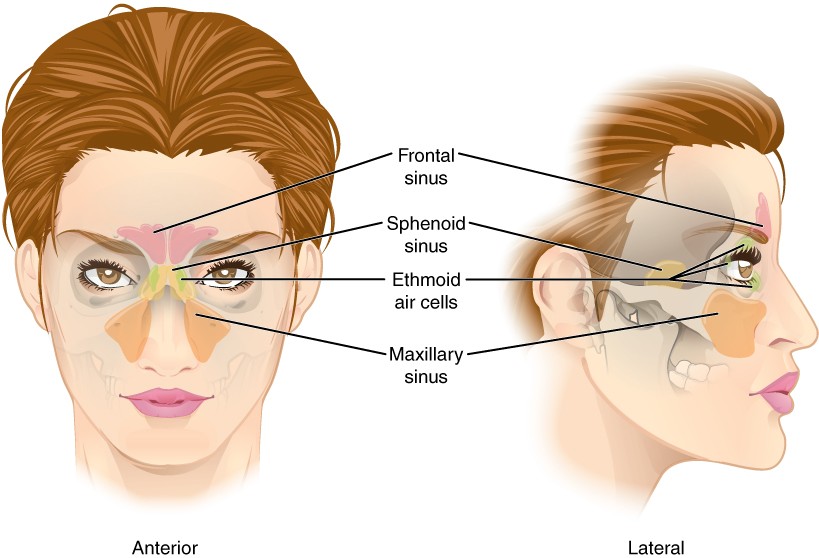
Figure 7.18 Paranasal Sinuses The paranasal sinuses are hollow, air-filled spaces named for the skull bone that each occupies. The most anterior is the frontal sinus, located in the frontal bone superior to the eyebrows. The largest are the maxillary sinuses, located in the right and left maxillary bones inferior to the orbits. The most posterior is the sphenoid sinus, located in the body of the sphenoid, deep to the sella turcica. The ethmoid air cells are multiple small spaces located in the right and left sides of the ethmoid, between the medial wall of the orbit and lateral wall of the superior nasal cavity.
The conchae, meatuses, and paranasal sinuses are lined by respiratory epithelium composed of ciliated pseudostratified columnar epithelium (Figure 22.5). The epithelium contains goblet cells, one of the specialised, columnar epithelial cells that produce mucus to trap debris. The cilia of the respiratory epithelium help remove the mucus and debris from the nasal cavity with a constant beating motion, sweeping materials towards the pharynx to be swallowed. Interestingly, cold air slows the movement of the cilia, resulting in accumulation of mucus that may in turn lead to a runny nose during cold weather. This moist epithelium functions to warm and humidify incoming air. Capillaries located just beneath the nasal epithelium warm the air by convection.
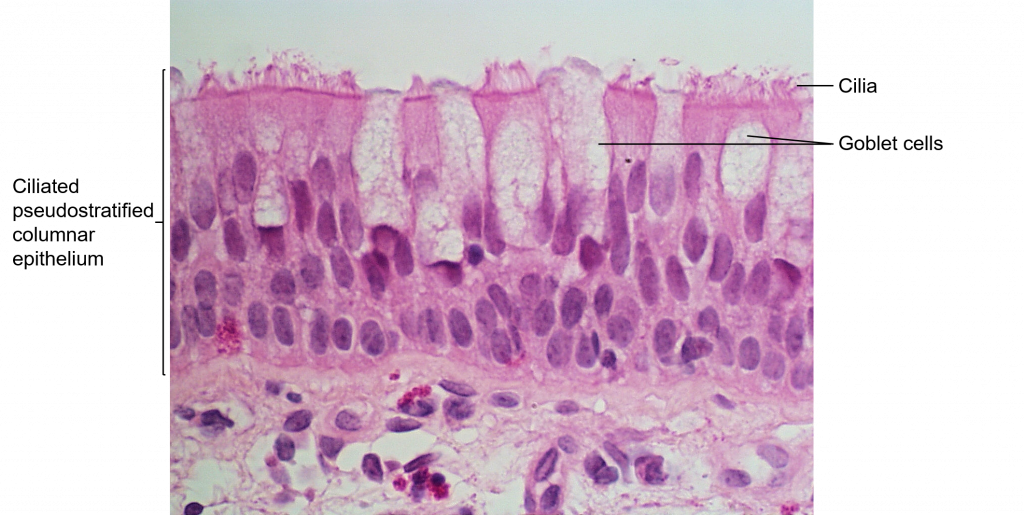 Figure 22.5 Ciliated Pseudostratified Columnar Epithelium Respiratory epithelium is ciliated pseudostratified columnar epithelium. Goblet cells provide lubricating mucus. LM × 680. [Attribution to Paul Shield, QUT]
Figure 22.5 Ciliated Pseudostratified Columnar Epithelium Respiratory epithelium is ciliated pseudostratified columnar epithelium. Goblet cells provide lubricating mucus. LM × 680. [Attribution to Paul Shield, QUT]
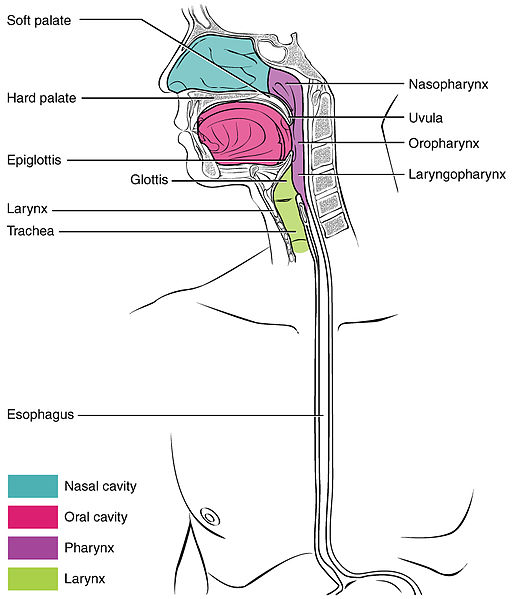
Pharynx
The pharynx is a tube formed by skeletal muscle and lined by mucous membrane that is continuous with that of the nasal cavities (see Figure 22.6). The pharynx is divided into three major regions: the nasopharynx, the oropharynx, and the laryngopharynx (Figure 22.6).
Figure 22.6 Divisions of the Pharynx The pharynx is divided into three regions: the nasopharynx, the oropharynx, and the laryngopharynx.
Larynx
The larynx is a cartilaginous structure inferior to the laryngopharynx that connects the pharynx to the trachea and helps regulate the volume of air that enters and leaves the lungs (Figure 22.7). The structure of the larynx is formed by several pieces of cartilage. Three large cartilage pieces—the thyroid cartilage (anterior), epiglottic cartilage (superior), and cricoid cartilage (inferior)—form the major structure of the larynx. The thyroid cartilage is the largest piece of hyaline cartilage that makes up the larynx. The thyroid cartilage consists of the laryngeal prominence, or “Adam’s apple,” which tends to be more prominent in males. The thick cricoid cartilage also consists of hyaline cartilage and forms a ring with a wide posterior region and a thinner anterior region. Smaller paired cartilages including the arytenoids attach to the epiglottis and the vocal cords and muscle that help move the vocal cords to produce speech.
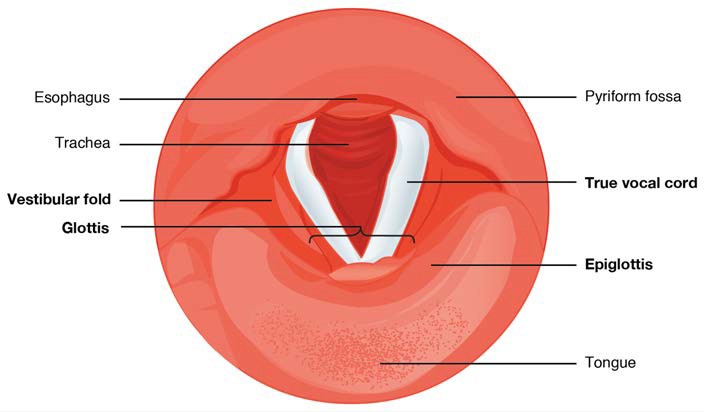
The epiglottic cartilage, attached to the thyroid cartilage, is a very flexible piece of elastic cartilage that covers the opening of the trachea (see Figure 22.6). When in the “closed” position, the unattached end of the epiglottis rests on the glottis. A vestibular fold, or false vocal cord, is one of a pair of folded sections of mucous membrane. A true vocal cord is one of the white, membranous folds attached by muscle to the thyroid and arytenoid cartilages of the larynx on their outer edges. The inner edges of the true vocal cords are free, allowing oscillation to produce sound. The space between the true vocal cords is called the glottis (Figure 22.8). The size of the membranous folds of the true vocal cords differs between individuals, producing voices with different pitch ranges. Folds in males tend to be larger than those in females, which create a deeper voice. The act of swallowing causes the pharynx and larynx to lift upward, allowing the pharynx to expand and the epiglottis of the larynx to swing downward, closing the opening to the trachea. These movements produce a larger area for food to pass through, while preventing food and beverages from entering the trachea.
Figure 22.8 Vocal Cords Superior view of the true vocal cords and vestibular folds of the larynx.
Continuous with the laryngopharynx, the superior portion of the larynx is lined with stratified squamous epithelium, transitioning into ciliated pseudostratified columnar epithelium that contains goblet cells. Similar to the nasal cavity and nasopharynx, this specialised epithelium produces mucus to trap debris and pathogens as they enter the trachea. The cilia beat the mucus upward towards the laryngopharynx, where it can be swallowed down the oesophagus.
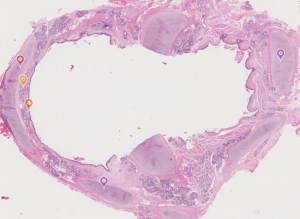
Trachea
The trachea (windpipe) extends from the larynx toward the lungs (Figure 22.9). The trachea is formed by 16 to 20 stacked, C-shaped pieces of hyaline cartilage that are connected by dense connective tissue. Muscle and connective tissue together form a flexible membrane that closes the posterior surface of the trachea, connecting the C-shaped cartilages to provide structural support and prevent the trachea from collapsing. The trachea is lined with pseudostratified ciliated columnar epithelium, which is continuous with the larynx. The oesophagus borders the trachea posteriorly.
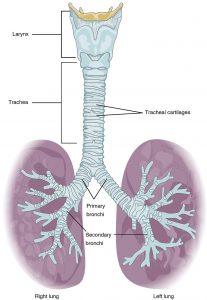
Figure 22.9 Trachea The tracheal tube is formed by stacked, C-shaped pieces of hyaline cartilage.
INTERACTIVE LINK
Bronchial Tree
The trachea branches into the right and left primary (main) bronchi. Like the trachea, these primary bronchi are lined by ciliated pseudostratified columnar epithelium containing mucus-producing goblet cells. Rings of cartilage, similar to those of the trachea, support the structure of the primary bronchi and prevent their collapse. The primary bronchi enter the lungs at the hilum, a concave region where blood vessels, lymphatic vessels, and nerves also enter the lungs, and then divide into secondary (lobar) bronchi. The secondary bronchi pass deep into the lung tissue and divide into tertiary (segmental) bronchi. The secondary and tertiary bronchi are also lined by ciliated pseudostratified columnar epithelium, however hyaline cartilage plates replace the rings of cartilage in the primary bronchi. The bronchi continue to branch into a bronchial tree. A bronchial tree (or respiratory tree) is the collective term used for these multiple-branched bronchi. The main function of the bronchi, like other conducting zone structures, is to provide a passageway for air to move into and out of each lung. In addition, the mucous membrane traps debris and pathogens.
A bronchiole branches from the tertiary bronchi. Bronchioles, which are about 1 mm in diameter, further branch until they become the tiny terminal bronchioles, which are the final part of the conducting zone. There are more than 1000 terminal bronchioles in each lung. The muscular walls of the bronchioles do not contain cartilage like those of the bronchi. This muscular wall can change the size of the tubing to increase or decrease airflow through the tube.
The respiratory zone begins where the terminal bronchioles join a respiratory bronchiole, the smallest type of bronchiole, which then leads to an alveolar duct, opening into a cluster of alveoli.
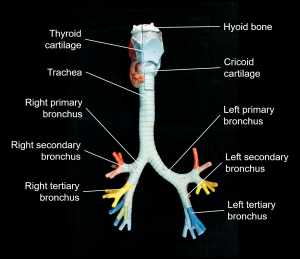
Figure XX Bronchial Tree The trachea bifurcates into the primary bronchi, which divide into the secondary bronchi and further divides into the tertiary bronchi.
INTERACTIVE LINK
The Lungs
Learning Objectives
By the end of this section, you will be able to:
- Identify and describe the features of the thoracic diaphragm
- Identify and describe the macroscopic features of the right and left lungs
- Summarise the blood flow pattern associated with the lungs
- Describe the visceral and parietal pleura and how it forms the pleural cavity
- Describe the histology and functional changes throughout the respiratory tract
A major organ of the respiratory system, each lung houses structures of both the conducting and respiratory zones. The main function of the lungs is to perform the exchange of oxygen and carbon dioxide with air from the atmosphere. To this end, the lungs exchange respiratory gases across a very large epithelial surface area—about 70 square metres—that is highly permeable to gases.
Gross Anatomy of the Lungs
The lungs are pyramid-shaped, paired organs that are connected to the trachea by the right and left bronchi; on the inferior surface, the lungs are bordered by the thoracic diaphragm. The thoracic diaphragm is the flat, dome-shaped muscle located at the base of the lungs and separates the thoracic and abdominal cavities. In order for the inferior vena cava to enter the thorax, it passes through the caval foramen in the thoracic diaphragm. To enter the abdomen, the descending aorta passes through the aortic hiatus of the thoracic diaphragm, and the oesophagus passes through the oesophageal hiatus of the diaphragm.
The lungs are enclosed by the pleurae, which are attached to the mediastinum. The right lung is shorter and wider than the left lung, and the left lung occupies a smaller volume than the right. The cardiac notch is an indentation on the surface of the left lung, and it allows space for the heart. The apex of the lung is the superior region, whereas the base is the opposite region near the thoracic diaphragm. The costal surface of the lung borders the ribs. The mediastinal surface faces the midline.
Each lung is composed of smaller units called lobes. Fissures separate these lobes from each other. The right lung consists of three lobes: the superior, middle, and inferior lobes. The horizontal fissure separates the right superior and middle lobes, and the oblique fissure separates the right middle and inferior lobes. The left lung consists of two lobes: the superior and inferior lobes. The oblique fissure separates the left superior and inferior lobes. A tongue-like extension of the left superior lobe projects anteriorly over the heart and is called the lingula of the left lung.
INTERACTIVE ACTIVITY
Blood Supply and Nervous Innervation of the Lungs
The blood supply of the lungs plays an important role in gas exchange and serves as a transport system for gases throughout the body. In addition, innervation by the both the parasympathetic and sympathetic nervous systems provides an important level of control through dilation and constriction of the airway.
Blood Supply
The major function of the lungs is to perform gas exchange, which requires blood from the pulmonary circulation. This blood supply contains deoxygenated blood and travels to the lungs where erythrocytes, also known as red blood cells, pick up oxygen to be transported to tissues throughout the body. The pulmonary artery is an artery that arises from the pulmonary trunk of the heart and carries deoxygenated blood to the alveoli. The pulmonary artery branches multiple times as it follows the bronchi, and each branch becomes progressively smaller in diameter. As they near the alveoli, the pulmonary arteries become the pulmonary capillary network. The pulmonary capillary network consists of tiny vessels with very thin walls that lack smooth muscle fibres. The capillaries branch and follow the bronchioles and structure of the alveoli. It is at this point that the capillary wall meets the alveolar wall, creating the respiratory membrane. Once the blood is oxygenated, it drains from the alveoli by way of multiple pulmonary veins, which exit the lungs through the hilum.
Nervous Innervation
Dilation and constriction of the airway are achieved through nervous control by the parasympathetic and sympathetic nervous systems. The parasympathetic system causes bronchoconstriction, whereas the sympathetic nervous system stimulates bronchodilation. Reflexes such as coughing, and the ability of the lungs to regulate oxygen and carbon dioxide levels, also result from this autonomic nervous system control.
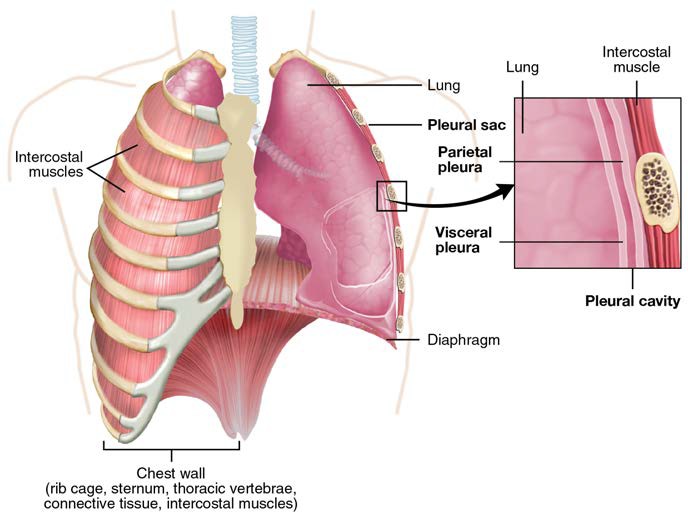
Pleura of the Lungs
Each lung is enclosed within a cavity that is surrounded by the pleura. The pleura (plural = pleurae) is a serous membrane that surrounds the lung. The right and left pleurae, which enclose the right and left lungs, respectively, are separated by the mediastinum. The pleurae consist of two layers. The visceral pleura is the layer that is superficial to the lungs, and extends into and lines the lung fissures (Figure 22.14). In contrast, the parietal pleura is the outer layer that connects to the thoracic wall, the mediastinum, and the thoracic diaphragm. The visceral and parietal pleurae connect to each other at the hilum. The pleural cavity is the space between the visceral and parietal layers.
The pleurae perform two major functions: they produce pleural fluid and create cavities that separate the major organs in the thoracic cavity. Pleural fluid lubricates to reduce the friction between the two layers to prevent trauma during breathing, and creates surface tension that helps maintain the position of the lungs against the thoracic wall. This adhesive characteristic of the pleural fluid causes the lungs to enlarge when the thoracic wall expands during ventilation, allowing the lungs to fill with air. The pleurae also create a division between major organs of the thoracic cavity that prevents interference due to the movement of the organs, while preventing the spread of infection.
Figure 22.14 Parietal and Visceral Pleurae of the Lungs
Thoracic Diaphragm
The thoracic diaphragm is the dome-shaped muscle located at the base of the lungs and separates the thoracic and abdominal cavities. Contraction of the thoracic diaphragm flattens its dome-shape to increase the size of the pleural cavity and create negative pressure to facilitate air movement into the lungs during inspiration. The thoracic diaphragm allows the passageway of a number of structures between the thoracic and abdominal cavities through three openings. The caval foramen carries the inferior vena cava from the abdomen to the thorax to empty blood into the right atrium of the heart. The oesophageal hiatus allows the oesophagus to enter the abdomen to empty food into the stomach. The aortic hiatus is the most posterior of the openings in the thoracic diaphragm allowing the descending aorta to travel from the thorax to the abdomen. It is at this point as it passes through the aortic hiatus that the thoracic aorta becomes the abdominal aorta.
Alveoli
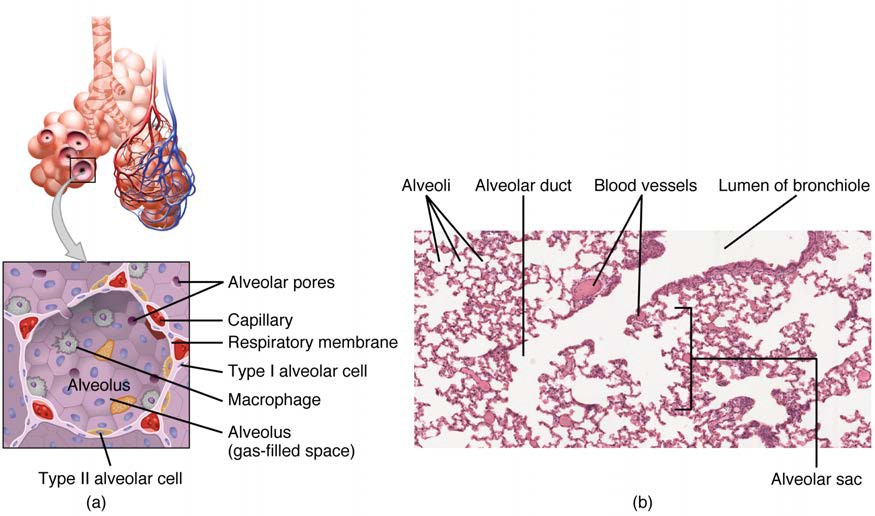
An alveolar duct is a tube composed of smooth muscle and connective tissue, which opens into a cluster of alveoli. An alveolus is one of the many small, grape-like sacs that are attached to the alveolar ducts.
An alveolar sac is a cluster of many individual alveoli that are responsible for gas exchange. An alveolus is approximately 200 μm in diameter with elastic walls that allow the alveolus to stretch during air intake, which greatly increases the surface area available for gas exchange.
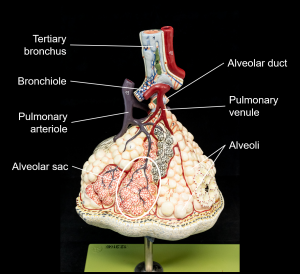
Figure 22.10 Respiratory Zone Bronchioles lead to alveolar sacs in the respiratory zone, where gas exchange occurs.
The alveolar wall consists of three major cell types: type I alveolar cells (pneumocyte), type II alveolar cells (pneumocyte), and alveolar macrophages. A type I alveolar cell is a squamous epithelial cell of the alveoli, which constitute up to 97% of the alveolar surface area. These cells are about 25 nm thick and are highly permeable to gases. A type II alveolar cell is interspersed among the type I cells and secretes pulmonary surfactant, a slippery substance to reduce the surface tension of the alveoli. Roaming around the alveolar wall is the alveolar macrophage, a phagocytic cell of the immune system that removes debris and pathogens that have reached the alveoli.
The simple squamous epithelium formed by type I alveolar cells is attached to a thin, elastic basement membrane. This epithelium is extremely thin and borders the endothelial membrane of capillaries. Taken together, the alveoli and capillary membranes form a respiratory membrane that is approximately 0.5 mm thick. The respiratory membrane allows gases to cross by simple diffusion, allowing oxygen to be picked up by the blood for transport and CO2 to be released into the air of the alveoli.
Figure 22.11 Structures of the Respiratory Zone (a) The alveolus is responsible for gas exchange. (b) A micrograph shows the alveolar structures within lung tissue. LM × 178. [Micrograph provided by the Regents of University of Michigan Medical School © 2012]
Key Terms
alveolar duct small tube that leads from the terminal bronchiole to the respiratory bronchiole and is the point of attachment for alveoli
alveolar macrophage immune system cell of the alveolus that removes debris and pathogens
alveolar pore opening that allows airflow between neighboring alveoli
alveolar sac cluster of alveoli
alveolus small, grape-like sac that performs gas exchange in the lungs
bronchial tree collective name for the multiple branches of the bronchi and bronchioles of the respiratory system
bronchiole branch of bronchi that are 1 mm or less in diameter and terminate at alveolar sacs
bronchoconstriction decrease in the size of the bronchiole due to contraction of the muscular wall
bronchodilation increase in the size of the bronchiole due to contraction of the muscular wall
bronchus tube connected to the trachea that branches into many subsidiaries and provides a passageway for air to enter and leave the lungs
cardiac notch indentation on the surface of the left lung that allows space for the heart
conducting zone region of the respiratory system that includes the organs and structures that provide passageways for air and are not directly involved in gas exchange
cricoid cartilage portion of the larynx composed of a ring of cartilage with a wide posterior region and a thinner anterior region; attached to the oesophagus
epiglottis leaf-shaped piece of elastic cartilage that is a portion of the larynx that swings to close the trachea during swallowing
expiration (also, exhalation) process that causes the air to leave the lungs
external nose region of the nose that is easily visible to others
glottis opening between the vocal folds through which air passes when producing speech
hilum concave structure on the mediastinal surface of the lungs where blood vessels, lymphatic vessels, nerves, and a bronchus enter the lung
inspiration (also, inhalation) process that causes air to enter the lungs
laryngeal prominence region where the two lamina of the thyroid cartilage join, forming a protrusion known as “Adam’s apple”
laryngopharynx portion of the pharynx bordered by the oropharynx superiorly and esophagus and trachea inferiorly; serves as a route for both air and food
larynx cartilaginous structure that produces the voice, prevents food and beverages from entering the trachea, and regulates the volume of air that enters and leaves the lungs
lingual tonsil lymphoid tissue located at the base of the tongue
lung organ of the respiratory system that performs gas exchange
meatus one of three recesses (superior, middle, and inferior) in the nasal cavity attached to the conchae that increase the surface area of the nasal cavity
naris (plural = nares) opening of the nostrils
nasal bone bone of the skull that lies under the root and bridge of the nose and is connected to the frontal and maxillary bones
nasal septum wall composed of bone and cartilage that separates the left and right nasal cavities
nasopharynx portion of the pharynx flanked by the conchae and oropharynx that serves as an airway
oropharynx portion of the pharynx flanked by the nasopharynx, oral cavity, and laryngopharynx that is a passageway for both air and food
palatine tonsil one of the paired structures composed of lymphoid tissue located anterior to the uvula
paranasal sinus one of the cavities within the skull that is connected to the conchae that serve to warm and humidify incoming air, produce mucus, and lighten the weight of the skull; consists of frontal, maxillary, sphenoidal, and ethmoidal sinuses
parietal pleura outermost layer of the pleura that connects to the thoracic wall, mediastinum, and diaphragm
pharyngeal tonsil structure composed of lymphoid tissue located in the nasopharynx
pharynx region of the conducting zone that forms a tube of skeletal muscle lined with respiratory epithelium; located between the nasal conchae and the esophagus and trachea
pleural cavity space between the visceral and parietal pleurae
pleural fluid substance that acts as a lubricant for the visceral and parietal layers of the pleura during the movement of breathing
pulmonary artery artery that arises from the pulmonary trunk and carries deoxygenated, arterial blood to the alveoli
pulmonary surfactant substance composed of phospholipids and proteins that reduces the surface tension of the alveoli; made by type II alveolar cells
respiratory bronchiole specific type of bronchiole that leads to alveolar sacs
respiratory epithelium ciliated lining of much of the conducting zone that is specialised to remove debris and pathogens, and produce mucus
respiratory membrane alveolar and capillary wall together, which form an air-blood barrier that facilitates the simple diffusion of gases
root region of the external nose between the eyebrows
thyroid cartilage largest piece of cartilage that makes up the larynx and consists of two lamina
trachea tube composed of cartilaginous rings and supporting tissue that connects the lung bronchi and the larynx; provides a route for air to enter and exit the lung
true vocal cord one of the pair of folded, white membranes that have a free inner edge that oscillates as air passes through to produce sound
type I alveolar cell squamous epithelial cells that are the major cell type in the alveolar wall; highly permeable to gases
type II alveolar cell cuboidal epithelial cells that are the minor cell type in the alveolar wall; secrete pulmonary surfactant
vestibular fold part of the folded region of the glottis composed of mucous membrane; supports the epiglottis during swallowing
visceral pleura innermost layer of the pleura that is superficial to the lungs and extends into the lung fissures