Chapter 7: SKELETAL SYSTEM
Introduction

Plain Radiography of the Hand. Medical imaging provides a non-invasive way of viewing the skeleton. Here you can see the invidivual bones of the carpus (wrist) and hand and the sites of the mobile joints lying between adjacent bones. [Attribution to Mikael Haggstrom, Wikimedia Commons]
Chapter Objectives
After studying this chapter, you will be able to:
- List and describe the functions of bones
- Describe the macroscopic appearance of bones
- Discuss the process of bone formation and development
- Describe the classification and movement of joints
- Describe the major morphological features of the bones of the axial and appendicular skeletons
The term skeleton does not only describe the many bones of the human body but also includes the small ligaments and cartilages which help to link adjacent bones and form joints or arthroses. The anatomy of the skeleton therefore requires an understanding of osteology, the study of bones, and arthrology, the study of joints. Whilst the skeleton may appear dry and inert, the skeleton is a structure of living tissue that grows, repairs, and renews itself. The bones within it are dynamic and complex organs that serve a number of important functions, including essential functions in protection of critical organs and facilitating body movement.
The skeletal system includes all of the bones, cartilages and ligaments of the body that support and give shape to the body and body structures. For adults, there are 206 bones in the skeleton. Younger individuals have higher numbers of bones because some bones fuse together during childhood and adolescence to form an adult bone. The primary functions of the skeleton are to provide a rigid, internal structure that can support the weight of the body against the force of gravity, and to provide a structure upon which muscles can act to produce movements of the body. The inferior portion of the skeleton is specialised for stability during walking or running. In contrast, the superior part of the skeleton has greater mobility and ranges of motion, features that allow you to lift and carry objects or turn your head and trunk. The bones of the skeleton also serve as the primary storage site for important minerals such as calcium and phosphate. The bone marrow found within bones stores fat and houses the blood-cell producing (haematopoetic) tissue of the body.
Functions of the Skeletal System
Learning Objectives
By the end of this section, you will be able to:
- List the functions of the skeletal system
- Describe how bone, cartilage and ligaments contribute to the functions of the skeletal system
Bone, or osseous tissue, is a hard, dense connective tissue that forms most of the adult skeleton, the support structure of the body. In the areas of the skeleton where bones move (for example, the ribcage and joints), cartilage, a semi-rigid form of connective tissue, provides flexibility and smooth surfaces for movement. The skeletal system is the body system composed of bones, cartilage, ligaments and joints and performs the following critical functions for the human body:
- supports the body
- facilitates movement
- protects internal organs
- produces blood cells
- stores and releases minerals and fat
Support, Movement and Protection
The most apparent functions of the skeletal system are the gross functions—those visible by observation. Simply by looking at a person, you can see how the bones support, facilitate movement, and protect the human body. Just as the steel beams of a building provide a scaffold to support its weight, the bones and cartilage of your skeletal system compose the scaffold that supports the rest of your body. Without the skeletal system, you would be a limp mass of organs, muscle, and skin.
Bones protect internal organs from injury by covering or surrounding them. For example, your ribs and sternum protect your lungs and heart, the bones of your vertebral column protect your spinal cord, and the bones of your cranium (skull) protect your brain (Figure 6.3).
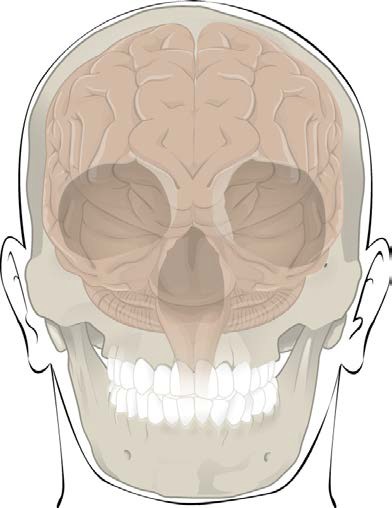
Figure 6.3 Bones Protect Brain The cranium completely surrounds and protects the brain from non-traumatic injury.
Bones also facilitate movement by serving as points of attachment for your muscles. While some bones only serve as a support for the muscles, others also transmit the forces produced when your muscles contract. From a mechanical point of view, bones act as levers and joints serve as fulcrums. Unless a muscle spans a joint and contracts, a bone is not going to move.
INTERACTIVE ACTIVITY
Play the animated video from Anatomy.TV (Primal Pictures) demonstrating the action of the biceps brachii in flexing the elbow and triceps brachii in extending the elbow. Note how the muscles cross the elbow joint to insert onto the radius and ulna, respectively, to exert their actions on the elbow joint. (Use fullscreen view if you have any problems visualising the model)
Note: In order for the embedded Anatomy.TV content to open and run correctly, you first need to click the following link to login to the Anatomy.TV database from the QUT library – it will open in a new tab, so leave that tab open in the background. When you return to this page, you may then need to refresh it (press the F5 key).
Each bone of the body serves a particular function, and therefore bones vary in size, shape, and strength based on these functions. For example, the bones of the inferior back (lumbar vertebrae) and lower limb are thick and strong to support your body weight. Similarly, the size of a bony landmark that serves as a muscle attachment site on an individual bone is related to the strength of this muscle. Muscles can apply very strong pulling forces to the bones of the skeleton. To resist these forces, bones have enlarged bony landmarks at sites where powerful muscles attach. This means that not only the size of a bone, but also its shape, is related to its function. For this reason, the identification of bony landmarks is important during your study of the skeletal system.
Bones are also dynamic organs that can modify their strength and thickness in response to changes in muscle strength or body weight. Thus, muscle attachment sites on bones will thicken if you begin a workout program that increases muscle strength. Similarly, the walls of weight-bearing bones will thicken if you gain body weight or begin pounding the pavement as part of a new running regimen. In contrast, a reduction in muscle strength or body weight will cause bones to become thinner. This may happen during a prolonged hospital stay, following limb immobilisation in a cast, or going into the weightlessness of outer space. Even a change in diet, such as eating only soft food due to the loss of teeth, will result in a noticeable decrease in the size and thickness of the jaw bones.
Cartilage of the skeleton provides flexible strength and support for body structures such as the thoracic cage, the external ear, and the trachea and larynx. At joints of the body, cartilage can also unite adjacent bones or provide cushioning between them. Ligaments are the strong connective tissue bands that hold the bones at a moveable joint together and serve to prevent excessive movements of the joint that would result in injury. Ligaments are defined as dense regular connective tissue bands that band between two bones or bone surfaces (in contrast tendons are part of a skeletal muscle organ and connect muscle fibres to bone).
Mineral Storage, Energy Storage and Haematopoiesis
On a metabolic level, bone tissue performs several critical functions. For one, the bone matrix acts as a reservoir for a number of minerals important to the functioning of the body, especially calcium and phosphorus. These minerals, incorporated into bone tissue, can be released back into the bloodstream to maintain levels needed to support physiological processes. Calcium ions, for example, are essential for muscle contractions and controlling the flow of other ions involved in the transmission of nerve impulses.
Bone also serves as a site for fat storage and blood cell production. The softer connective tissue that fills the interior of most bone is referred to as bone marrow (Figure 6.5). There are two types of bone marrow: yellow bone marrow and red bone marrow. Yellow bone marrow contains adipose tissue; the triglycerides stored in the adipocytes of the tissue can serve as a source of energy. Red bone marrow is where haematopoiesis—the production of blood cells—takes place. Erythrocytes (red blood cells), leucocytes (white blood cells), and platelets are all produced in the red bone marrow.
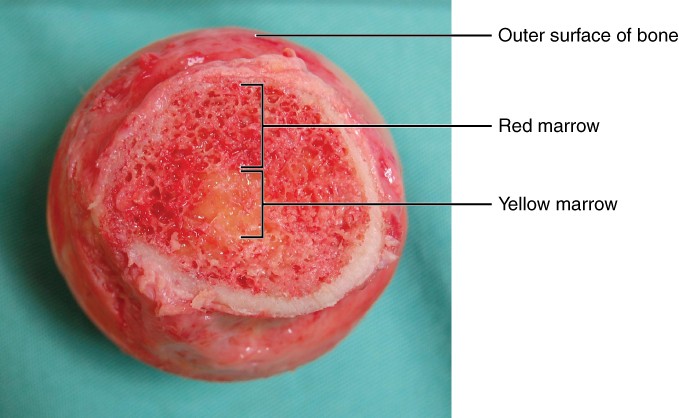
Figure 6.5 Head of Femur Showing Red and Yellow Bone Marrow The head of the femur contains both yellow and red bone marrow. Yellow bone marrow stores fat. Red bone marrow is responsible for haematopoiesis. [Modification of work by “stevenfruitsmaak”/Wikimedia Commons]
Macroscopic Appearance of Bones
Learning Objectives
By the end of this section, you will be able to:
- Classify bones according to their shapes
- Describe the function of each category of bones
- Describe how cortical and trabecular bone tissue contribute to the structure of bones
- Describe how bones are nourished
Bone Classification
The 206 typical bones that compose the adult skeleton are divided into four categories based on their shape: long, short, flat and irregular (Figure 6.6). Their shape and their function are related such that each categorical shape of bone has a distinct function.
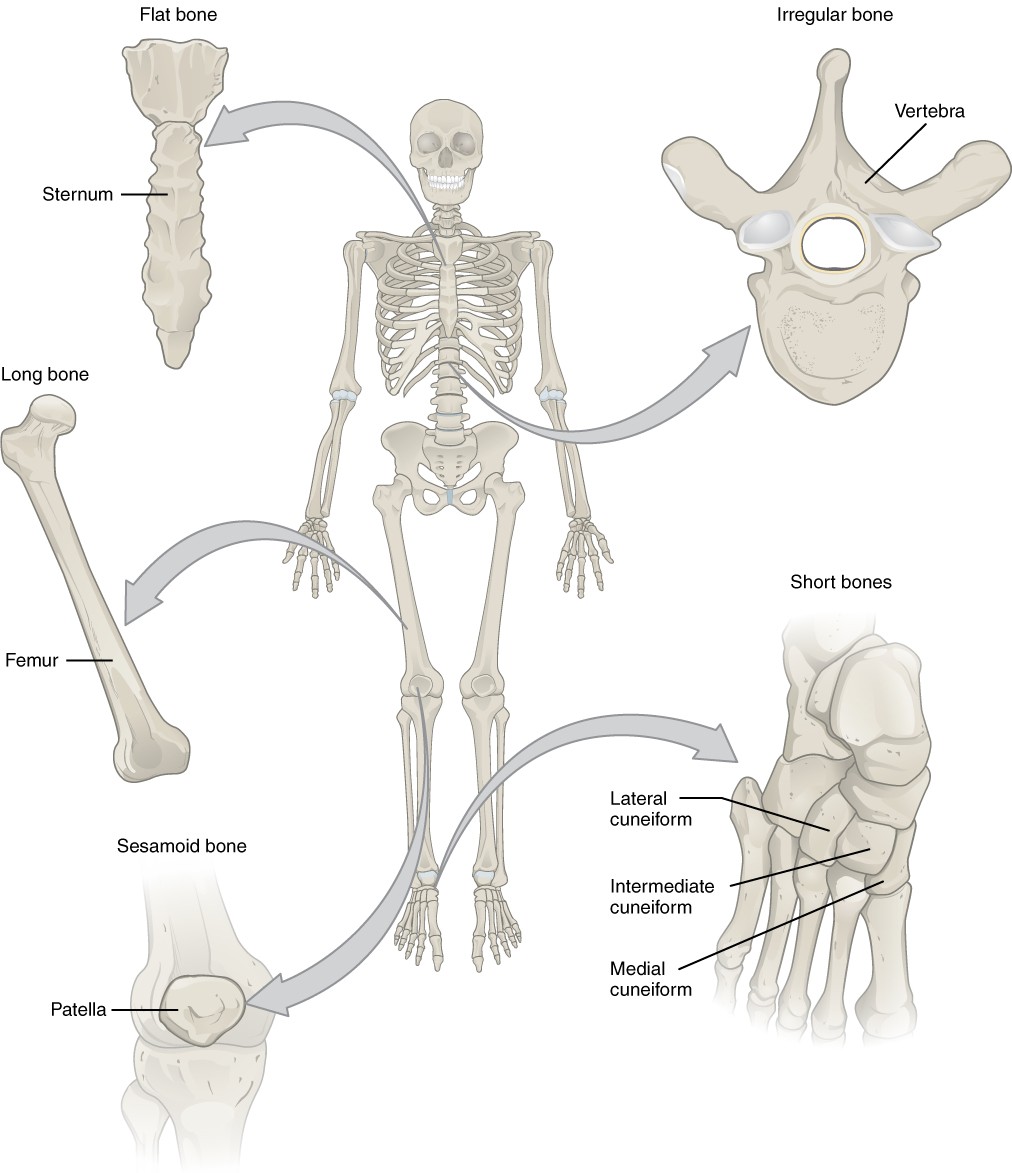
Figure 6.6 Classification of Bones by Shape Examples of a bone in each shape category are provided.
Table 6.1 reviews bone classifications with their associated features, functions, and examples.
Table 6.1 Bone Classifications
| Bone classification | Features | Function(s) | Examples |
| Long | Cylinder-like shape, longer than it is wide | Leverage | Femur, tibia, fibula, metatarsals, humerus, ulna, radius, metacarpals, phalanges |
| Short | Cube-like shape, approximately equal in length, width, and thickness | Provide stability, support, while allowing for some motion | Carpals, tarsals |
| Flat | Thin and curved | Points of attachment for muscles; protectors of internal organs | Sternum, ribs, scapulae, cranial bones |
| Irregular | Complex shape | Protect internal organs | Vertebrae, facial bones, os coxa (hip bone) |
| Sesamoid | Small and round; embedded in tendons | Protect tendons from wear and tear (shear forces) and increase lever of muscle action | Patellae |
Organisation of a Bone Organ
The structure of a long bone allows for the best visualisation of all of the parts of a bone organ (Figure 6.7). The term bone organ acknowledges that a bone does not only consist of bone tissue but other connective tissue derivatives including cartilaginous and connective tissue proper, adipose tissue and fluid connective tissue. These other connective tissue structures include the articular cartilage which line the joint surfaces of a bone, the dense irregular connective tissue of the periosteum and endosteum that line the non-joint bone surfaces, the yellow bone marrow and red bone marrow.
We will examine the structure of a long bone as an example of a bone organ. A long bone has two parts: the diaphysis and the epiphysis. The diaphysis is the tubular shaft that runs between the proximal and distal ends of the bone. The hollow region in the diaphysis is called the medullary cavity, which is filled with yellow bone marrow in the adult. The walls of the diaphysis are composed of dense and hard cortical bone tissue. The wider section at each end of the bone is called the epiphysis (plural = epiphyses), which is filled with trabecular bone tissue. Red bone marrow fills the spaces in the trabecular bone tissue. Each epiphysis meets the diaphysis at the metaphysis (the part of the diaphysis closest to the epiphysis). At the junction between the epiphysis and metaphysis the epiphyseal plate (growth plate), a layer of hyaline (transparent) cartilage can be found in a growing bone in a child. When the bone stops growing in early adulthood (approximately 18–21 years), the cartilage is replaced by osseous tissue and the epiphyseal plate becomes an epiphyseal line (as seen in Figure 6.7).
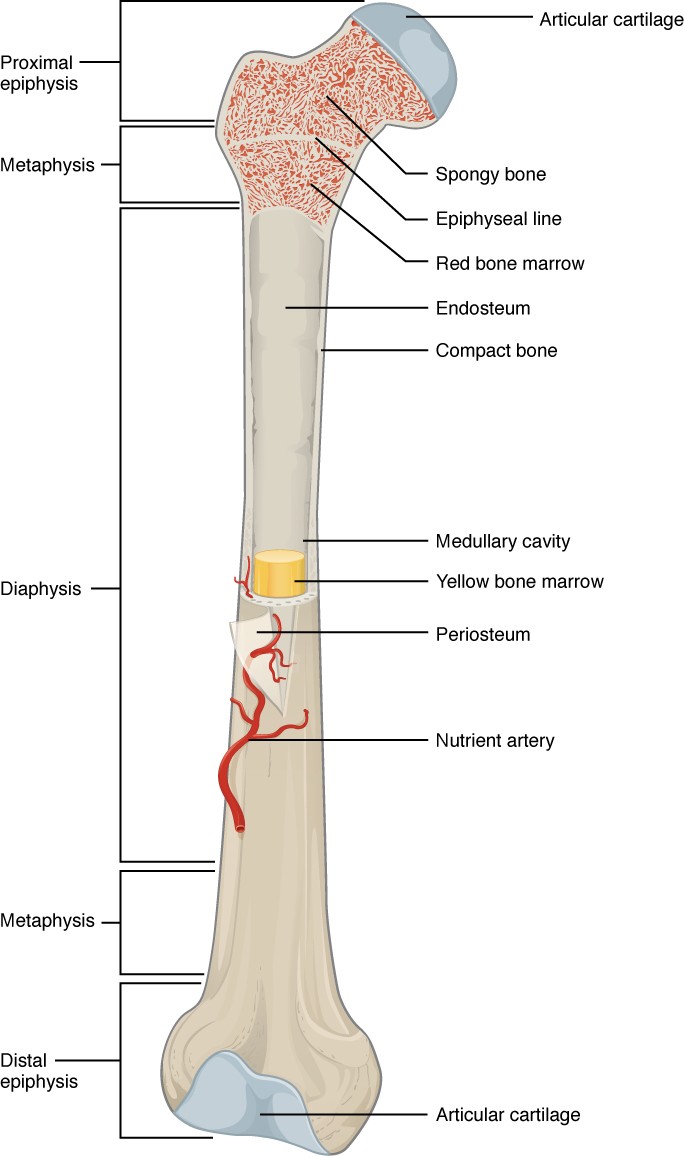
Figure 6.7 Anatomy of a Long Bone A typical long bone shows the macroscopic anatomical characteristics of bone.
The medullary cavity has a delicate membranous lining composed of dense irregular connective tissue called the endosteum (end- = “inside”; oste- = “bone”), where bone growth, repair, and remodelling occur. The external surface of the bone is covered with a similar dense irregular connective tissue membrane called the periosteum (peri- = “around” or “surrounding”). The periosteum contains blood vessels, nerves, and lymphatic vessels that nourish the cortical bone tissue. Tendons and ligaments also attach to bones at the periosteum. The periosteum covers the entire external surface except where the epiphyses meet other bones to form joints (Figure 6.8). In this region, the epiphyses are covered with articular cartilage, a thin layer of hyaline cartilage that reduces friction and acts as a shock absorber.
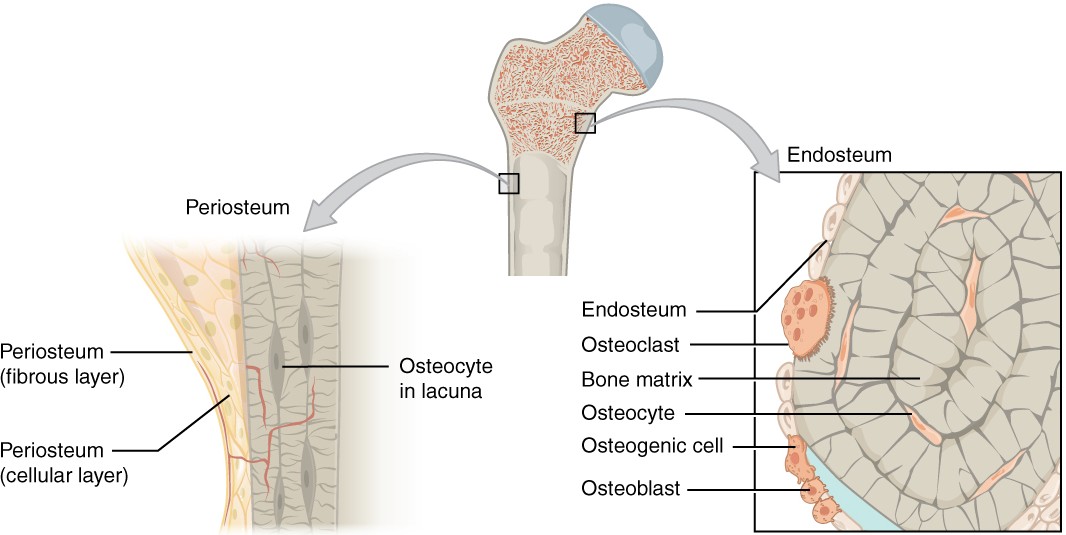
Figure 6.8 Periosteum and Endosteum The periosteum forms the outer surface of bone, and the endosteum lines the medullary cavity.
The trabecular bone tissue and medullary cavity receive nourishment from arteries that pass through the cortical bone tissue. The arteries enter through the nutrient foramen (plural = foramina), small openings in the diaphysis (Figure 6.15). The osteocytes in trabecular bone tissue are nourished by blood vessels of the periosteum and via blood that circulates in the bone marrow. As the blood passes through the marrow cavities, it is collected by veins, which then pass out of the bone through the foramina.
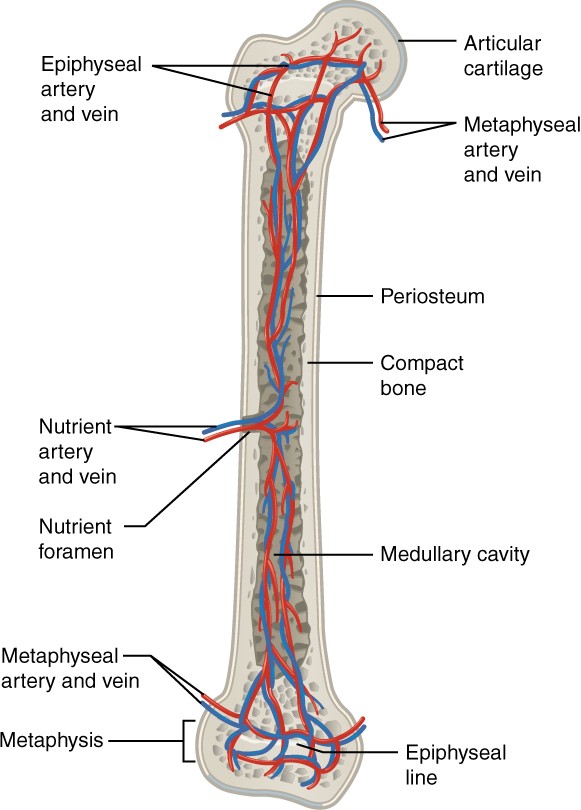
Figure 6.15 Diagram of Blood Supply to Bone Blood vessels enter the bone through the nutrient foramen.
Bone Formation and Development
Learning Objectives
By the end of this section, you will be able to:
- Explain the function of cartilage
- List the steps of intramembranous ossification
- List the steps of endochondral ossification
- Explain the growth activity at the epiphyseal plate
- Compare and contrast the processes of modelling and remodelling
In the early stages of embryonic development, the embryo’s skeleton consists of fibrous membranes and hyaline cartilage. By the sixth or seventh week of embryonic life, the actual process of bone development, ossification, begins. There are two osteogenic pathways—intramembranous ossification and endochondral ossification—but bone is the same regardless of the pathway that produces it. Bone requires a model tissue on which to lay down its mineral matrix; this may be a fibrous membrane (intramembranous ossification) or a cartilage template (endochondral ossification). For skeletal development, the most common template is cartilage. During foetal development, a framework is laid down that determines where bones will form. Throughout foetal development and into childhood growth and development, bone forms on the cartilaginous matrix. By the time a foetus is born, most of the cartilage has been replaced with bone. Some additional cartilage will be replaced throughout childhood, and some cartilage remains in the adult skeleton.
Regardless of which type of ossification a bone forms from the first site of bone ossification is termed the primary ossification centre. Most primary ossification centres appear before birth in the central part of each developing bone. In long bones the primary centres occur in the diaphysis and in the body or central part of the bone for irregular and short bones. Most bones have only one primary ossification centre (such as long bones), but some irregular bones such as the os coxa (hip bone) and vertebrae have multiple primary ossification centres that appear simultaneously. Bones that form from endochondral ossification, can then have additional sites of ossification at the ends/peripheral sites of the bone. These are known as secondary ossification centres and they typically appear postnatally, many forming around the time of puberty.
How Bones Grow
The epiphyseal plate is the area of growth in a long bone. It is a layer of hyaline cartilaginous tissue where endochondral ossification occurs in immature bones. On the epiphyseal side of the epiphyseal plate, cartilage is formed. On the diaphyseal side, cartilage is ossified, and the diaphysis grows in length – this is called longitudinal growth. Bones continue to grow in length until early adulthood. The rate of growth is controlled by hormones. When the chondrocytes in the epiphyseal plate cease their proliferation and bone replaces the cartilage, longitudinal growth stops. All that remains of the epiphyseal plate is an osseous scar called the epiphyseal line (Figure 6.19).
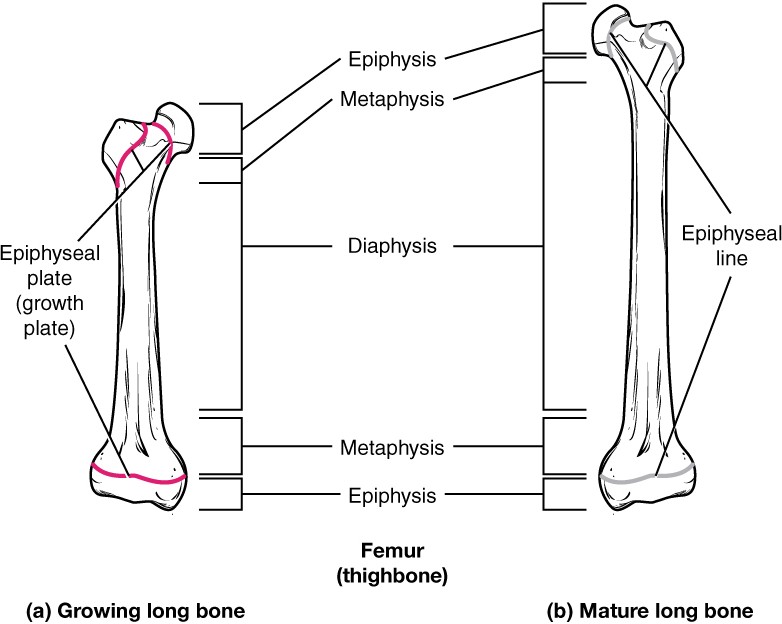
Figure 6.19 Progression from Epiphyseal Plate to Epiphyseal Line As a bone matures, the epiphyseal plate progresses to an epiphyseal line. (a) Epiphyseal plates are visible in a growing bone. (b) Epiphyseal lines are the remnants of epiphyseal plates in a mature bone.
While bones are increasing in length, they are also increasing in diameter; growth in diameter can continue even after longitudinal growth ceases. This is called appositional growth. Osteoclasts resorb old bone that lines the medullary cavity, while osteoblasts, via intramembranous ossification, produce new bone tissue deep to the periosteum. The erosion of old bone along the medullary cavity and the deposition of new bone deep to the periosteum not only increase the diameter of the diaphysis but also increase the diameter of the medullary cavity. This process is called bone modelling.
Bone Remodelling
The process in which matrix is resorbed on one surface of a bone and deposited on another is known as bone modelling. Modelling primarily takes place during bone growth. However, in adult life, bone undergoes remodelling, in which osetoclasts resorb old or damaged bone followed by osteoblasts laying down new bone to replace the bone that was resorbed. Injury, exercise, and other activities can activate bone remodelling, however bone remodelling is an ongoing activity as part of calcium homeostasis. The regular resorption of bone tissue releases calcium into the bloodstream to be used throughout the body in metabolic processes. This daily and ongoing process relies on the regular dietary intake of calcium to maintain high calcium levels in the mineralisation of bone tissue during the replacement of resorbed bone tissue.
Bone Markings
Learning Objectives
By the end of this section, you will be able to:
- Define and list examples of bone markings
Bone Markings
The surface features of bones vary considerably, depending on the function and location in the body. There are three general classes of bone markings: (1) articulations, (2) projections, and (3) depressions. As the name implies, an articulation is where two bone surfaces come together (articulus = “joint”). These surfaces tend to conform to one another, such as one being rounded and the other cupped, to facilitate the movement of the articulation. A projection is an area of a bone that projects out from the surface of the bone. These are the attachment points for tendons and ligaments. In general, their size and shape is an indication of the forces exerted through the attachment to the bone. A depression is an hole or groove in the bone that allows blood vessels and nerves to course around or through a bone. As with the other markings, their size and shape reflect the size of the vessels and nerves that penetrate the bone at these points. There are many specific examples of each of these bone marking categories as described in Table 6.2 and illustrated in Figure 6.10.
Table 6.2 Bone Markings
| Marking | Description | Example |
| Articulations | Where two bones meet | |
| Head | Prominent rounded surface (ball-like) | Head of femur |
| Facet | Flat surface | Vertebrae (inferior and superior articular facets) |
| Condyle | Rounded convex surface | Femoral condyles |
| Projections | Raised markings | |
| Protuberance | Roughened elevation | external occipital protuberance |
| Process | Prominent projection, often elongated | Spinous process of vertebra |
| Spine | Pointed process | Ischial spine of os coxa (hip bone) |
| Tubercle | Small, rounded process | Greater and lesser tubercles of humerus |
| Tuberosity | Rough surface | Deltoid tuberosity of humerus |
| Crest | Ridge | Iliac crest of os coxa (hip bone) |
| Depressions | Passageway or indent | |
| Fossa | Elongated basin | Iliac fossa of os coxa (hip bone) |
| Sulcus | Groove | Intertubercular sulcus of humerus |
| Canal | Passage in bone | Optic canal of frontal bone |
| Fissure | Slit through bone | Superior orbital fissure |
| Foramen | Hole through bone | Foramen magnum in the occipital bone |
| Meatus | Opening into canal | External auditory meatus |
| Sinus | Air-filled space in bone | Frontal sinus |
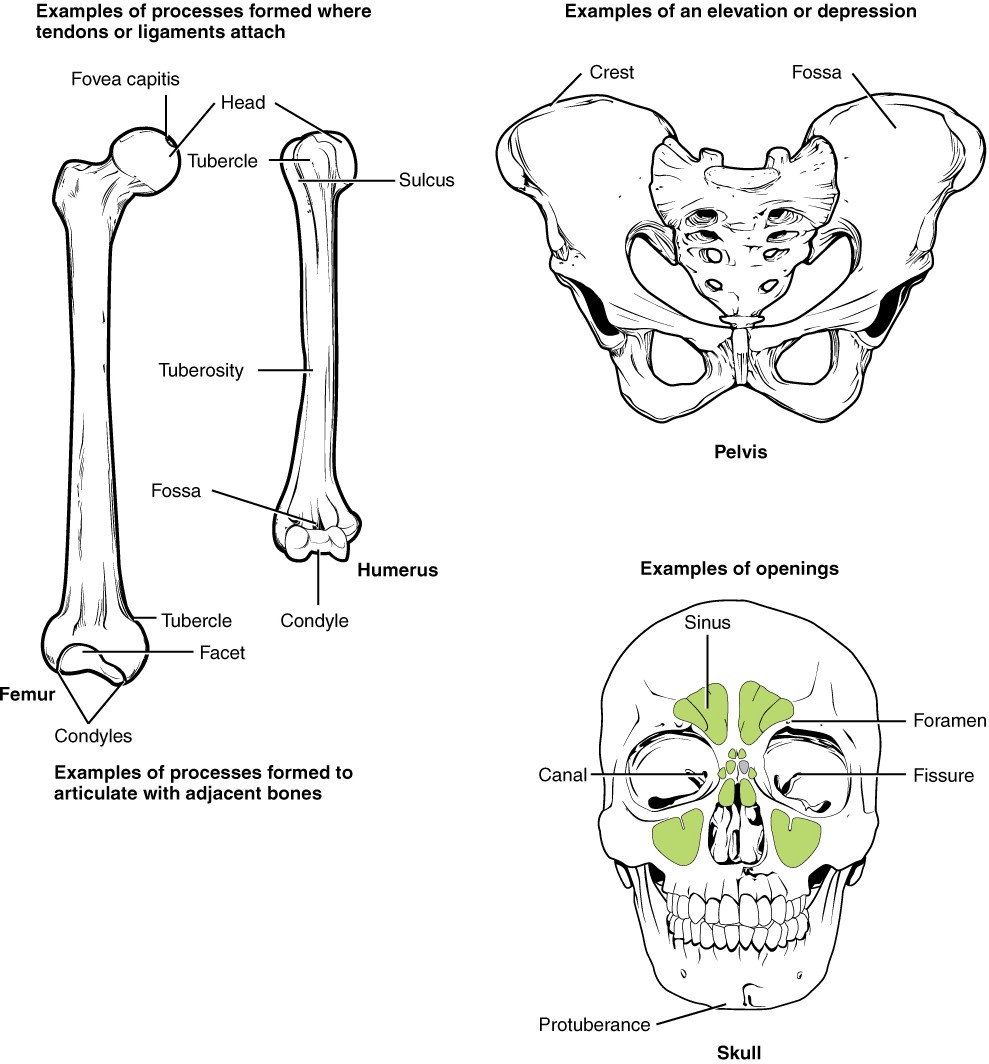
Figure 6.10 Bone Features The surface features of bones depend on their function, location, attachment of ligaments and tendons, or the penetration of blood vessels and nerves.
Divisions of the Skeletal System
Learning Objectives
By the end of this section, you will be able to:
- Distinguish between the axial skeleton and appendicular skeleton
- Define the axial skeleton and its components
- Define the appendicular skeleton and its components
The skeleton is subdivided into two major divisions—the axial and appendicular (Figure 7.2).
Your skeleton provides the internal supporting structure of the body. The adult axial skeleton consists of 80 bones that form the head and body trunk. Attached to this are the limbs, whose 126 bones constitute the appendicular skeleton. These bones are divided into two groups: the bones that are located within the limbs themselves, and the girdle bones that attach the limbs to the axial skeleton. The bones of the shoulder region form the pectoral girdle, which anchors the upper limb to the thoracic cage of the axial skeleton. The lower limb is attached to the vertebral column by the pelvic girdle.
Because of our upright stance, different functional demands are placed upon the upper and lower limbs. Thus, the bones of the lower limbs are adapted for weight-bearing, support and stability, as well as for body locomotion via walking or running. In contrast, our upper limbs are not required for these functions. Instead, our upper limbs are highly mobile and can be utilised for a wide variety of activities. The large range of upper limb movements, coupled with the ability to easily manipulate objects with our hands and opposable thumbs, has allowed humans to construct the modern world in which we live.
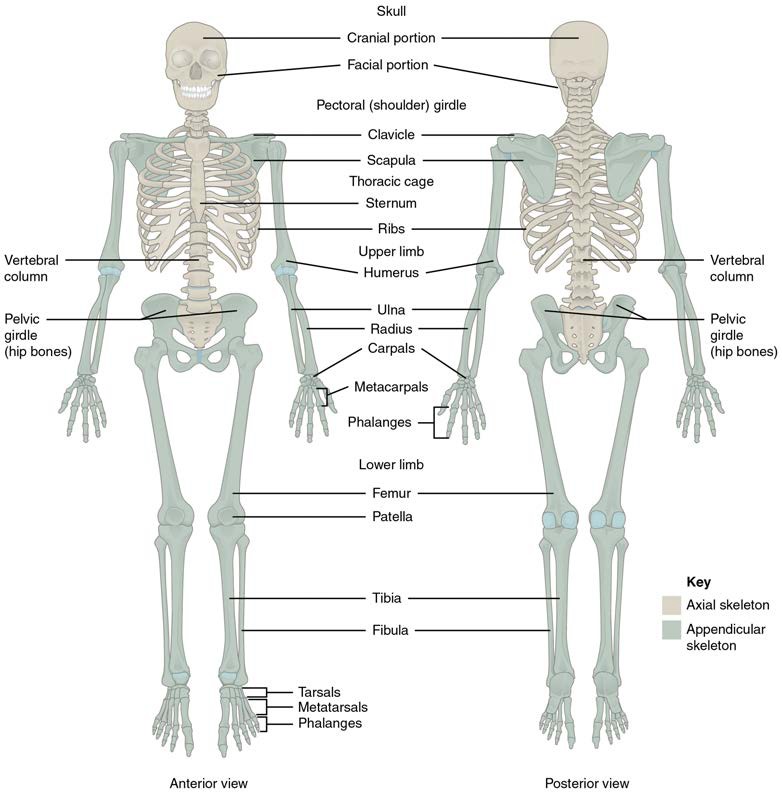
Figure 7.2 Axial and Appendicular Skeleton The axial skeleton supports the head, neck, back and thorax and thus forms the vertical axis of the body. It consists of the skull, vertebral column (including the sacrum and coccyx), and the thoracic cage, formed by the ribs and sternum. The appendicular skeleton is made up of all bones of the upper and lower limbs.
Axial: The Skull
Learning Objectives
By the end of this section, you will be able to:
- List and identify the major bones of the cranial and facial skeleton
- Locate the major sutures of the skull and name the bones associated with each
- Define the paranasal sinuses and identify the location of each
- Identify the bones and structures that form the nasal septum and nasal conchae, and locate the hyoid bone
- Identify the major bony openings of the skull
The skull is the skeletal structure of the head that supports the face and protects the brain. It is subdivided into the facial bones and the cranial bones (Figure 7.3). The facial bones form the nasal cavity, enclose the eyeballs, and support the teeth of the upper and lower jaws. The rounded cranial bones surround and protect the brain and house the middle and inner ear structures.
In the adult, the skull consists of 22 individual bones, 21 of which are immobile and united into a single unit (the cranium). The 22nd bone is the mandible (lower jaw), which is the only moveable bone of the skull. The term cranium then is used to describe all bones of the skull except for the mandible.
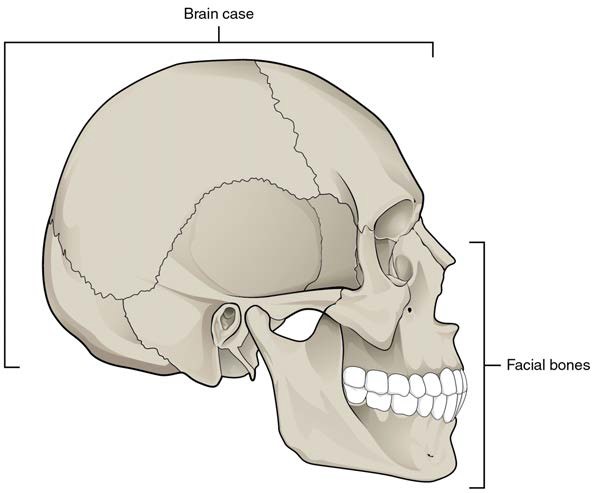
Figure 7.3 Parts of the Skull The skull consists of the rounded cranial bones that houses the brain and the facial bones that form the upper and lower jaws, nose, orbits, and other facial structures.
INTERACTIVE ACTIVITY
Sutures of the Skull
A suture is an immobile joint between adjacent bones of the skull. The narrow gap between the bones is filled with dense, fibrous connective tissue that unites the bones. The long sutures located between the cranial bones are not straight, but instead follow irregular, tightly twisting paths. These twisting lines serve to tightly interlock the adjacent bones, thus adding strength to the skull for brain protection.
The two suture lines seen on the superior aspect of the skull are the coronal and sagittal sutures. The coronal suture runs from side to side across the skull, within the coronal plane of section (see Figure 7.5). It joins the frontal bone to the right and left parietal bones. The sagittal suture extends posteriorly from the coronal suture, running along the midline at the superior aspect of the skull in the sagittal plane of section (see Figure 7.9). It unites the right and left parietal bones. On the posterior skull, the sagittal suture terminates by joining the lambdoidal suture. The lambdoidal suture extends inferiorly and laterally to either side away from its junction with the sagittal suture. The lambdoidal suture joins the occipital bone to the right and left parietal and temporal bones. This suture is named for its upside-down “V” shape, which resembles the capital letter version of the Greek letter lambda (Λ). The squamousal suture is located on the lateral skull. It unites the squamous portion of the temporal bone with the parietal bone (see Figure 7.5).
Development of the Skull
As the cranial bones grow in the foetal skull, they remain separated from each other by large areas of dense connective tissue, each of which is called a fontanelle (Figure 7.33). The fontanelles are the soft spots on an infant’s head. They are important during birth because these areas allow the skull to change shape as it squeezes through the birth canal. After birth, the fontanelles allow for continued growth and expansion of the skull as the brain enlarges. The largest fontanelle is located on the anterior head, at the junction of the frontal and parietal bones. The fontanelles decrease in size and disappear by approximately 2 years of age. However, the skull bones remain separated from each other at the sutures, which contain dense fibrous connective tissue that unites the adjacent bones. The connective tissue of the sutures allows for continued growth of the skull bones as the brain enlarges during childhood growth.
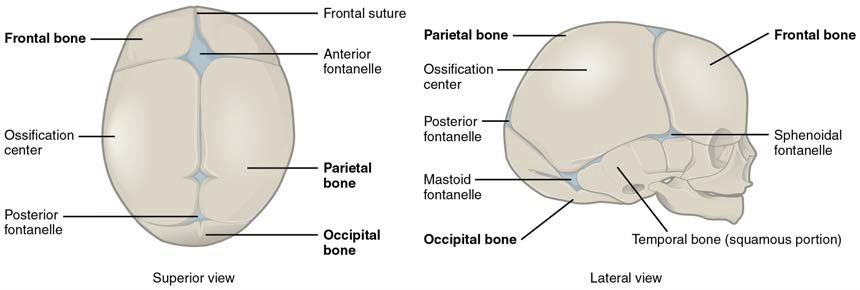
Figure 7.33 Newborn Skull The bones of the newborn skull are not fully ossified and are separated by large areas called fontanelles, which are filled with fibrous connective tissue. The fontanelles allow for continued growth of the skull after birth. At the time of birth, the facial bones are small and underdeveloped.
Cranial Bones of the Skull
The cranial bones contain and protect the brain. The interior space that is almost completely occupied by the brain is called the cranial cavity. This cavity is bounded superiorly by the rounded superior aspect of the skull, which is called the calvaria (skullcap), and the lateral and posterior sides of the skull. The bones that form the superior and lateral sides of the cranial bones are usually referred to as the “flat” bones of the skull. The floor of the cranium is referred to as the base of the skull. This is a complex area that varies in depth and has numerous openings for the passage of cranial nerves, blood vessels and the spinal cord. Inside the skull, the base is subdivided into three large spaces, called the anterior cranial fossa, middle cranial fossa and posterior cranial fossa (fossa = “trench or ditch”) (Figure 7.6). From anterior to posterior, the fossae increase in depth. The shape and depth of each fossa corresponds to the shape and size of the brain region that each houses. The frontal lobes of the cerebrum occupy the anterior cranial fossa, the temporal lobes occupy the middle cranial fossa and the cerebellum occupies the posterior cranial fossa.
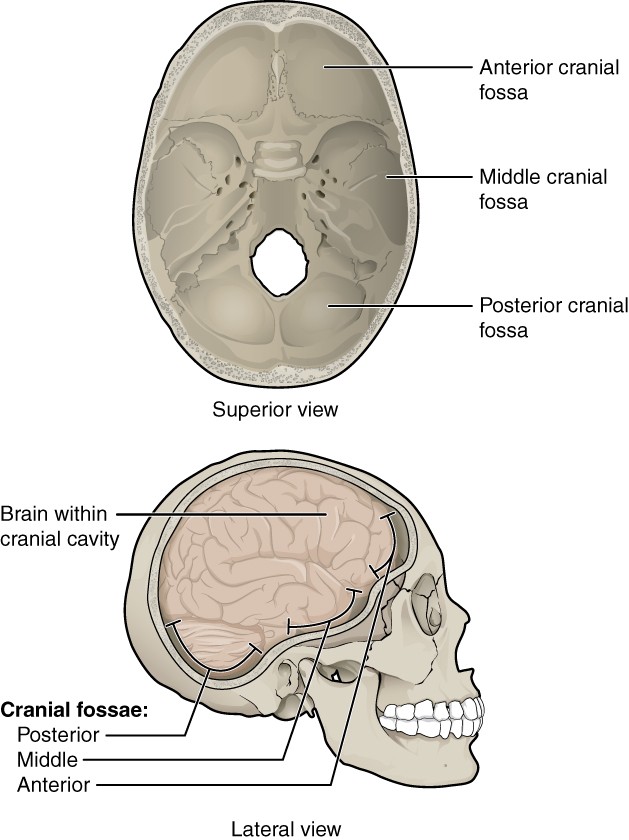
Figure 7.6 Cranial Fossae The cranial bones surround and protect the brain, which occupies the cranial cavity. The base of the cranium, which forms the floor of cranial cavity, is subdivided into the shallow anterior cranial fossa, the middle cranial fossa, and the deep posterior cranial fossa.
The cranial bones consist of eight bones. These include the paired parietal and temporal bones, plus the unpaired frontal, occipital, sphenoid and ethmoid bones.
INTERACTIVE ACTIVITY
Facial Bones of the Skull
The facial bones of the skull form the upper and lower jaws, the nose, nasal cavity and nasal septum, and the orbit. The facial bones include 14 bones, with six paired bones and two unpaired bones. The paired bones are the maxilla, palatine, zygomatic, nasal, lacrimal, and inferior nasal conchae bones. The unpaired bones are the vomer and mandible bones. Although classified as a cranial bone, the ethmoid bone also contributes to the nasal septum and the walls of the nasal cavity and orbit.
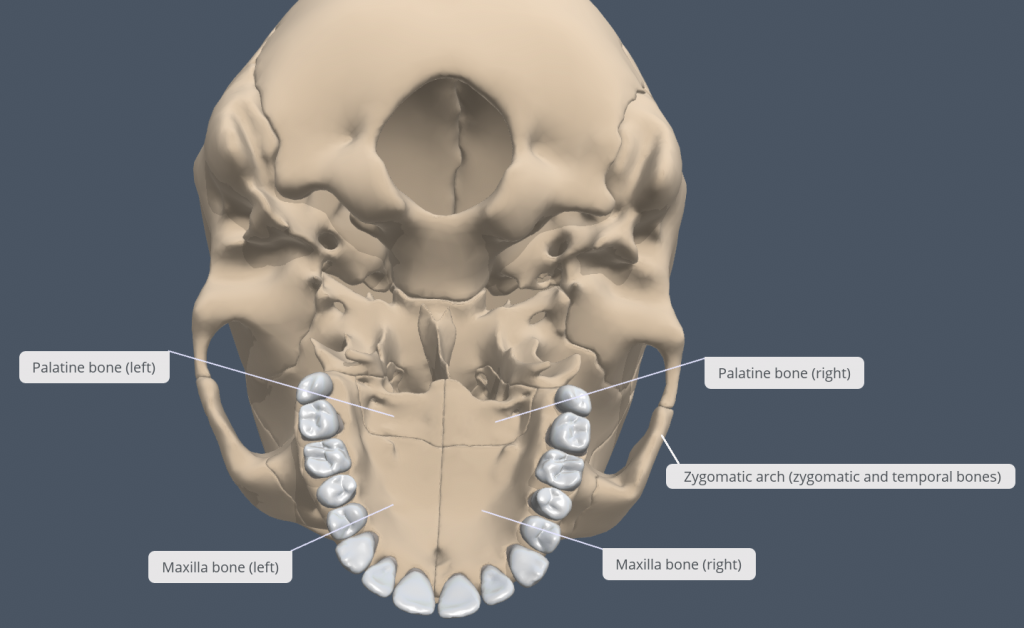
Figure XX: Hard palate of cranium The hard palate is made up from the right and left maxillae anteriorly (3/4) and the right and left palatine bones posteriorly (1/4). The hard palate marks the boundary between the oral and nasal cavities. Also note the zygomatic arch on the cranium that is formed from processes from the zygomatic bone and temporal bone that connect laterally. [Created in Anatomy.TV, Primal Pictures]
The Orbital Cavity
The orbital cavity is the bony socket that houses the eyeball and contains the muscles that move the eyeball or open the upper eyelid (extraocular eye muscles). Each orbital cavity is cone-shaped, with a narrow posterior region that widens toward the large anterior opening. The walls of each orbital cavity include contributions from seven skull bones (Figure 7.16).
At the posterior apex of the orbit is the opening of the optic canal, which allows for passage of the optic nerve from the retina to the brain. Lateral to this is the elongated and irregularly shaped superior orbital fissure, which provides passage for the artery that supplies the eyeball, sensory nerves, and the nerves that supply the muscles involved in eye movements. Also note the inferior orbital fissure located inferolateral to the superior orbital fissure, which allows carries a number of arteries and nerves.
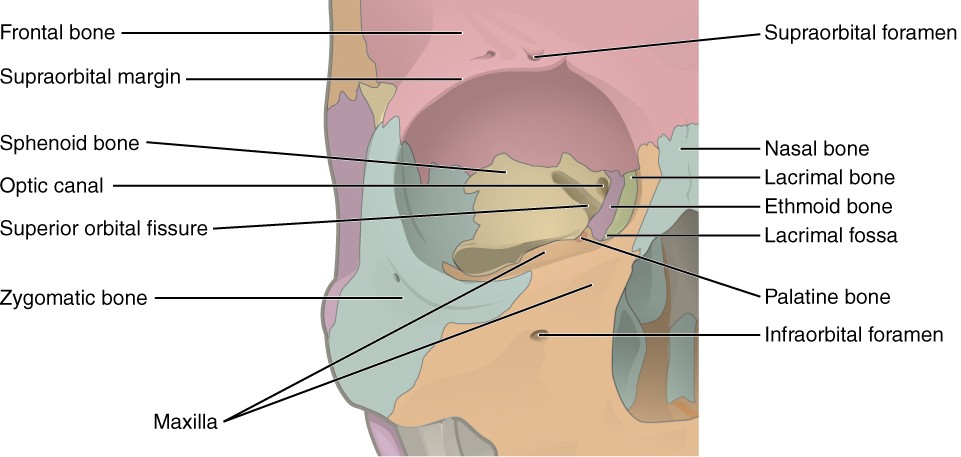
Figure 7.16 Bones of the Orbit Seven skull bones contribute to the walls of the orbit. Opening into the posterior orbit from the cranial cavity are the optic canal and superior orbital fissure.
The Nasal Septum and Nasal Conchae
The nasal septum consists of both bone and cartilage components (Figure 7.17; see also Figure 7.11). The superior part of the septum is formed by the perpendicular plate of the ethmoid bone. The inferior and posterior parts of the septum are formed by the triangular-shaped vomer bone. In an anterior view of the skull, the perpendicular plate of the ethmoid bone is easily seen inside the nasal opening as the superior part of the nasal septum, but only a small portion of the vomer is seen as the inferior septum. A better view of the vomer bone is seen when looking into the posterior nasal cavity with an inferior view of the skull, where the vomer forms the full height of the nasal septum. The anterior nasal septum is formed by the septal cartilage, a flexible plate that fills in the gap between the perpendicular plate of the ethmoid and vomer bones. This hyaline cartilage plate also extends externally into the nose where it separates the right and left nostrils.
Attached to the lateral wall on each side of the nasal cavity are the superior, middle, and inferior nasal conchae (singular = concha), which are named for their positions (see Figure 7.13). These are bony plates that curve inferiorly as they project into the space of the nasal cavity. They serve to swirl the incoming air, which helps to warm and moisturise it before the air moves into the delicate air sacs of the lungs. This also allows mucous, secreted by the tissue lining the nasal cavity, to trap incoming dust, pollen, bacteria and viruses. The largest of the conchae is the inferior nasal concha, which is an independent bone of the skull. The middle conchae and the superior conchae, which are the smallest, are both formed by the ethmoid bone. When looking into the anterior nasal opening of the skull, only the inferior and middle conchae can be seen. The small superior nasal concha is well hidden superior and posterior to the middle concha.
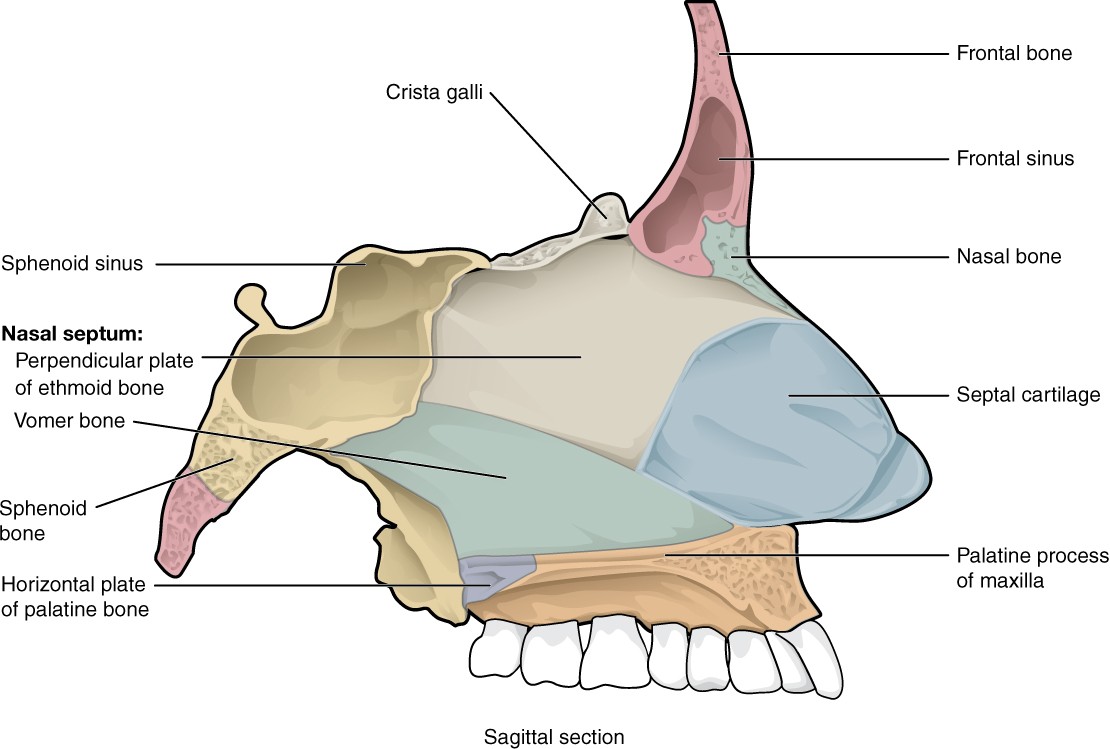
Figure 7.17 Nasal Septum The nasal septum is formed by the perpendicular plate of the ethmoid bone and the vomer bone. The septal cartilage fills the gap between these bones and extends into the nose. Also note the bones that make up the hard palate: maxillae anteriorly and palatine bones posteriorly.
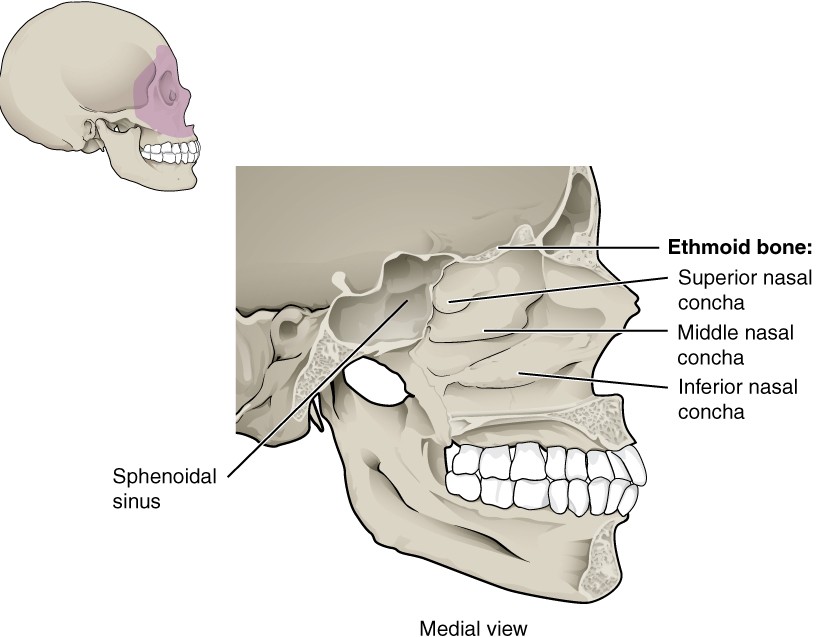
Figure 7.13 Lateral Wall of Nasal Cavity The three nasal conchae are curved bones that project from the lateral walls of the nasal cavity. The superior nasal concha and middle nasal concha are parts of the ethmoid bone. The inferior nasal concha is an independent bone of the skull.
Hyoid Bone
The hyoid bone is an independent bone that does not contact any other bone and thus is not part of the skull (Figure 7.19). It is a small U-shaped bone located in the superior aspect of the neck near the level of the inferior mandible, with the tips of the “U” pointing posteriorly. The hyoid serves as the base for the tongue, and is attached to the larynx inferiorly and the pharynx posteriorly. The hyoid is held in position by a series of small muscles that attach to it superiorly and inferiorly. These muscles act to move the hyoid superiorly/inferiorly or anteriorly/posteriorly. Movements of the hyoid are coordinated with movements of the tongue, larynx and pharynx during swallowing and speaking.
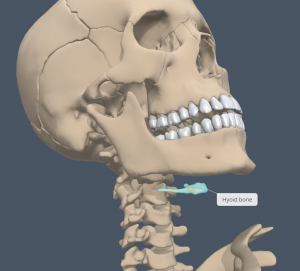
Figure 7.19 Hyoid Bone The hyoid bone is located in the superior aspect of the neck and does not join with any other bone. It provides attachments for muscles that act on the tongue, larynx and pharynx. [Created in Anatomy.TV, Primal Pictures]
Axial: The Vertebral Column
Learning Objectives
By the end of this section, you will be able to:
- Describe each region of the vertebral column and the number of bones in each region
- Discuss the curves of the vertebral column and how these change after birth
- Describe a typical vertebra and determine the distinguishing characteristics for vertebrae in each vertebral region and features of the sacrum and the coccyx
- Define the structure of an intervertebral disc
The vertebral column is known in layterms as the spinal column or spine (Figure 7.20). It consists of a sequence of vertebrae (singular = vertebra), each of which is separated and united by an intervertebral disc. Together, the vertebrae and intervertebral discs form the vertebral column. It is a flexible column that supports the head, neck and body and allows for their movements. It also protects the spinal cord, which passes through openings in the vertebrae.
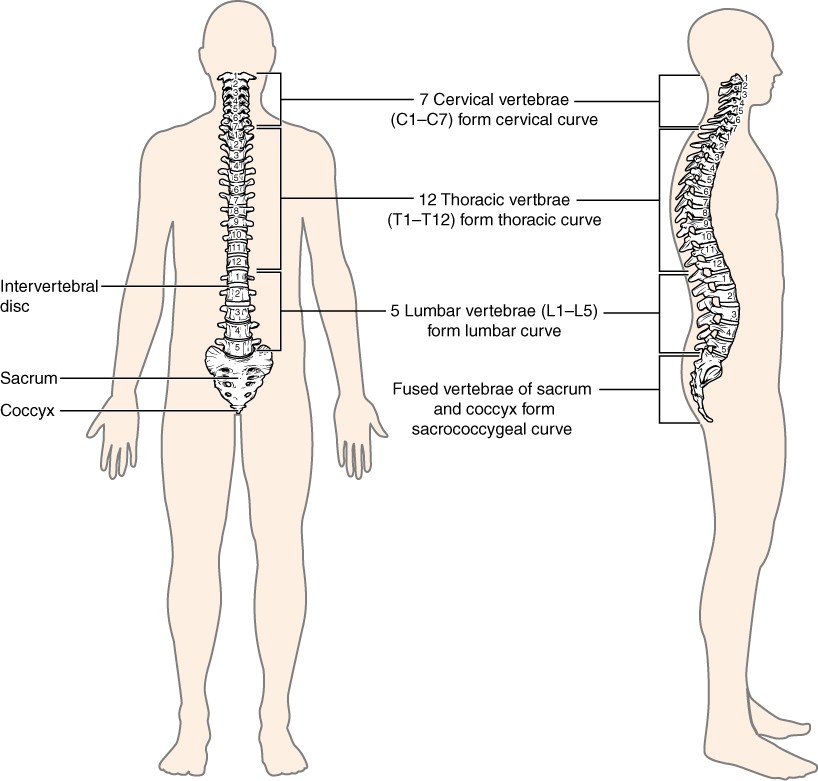
Figure 7.20 Vertebral Column The adult vertebral column consists of 24 vertebrae, plus the sacrum and coccyx. The vertebrae are divided into three regions: cervical C1–C7 vertebrae, thoracic T1–T12 vertebrae, and lumbar L1–L5 vertebrae. The vertebral column is curved, with two primary curvatures (thoracic and sacrococcygeal curves) and two secondary curvatures (cervical and lumbar curves).
Regions of the Vertebral Column
The vertebral column originally develops as a series of 33 vertebrae, but this number is eventually reduced to 24 vertebrae, plus the sacrum and coccyx due to fusion of individual sacral and coccygeal elements as we age. The vertebral column is subdivided into five regions, with the vertebrae in each area named for that region and numbered in descending order. In the neck, there are seven cervical vertebrae, each designated with the letter “C” followed by its number. Superiorly, the C1 vertebra articulates (forms a joint) with the occipital condyles of the skull. Inferiorly, C1 articulates with the C2 vertebra, and so on. Inferior to these are the 12 thoracic vertebrae, designated T1–T12. The inferior back contains the L1–L5 lumbar vertebrae. The single sacrum is formed by the fusion of five sacral vertebrae. Similarly, the coccyx results from the fusion of four small coccygeal vertebrae. However, sacral and coccygeal fusion does not start until 20 years of age and are not completed until middle age.
Curvatures of the Vertebral Column
The adult vertebral column does not form a straight line, but instead has four curvatures along its length (see Figure 7.20). These curves increase the vertebral column’s strength, flexibility, and ability to absorb shock. When the load on the vertebral column is increased, by carrying a heavy backpack for example, the curvatures increase in depth (become more curved) to accommodate the extra weight. They then spring back when the weight is removed. The four adult curvatures are classified as either primary or secondary curvatures. Primary curves are retained from the original foetal curvature, while secondary curvatures develop after birth.
During foetal development, the body is flexed anteriorly into the foetal position, giving the entire vertebral column a single curvature that is concave anteriorly. In the adult, this foetal curvature is retained in two regions of the vertebral column as the thoracic curvature, which involves the thoracic vertebrae, and the sacrococcygeal curvature, formed by the sacrum and coccyx. Each of these is thus called a primary curvature because they are retained from the original foetal curvature of the vertebral column.
A secondary curvature develops gradually after birth as the child learns to move its head, sit upright, stand and walk. Secondary curvatures are concave posteriorly, opposite in direction to the original foetal curvature. The cervical curvature of the neck region develops as the infant begins to hold their head upright when sitting. Later, as the child begins to stand and then to walk, the lumbar curvature of the inferior back develops.
General Structure of a Vertebra
Within the different regions of the vertebral column, vertebrae vary in size and shape, but they all follow a similar structural pattern. A typical vertebra will consist of a body, a vertebral arch and seven processes (Figure 7.23).
The vertebral body is the anterior portion of each vertebra and is the part that supports the body weight. Because of this, the vertebral bodies progressively increase in size and thickness as you move inferiorly in the vertebral column. The bodies of adjacent vertebrae are separated and strongly united by an intervertebral disc.
The vertebral arch forms the posterior portion of each vertebra. It consists of four parts, the right and left pedicles and the right and left laminae. Each pedicle forms one of the lateral sides of the vertebral arch. The pedicles are anchored to the posterior side of the vertebral body. Each lamina forms part of the posterior roof of the vertebral arch. The large opening between the vertebral arch and body is the vertebral foramen, which contains the spinal cord. In the intact vertebral column, the vertebral foramina of all of the vertebrae align to form the vertebral canal, which serves as the bony protection and passageway for the spinal cord. When the vertebrae are aligned together in the vertebral column, notches in the margins of the pedicles of adjacent vertebrae together form an intervertebral foramen, the opening through which a spinal nerve exits from the vertebral column (Figure 7.24).
Seven processes arise from the vertebral arch. Each paired transverse process projects laterally and arises from the junction point between the pedicle and lamina. The single spinous process projects posteriorly at the midline of the back. The spinous processes can easily be palpated as a series of bumps just deep to the skin along the midsagittal plane of the back. The transverse and spinous processes serve as important muscle attachment sites. A superior articular process extends superiorly, and an inferior articular process projects inferiorly on each side of a vertebra. The paired superior articular processes of one vertebra join with the corresponding paired inferior articular processes from the next more superior vertebra. These junctions form slightly moveable joints between the adjacent vertebrae. The shape and orientation of the articular processes vary in different regions of the vertebral column and play a major role in determining the type and range of motion available in each region.
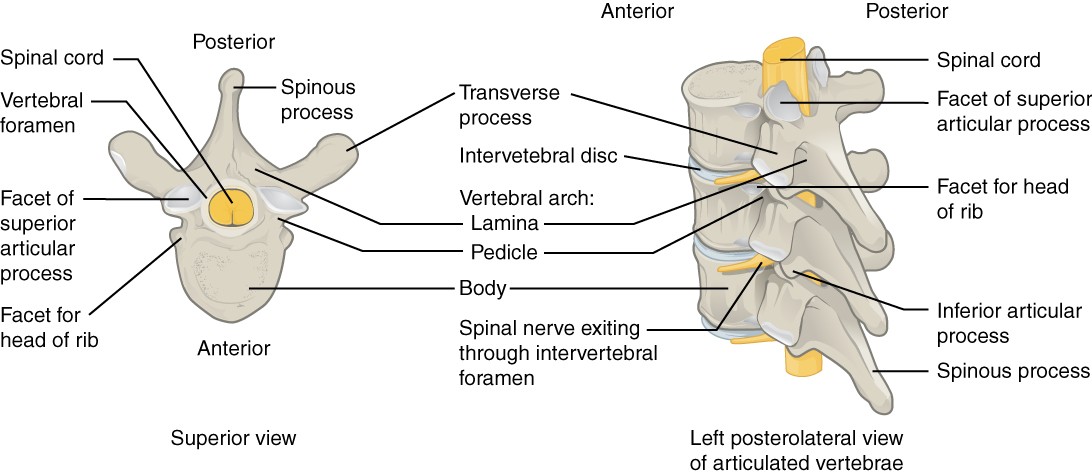
Figure 7.23 Parts of a Typical Vertebra A typical vertebra consists of a body and a vertebral arch. The arch is formed by the paired pedicles and paired laminae. Arising from the vertebral arch are the transverse, spinous, superior articular, and inferior articular processes. The vertebral foramen provides passage for the spinal cord. Each spinal nerve exits through an intervertebral foramen, located between adjacent vertebrae. Intervertebral discs unite the bodies of adjacent vertebrae.
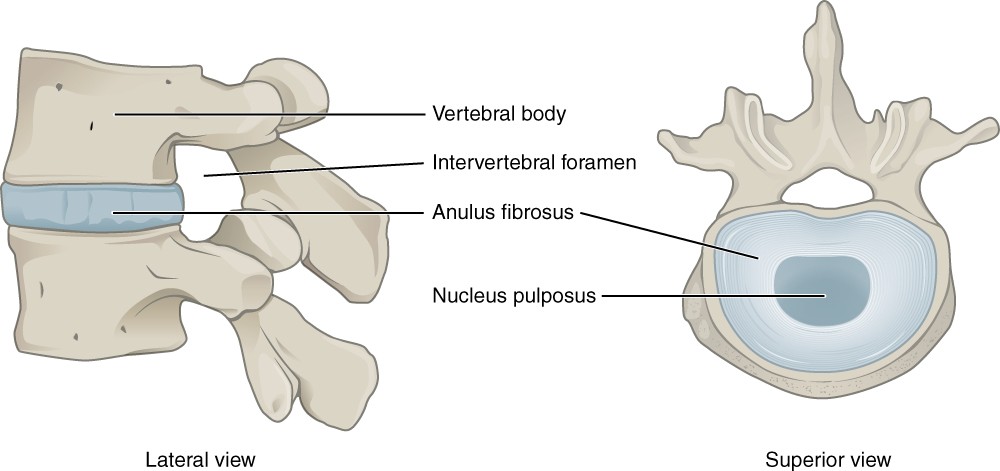
Figure 7.24 Intervertebral Disc The bodies of adjacent vertebrae are separated and united by an intervertebral disc, which provides padding and allows for movements between adjacent vertebrae. The disc consists of a fibrous outer layer called the annulus fibrosus and a gel-like centre called the nucleus pulposus. The intervertebral foramen is the opening formed between adjacent vertebrae for the exit of a spinal nerve.
Regional Modifications of Vertebrae
In addition to the general characteristics of a typical vertebra described above, vertebrae also display characteristic size and structural features that vary between the different vertebral column regions. Thus, cervical vertebrae are smaller than lumbar vertebrae due to differences in the proportion of body weight that each supports. Thoracic vertebrae have sites for rib attachment, and the vertebrae that give rise to the sacrum and coccyx have fused together into single bones.
Cervical Vertebrae
Typical cervical vertebrae, such as C4 or C5, have several characteristic features that differentiate them from thoracic or lumbar vertebrae (Figure 7.25). Cervical vertebrae have a small body, reflecting the fact that they carry the least amount of body weight. Cervical vertebrae usually have a bifid (Y-shaped) spinous process. The spinous processes of the C3–C6 vertebrae are short, but the spinous process of C7 is much longer. You can find these vertebrae by running your finger down the midline of the posterior neck until you encounter the prominent C7 spinous process located at the base of the neck. The transverse processes of the cervical vertebrae are sharply curved (U-shaped) to allow for passage of the cervical spinal nerves. Each transverse process also has an opening called the transverse foramen. An important artery (the vertebral artery) that supplies blood to the brain ascends up the neck by passing through these openings. The superior and inferior articular processes of the cervical vertebrae are flattened and largely oriented transversely.
The first and second cervical vertebrae are further modified, giving each a distinctive appearance. The first cervical (C1) vertebra is also called the atlas, because this is the vertebra that supports the skull on the superior aspect of the vertebral column (in Greek mythology, Atlas was the god who supported the heavens on his shoulders). The C1 vertebra does not have a body or spinous process. Instead, it is ring-shaped, consisting of an anterior arch and a posterior arch. The transverse processes of the atlas are longer and extend more laterally than do the transverse processes of any other cervical vertebrae. The superior articular processes face superiorly and are deeply concave for articulation with the occipital condyles on the base of the skull.
The second cervical (C2) vertebra is called the axis, because it serves as the axis for rotation when turning the head toward the right or left. The axis resembles typical cervical vertebrae in most respects, but is easily distinguished by the dens (odontoid process), a bony projection that extends superiorly from the vertebral body. The dens articulates with the internal/posterior aspect of the anterior arch of the atlas, to form the median atlantoaxial joint. The dens is considered to be formed from what would have been the body of the atlas.
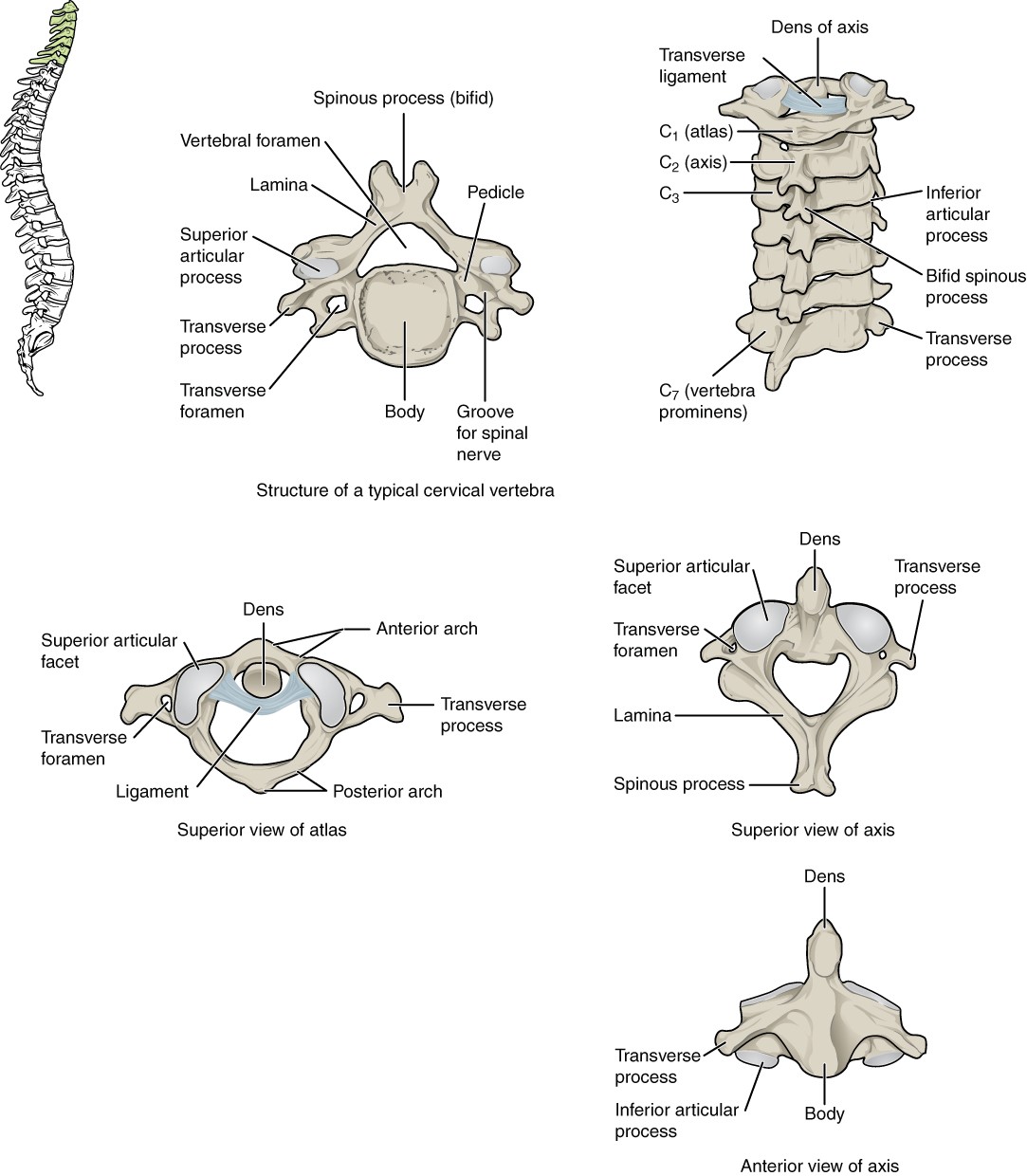
Figure 7.25 Cervical Vertebrae A typical cervical vertebra has a small body, a bifid spinous process, transverse processes that have a transverse foramen and are curved for spinal nerve passage. The atlas (C1 vertebra) does not have a body or spinous process. It consists of an anterior and a posterior arch and elongated transverse processes. The axis (C2 vertebra) has the superiorly projecting dens, which articulates with the anterior arch of the atlas.
Thoracic Vertebrae
The bodies of the thoracic vertebrae are larger than those of cervical vertebrae (Figure 7.26). The characteristic feature for a typical midthoracic vertebra is the spinous process, which is long and has a pronounced inferiorly sloped angle that causes it to overlap with the next inferior vertebra. The superior articular processes of thoracic vertebrae face anteriorly and the inferior processes face posteriorly in the coronal plane. These orientations are important determinants for the type and range of movements available to the thoracic region of the vertebral column.
Thoracic vertebrae have several additional articulation sites, each of which is called a facet, where a rib is attached. Most thoracic vertebrae have two facets located on the lateral sides of the body, each of which is called a costal facet (costal = “rib”). These are for articulation with the head (end) of a rib. An additional facet is located on the transverse process for articulation with the tubercle of a rib.
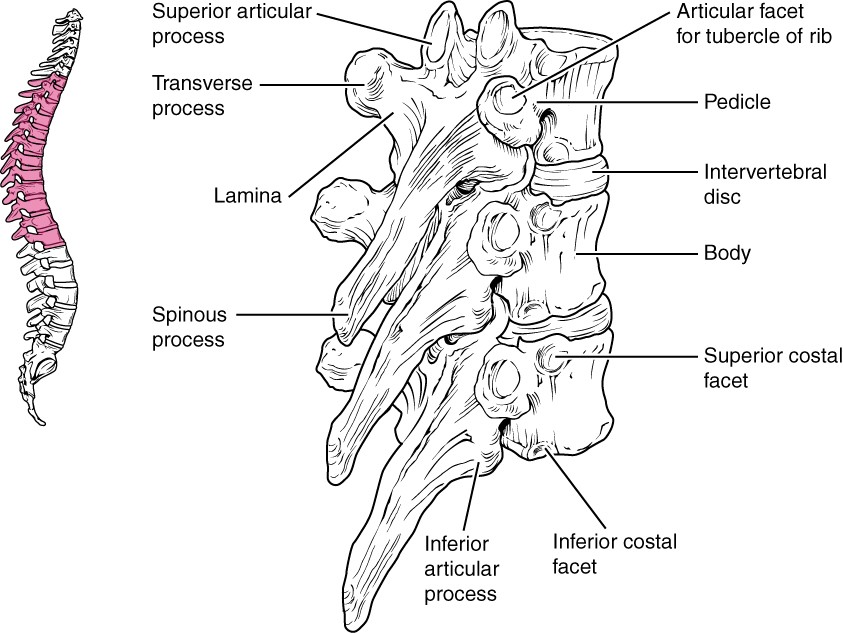
Figure 7.26 Thoracic Vertebrae A typical thoracic vertebra is distinguished by the spinous process, which is long and projects inferiorly to overlap with the next inferior vertebra. It also has articulation sites (facets) on the vertebral body and transverse processes for rib articulation.
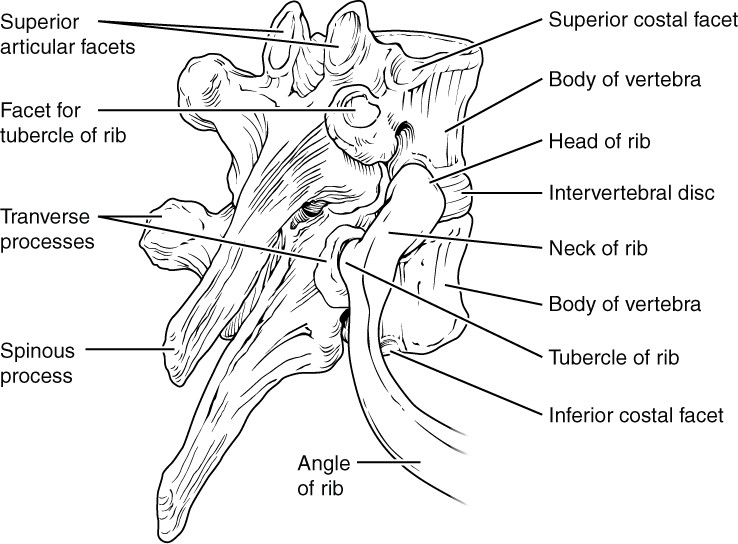
Figure 7.27 Rib Articulation in Thoracic Vertebrae Thoracic vertebrae have superior and inferior articular facets on the vertebral body for articulation with the head of a rib, and a transverse process facet for articulation with the rib tubercle.
Lumbar Vertebrae
Lumbar vertebrae carry the greatest amount of body weight and are thus characterised by the large size and thickness of the vertebral body (Figure 7.28). They have short transverse processes and a short, rectangular spinous process that projects posteriorly. The articular processes are large, with the superior process facing medially and the inferior facing laterally.
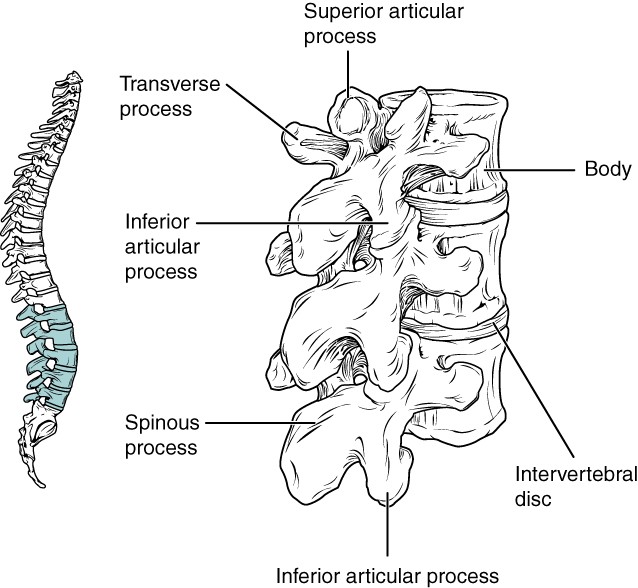
Figure 7.28 Lumbar Vertebrae Lumbar vertebrae are characterised by having a large, thick body and a short, rectangular-shaped spinous process.
Sacrum and Coccyx
The sacrum is a triangular-shaped bone that is thick and wide across its superior base where it is weight bearing and then tapers down to an inferior, non-weightbearing apex (Figure 7.29). It is formed by the fusion of five sacral vertebrae, a process that does not begin until after the age of 20 years. On the anterior surface of the older adult sacrum, the lines of vertebral fusion can be seen as four transverse ridges. On the posterior surface, running inferiorly in the midsagittal plane, is the median sacral crest, a bumpy ridge that is the remnant of the fused spinous processes (median = “midline”; while medial = “toward, but not necessarily at, the midline”).
Laterally the sacrum has the auricular surface, which joins with the ilium portion of the os coxa to form the immobile sacroiliac joints of the pelvis. The anterior and posterior surfaces of the sacrum have a series of paired openings called sacral foramina (singular = foramen) that connect to the sacral canal (equivalent to vertebral canal of cervical, thoracic and lumbar vertebrae). Each of these openings is called a posterior (dorsal) sacral foramen or anterior (ventral) sacral foramen. These openings allow for the anterior and posterior branches of the sacral spinal nerves to exit the sacrum.
The coccyx is derived from the fusion of four very small coccygeal vertebrae (see Figure 7.29). It articulates with the inferior tip of the sacrum. It is not weightbearing in the standing position, but may receive some body weight when sitting.
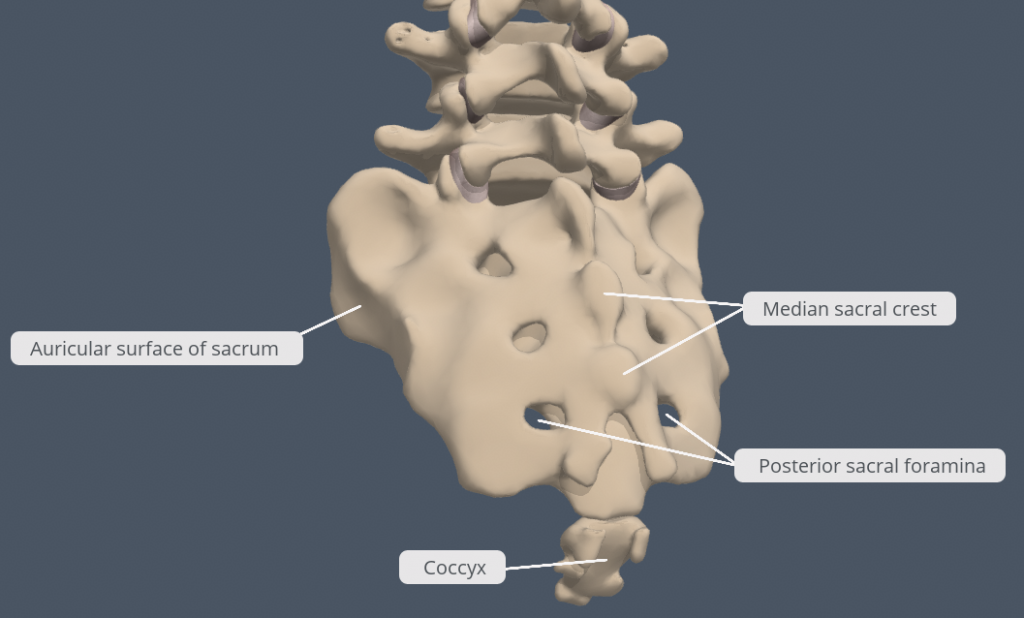
Figure 7.29 Sacrum and Coccyx (Posterolateral view) The sacrum is formed from the fusion of five sacral vertebrae. The fused spinous processes form the median sacral crest. Spinal nerves travel out of the sacral canal via the posterior and anterior sacral foramina (only posterior foramina visible in this figure). The auricular surface of the sacrum articulates with the os coxa to form the sacroiliac joint, connecting the axial skeleton to the appendicular skeleton. The coccyx is formed by the fusion of four small coccygeal vertebrae. [Created in Anatomy.TV, Primal Pictures]
Intervertebral Discs
The bodies of adjacent vertebrae are strongly anchored to each other by an intervertebral disc. This structure provides padding between the bones during weightbearing, and because it can change shape, also allows for movement between the vertebrae. Although the total amount of movement available between any two adjacent vertebrae is small, when these movements are summed together along the entire length of the vertebral column, large body movements can be produced.
Intervertebral Disc
An intervertebral disc is a fibrocartilaginous pad that fills the gap between adjacent vertebral bodies (see Figure 7.24). The intervertebral disc is an example of a symphysis joint. Each disc is anchored to the bodies of its adjacent vertebrae, thus strongly uniting these. The discs also provide padding between vertebrae during weight bearing. Because of this, intervertebral discs are thin in the cervical region and thickest in the lumbar region, which carries the most body weight. In total, the intervertebral discs account for approximately 25 percent of your body height between the top of the pelvis and the base of the skull. Intervertebral discs are also flexible and can change shape to allow for movements of the vertebral column.
Each intervertebral disc consists of two parts. The annulus fibrosus is the tough, fibrous external layer of the disc. It forms a circle (annulus = “ring” or “circle”) and is firmly anchored to the outer margins of the adjacent vertebral bodies. Inside is the nucleus pulposus, consisting of a softer, more gel-like material. It has a high water content that serves to resist compression and thus is important for weightbearing. With increasing age, the water content of the nucleus pulposus gradually declines. This causes the disc to become thinner, decreasing total body height somewhat, and reduces the flexibility and range of motion of the disc, making bending more difficult.
Axial: The Thoracic Cage
Learning Objectives
By the end of this section, you will be able to:
- Discuss the components that make up the thoracic cage
- Identify the parts of the sternum and define the sternal angle
- Discuss the parts of a rib and rib classifications
The thoracic cage forms the thorax (chest) portion of the body. It consists of the 12 pairs of ribs with their costal cartilages and the sternum (Figure 7.32). The ribs are anchored posteriorly to the 12 thoracic vertebrae (T1–T12). The thoracic cage protects the heart and lungs.
Sternum
The sternum is the elongated bony structure that anchors the anterior thoracic cage. It consists of three parts: the manubrium, body, and xiphoid process. The manubrium is the wider, superior portion of the sternum. The superior edge of the manubrium has a shallow, U-shaped border called the jugular (suprasternal) notch. This can be easily palpated at the anterior base of the neck, between the medial ends of the clavicles. The clavicular notch is the shallow depression located on either side at the superior-lateral margins of the manubrium. This is the site of the sternoclavicular joint, between the sternum and clavicle. The first ribs also attach to the manubrium.
The elongated, central portion of the sternum is the body. The manubrium and body join together at the sternal angle, so called because the junction between these two components is not flat, but forms a slight bend. The sternal angle commonly lies at the level of the intervertebral disc betweeen T4 and T5. The second rib attaches to the sternum at the sternal angle. Since the first rib is hidden posterior to the clavicle, the second rib is the most superior rib that can be identified by palpation. Thus, the sternal angle and second rib are important landmarks for the identification and counting of the more inferior ribs. Ribs 3–7 attach to the sternal body.
The inferior tip of the sternum is the xiphoid process. This small structure is cartilaginous early in life, but gradually becomes ossified starting during middle age.
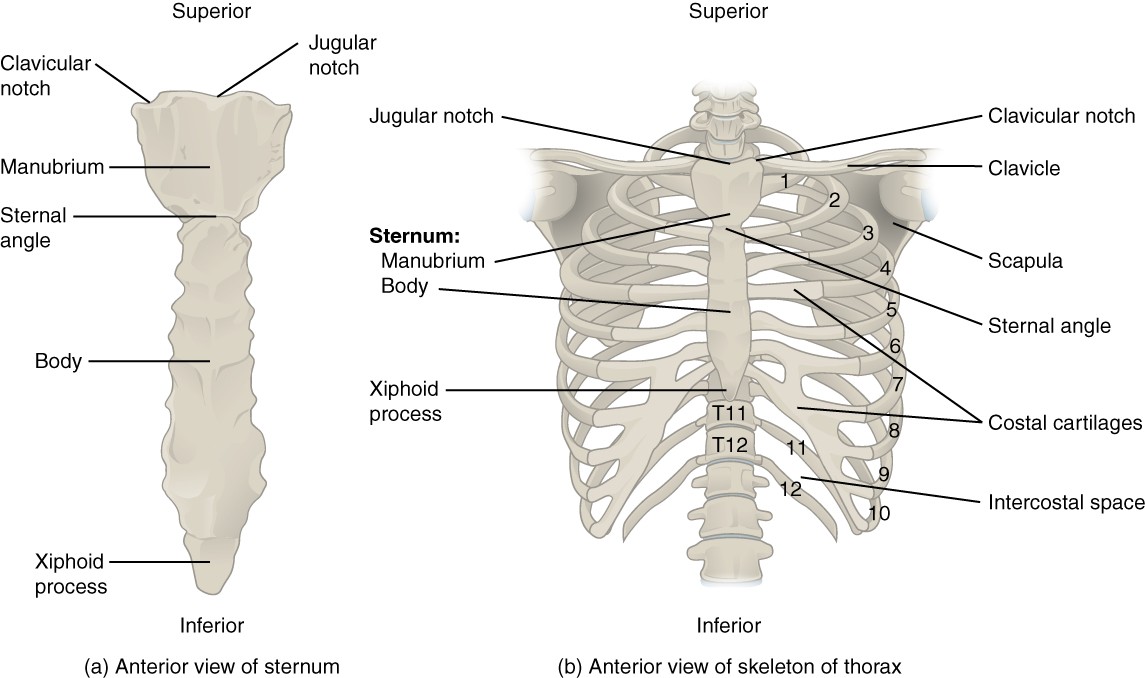
Figure 7.32 Thoracic Cage The thoracic cage is formed by the (a) sternum and (b) 12 pairs of ribs with their costal cartilages. The ribs are anchored posteriorly to the 12 thoracic vertebrae. The sternum consists of the manubrium, body and xiphoid process. The ribs are classified as true ribs (1–7) and false ribs (8–12). The last two pairs of false ribs are also known as floating ribs (11–12).
Ribs
Each rib is a curved, flattened bone that contributes to the wall of the thorax. The ribs articulate posteriorly with the T1–T12 thoracic vertebrae, and most attach anteriorly via their costal cartilages to the sternum. There are 12 pairs of ribs. The ribs are numbered 1–12 in accordance with the thoracic vertebrae.
Parts of a Typical Rib
The posterior end of a typical rib is called the head of the rib (see Figure 7.27). This region articulates primarily with the costal facet located on the body of the same numbered thoracic vertebra and to a lesser degree, with the costal facet located on the body of the next superior vertebra. A small bump on the posterior rib surface is the tubercle of the rib, which articulates with the facet located on the transverse process of the same numbered vertebra. The remainder of the rib is the shaft of the rib (body). A shallow costal groove for the passage of blood vessels and a nerve is found along the inferior margin of each rib.
Rib Classifications
The bony ribs do not extend anteriorly completely around to the sternum. Instead, each rib ends in a costal cartilage. These cartilages are made of hyaline cartilage and can extend to more than 7cm. Most ribs are then attached, either directly or indirectly, to the sternum via their costal cartilage (see Figure 7.32). The ribs are classified into three groups based on their relationship to the sternum.
Ribs 1–7 are classified as true ribs. The costal cartilage from each of these ribs attaches directly to the sternum. Ribs 8–12 are called false ribs. The costal cartilages from these ribs do not attach directly to the sternum. For ribs 8–10, the costal cartilages are attached to the cartilage of the more superior rib. Thus, the cartilage of rib 10 attaches to the cartilage of rib 9, rib 9 then attaches to rib 8, and rib 8 is attached to rib 7. The last two false ribs (11–12) are also called floating ribs. These are short ribs that do not attach to the sternum at all. Instead, their small costal cartilages terminate within the musculature of the lateral abdominal wall.
Appendicular: The Pectoral Girdle
Learning Objectives
By the end of this section, you will be able to:
- Describe the bones that form the pectoral girdle
- Identify and describe the major features of the clavicle and scapula
The pectoral girdle consists of two bones, the scapula and clavicle (Figure 8.3). The right and left pectoral girdles are not joined to each other, allowing each to operate independently.
The clavicle (collarbone) is an S-shaped bone located on the anterior side of the shoulder. The clavicle has three regions: the medial end, the lateral end, and the shaft. The medial end, known as the sternal end of the clavicle, has a triangular shape and articulates with the manubrium portion of the sternum. This forms the sternoclavicular joint, which is the only bony articulation between the pectoral girdle of the upper limb and the axial skeleton. The lateral or acromial end of the clavicle articulates with the acromion of the scapula at the acromioclavicular joint, the portion of the scapula that forms the bony tip of the shoulder.
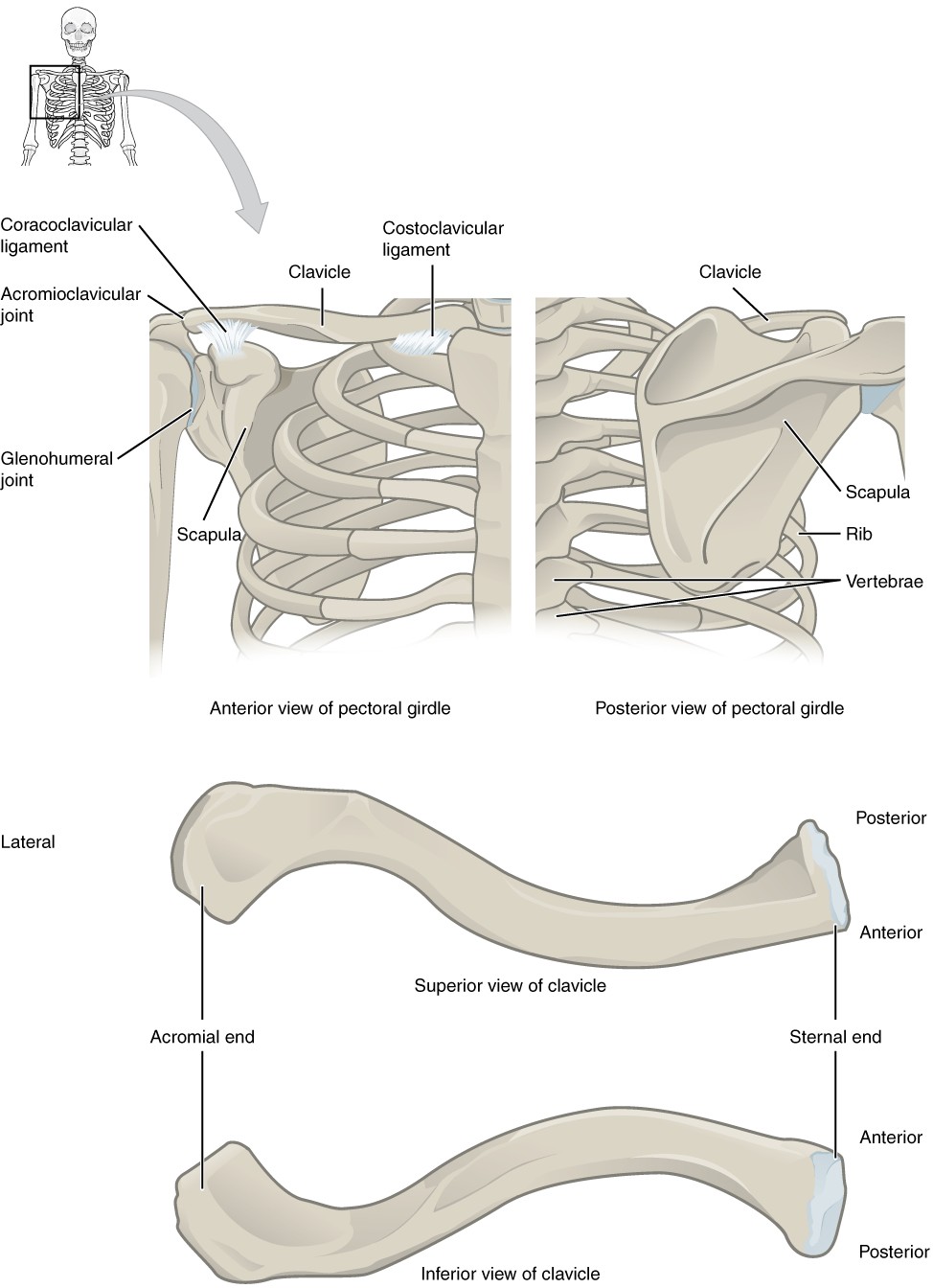
Figure 8.3 Pectoral Girdle The pectoral girdle consists of the clavicle and the scapula, which serve to attach the upper limb to the sternum of the axial skeleton.
The scapula (shoulder blade) lies on the posterior aspect of the shoulder. The scapula has several important landmarks (Figure 8.4). The inferior point of the triangular scapula is the inferior angle of the scapula. Laterally the scapula has a shallow concavity called the glenoid fossa (glenoid cavity), which articulates with the humerus of the brachium to form the glenohumeral joint (shoulder joint). The scapula also has two prominent projections. Superior to the glenoid fossa is the hook-like coracoid process (coracoid = “shaped like a crow’s beak”). This process projects anteriorly and curves laterally. On the posterior aspect, the spine of the scapula is a long and prominent ridge that runs across its superior portion. Extending laterally from the spine is a flattened and expanded region called the acromion or acromial process. The acromion forms the bony tip of the superior shoulder region and articulates with the lateral end of the clavicle, forming the acromioclavicular joint (see Figure 8.3). Together, the clavicle, acromion, and spine of the scapula form a V-shaped bony line that provides for the attachment of neck and back muscles that act on the shoulder, as well as muscles that pass across the glenohumeral joint to act on the brachium.
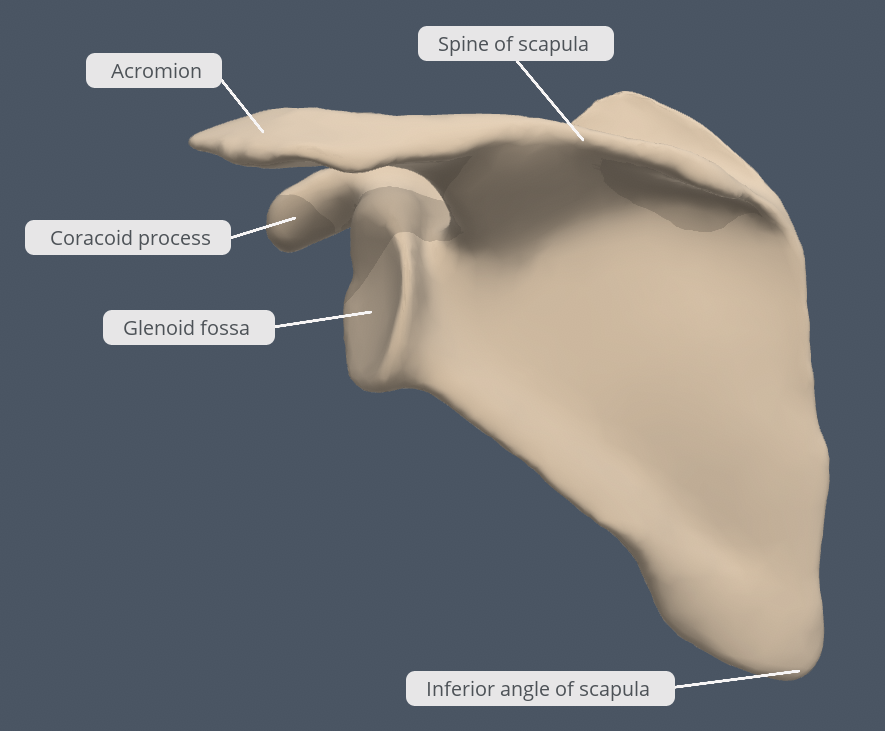
Figure 8.4 Scapula (Posterolateral view) Note the major features of the scapula including the glenoid fossa that articulates with the head of the humerus at the glenohumeral joint and the acromion that articulates with the clavicle to form the acromioclavicular joint. The spine of the scapula, acromion and inferior angle of the scapula are all important palpable landmarks of the scapula. [Created in Anatomy.TV, Primal Pictures]
Appendicular: Bones of the Upper Limb
Learning Objectives
By the end of this section, you will be able to:
- Identify and describe the major features of the humerus, ulna, radius, carpals, metacarpals and phalanges of the hand
- List the bones and bony landmarks that articulate at each joint of the upper limb
The upper limb is divided into three regions. These consist of the brachium (arm), located between the glenohumeral and elbow joints; the antebrachium (forearm), which is between the elbow and radiocarpal (wrist) joints; and the hand, which is located distal to the wrist. There are 30 bones in each upper limb (see Figure 8.2). The humerus is the single bone of the brachium, and the ulna (medially) and the radius (laterally) are the paired bones of the antebrachium. The base of the hand contains eight bones, each called a carpal bone, and the palm of the hand is formed by five bones, each called a metacarpal bone. The fingers and thumb contain a total of 14 bones, each of which is a phalanx (phalange, plural) of the hand.
Humerus
The humerus is the single bone of the brachial region (Figure 8.5). At its proximal end is the head of the humerus. This is the large, round, smooth region that faces medially. The head articulates with the glenoid fossa of the scapula to form the glenohumeral (shoulder) joint. Located on the lateral side of the proximal humerus is an expanded bony area called the greater tubercle. The smaller lesser tubercle of the humerus is found on the anterior aspect of the humerus. Both the greater and lesser tubercles serve as attachment sites for the rotator cuff muscles that act across the glenohumeral joint. Passing between the greater and lesser tubercles is the narrow intertubercular sulcus, which is also known as the bicipital groove because it provides passage for the tendon of the long head of the biceps brachii muscle. The deltoid tuberosity is a roughened, V-shaped region located on the lateral side in the middle of the humerus shaft. As its name indicates, it is the site of attachment for the deltoid muscle.
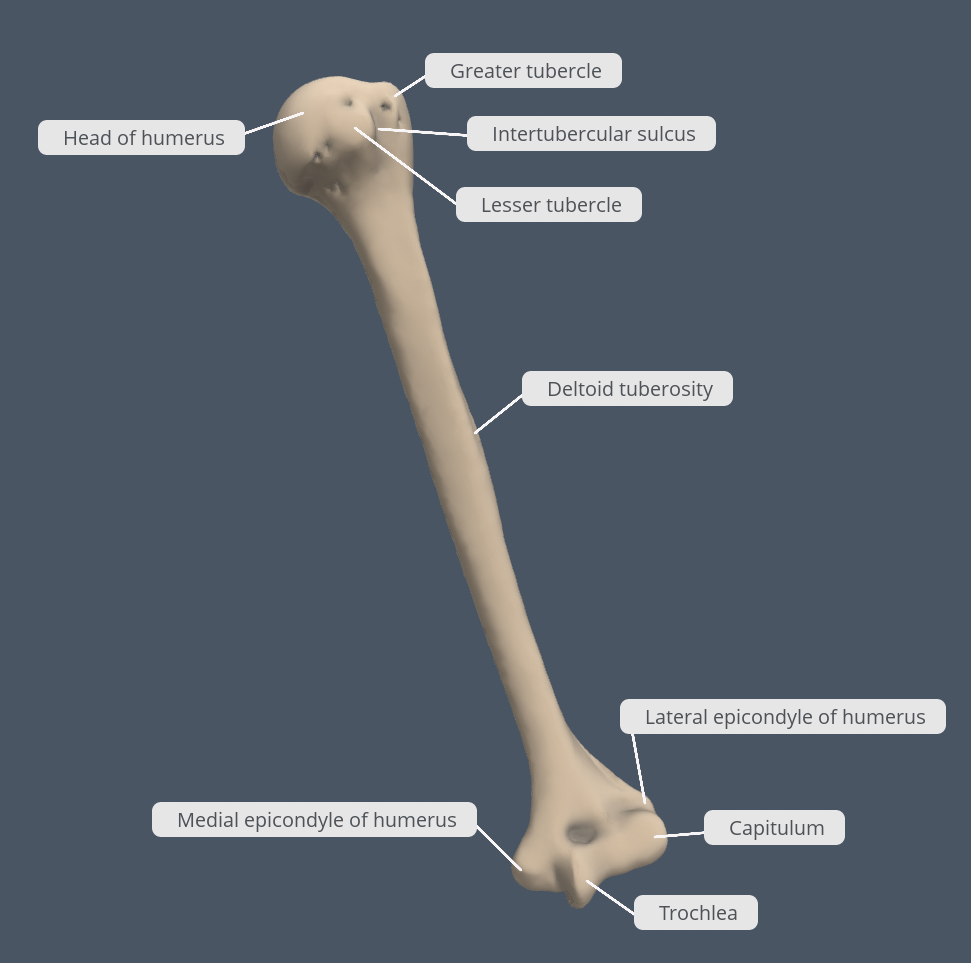
Figure 8.5 Humerus (Anterior view) The humerus is the single bone of the brachial region. It articulates with the radius and ulna to form the elbow joint, and the scapula to form the glenohumeral joint. [Created in Anatomy.TV, Primal Pictures]
Distally, the humerus becomes flattened. The prominent bony projection on the medial side is the medial epicondyle of the humerus. This large bony projection often gets bumped, resulting in compression to the ulnar nerve that courses posterior to the medial epicondyle; when we experience pain through a dingling sensation in our antebrachium and hand we say we have hit our ‘funny bone’ – but of course at the time it is anything but funny! The much smaller lateral epicondyle of the humerus is found on the lateral side of the distal humerus. All of these areas are attachment points for muscles that act on the antebrachium, carpus (wrist) and hand. The powerful grasping muscles of the anterior antebrachium arise from the medial epicondyle, which is thus larger and more robust than the lateral epicondyle that gives rise to the weaker posterior antebrachial muscles.
The distal end of the humerus has two articulation areas, which join the ulna and radius to form the elbow joint. The more medial of these areas is the trochlea, a pulley-shaped region (trochlea = “pulley”), which articulates with the ulna (ulnohumeral part of elbow joint). Immediately lateral to the trochlea is the capitulum (“small head”), a knob-like structure located on the anterior surface of the distal humerus. The capitulum articulates with the radius (radiohumeral part of elbow joint). The posterior humerus has the olecranon fossa, a large non-articular depression that receives the olecranon process of the ulna when the elbow joint is fully extended.
Ulna
The ulna is the medial bone of the antebrachium. It runs parallel to the radius, which is the lateral bone of the antebrachium (Figure 8.6). The proximal end of the ulna resembles a crescent wrench with its large, C-shaped trochlear notch. This region articulates with the trochlea of the humerus as part of the elbow joint. To the lateral side and slightly inferior to the trochlear notch is a small, smooth area called the radial notch of the ulna. This area is the site of articulation between the proximal radius and the ulna, forming the proximal radioulnar joint. The posterior and superior portions of the proximal ulna make up the olecranon, which forms the posterior bony tip of the elbow.
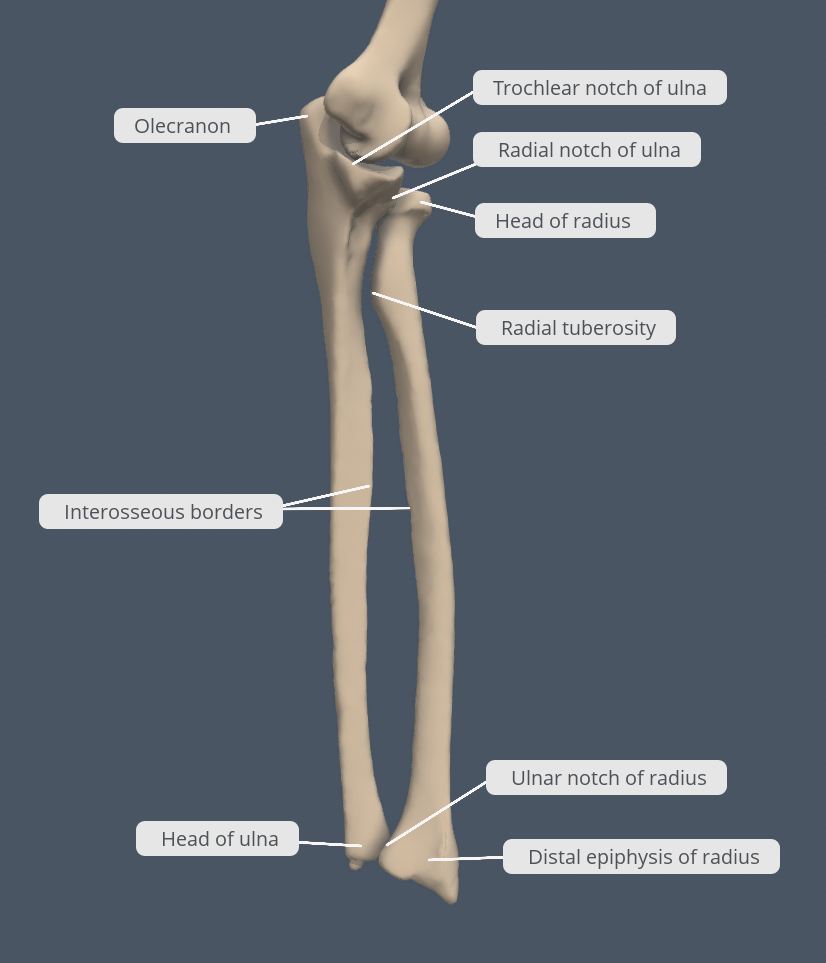
Figure 8.6 Ulna and Radius (Anterior view) The ulna is located on the medial side of the antebrachium and the radius is on the lateral side. These bones are attached to each other by an interosseous membrane at their interosseous borders. Note the articulations between the radius, ulna and humerus to form the elbow joint. [Created in Anatomy.TV, Primal Pictures]
More distal is the shaft of the ulna. The lateral side of the shaft forms a ridge called the interosseous border of the ulna. This is the line of attachment for the interosseous membrane of the antebrachium, a sheet of dense connective tissue that unites the ulna and radius. The small, rounded area that forms the distal end is the head of the ulna.
Radius
The radius runs parallel to the ulna, on the lateral (thumb) side of the antebrachium (see Figure 8.6). The head of the radius is a disc-shaped structure that forms the proximal end. The small depression on the surface of the head articulates with the capitulum of the humerus as part of the elbow joint, whereas the smooth, outer margin of the head articulates with the radial notch of the ulna at the proximal radioulnar joint. Inferior to this point on the medial side is the radial tuberosity, an oval-shaped, bony protuberance that serves as a muscle attachment point for the tendon of the biceps brachii. The shaft of the radius is slightly curved and has a small ridge along its medial side. This ridge forms the interosseous border of the radius, which, like the similar border of the ulna, is the line of attachment for the interosseous membrane that unites the two antebrachial bones. The distal end of the radius has a smooth surface for articulation with two carpal bones to form the radiocarpal joint or wrist joint (Figure 8.7 and Figure 8.8). On the medial side of the distal radius is the ulnar notch of the radius. This shallow depression articulates with the head of the ulna, which together form the distal radioulnar joint.
Carpal Bones
The carpus is formed by a series of eight small carpal bones (see Figure 8.7). The carpal bones are arranged in two rows, forming a proximal row of four carpal bones and a distal row of four carpal bones. The bones in the proximal row, running from the lateral (thumb) side to the medial side, are the scaphoid (“boat-shaped”), lunate (“moon- shaped”), triquetrum or triquetral bone (“three-cornered”), and pisiform (“pea-shaped”) bones. The small, rounded pisiform bone articulates with the anterior surface of the triquetrum. The pisiform thus projects anteriorly, where it forms the bony bump that can be felt at the medial base of your hand. The distal bones (lateral to medial) are the trapezium (“table”), trapezoid (“resembles a table”), capitate (“head-shaped”), and hamate (“hooked bone”) bones. The hamate bone is characterised by a prominent bony extension on its anterior side called the hook of the hamate.
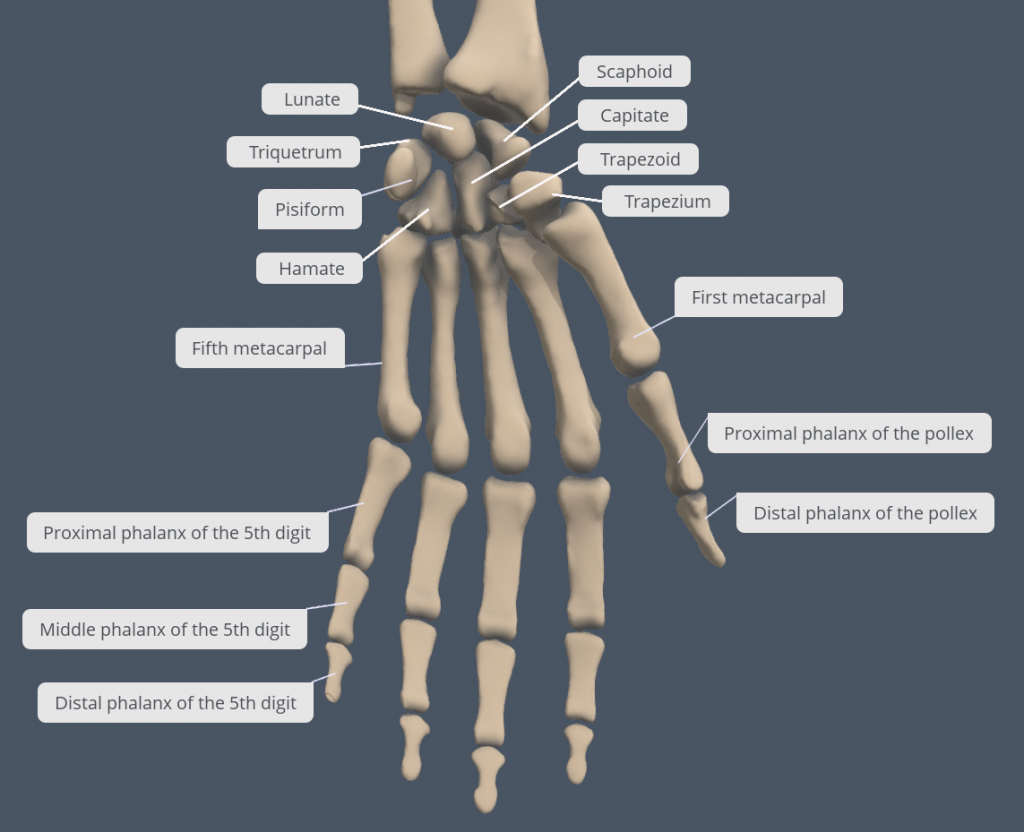
Figure 8.7 Bones of the Wrist and Hand The eight carpal bones form the base of the hand. These are arranged into proximal and distal rows of four bones each. The metacarpal bones form the palm of the hand. The pollex (thumb) and fingers consist of the phalangeal bones. [Created in Anatomy.TV, Primal Pictures]
The carpal bones form the base of the hand. This can be seen in the radiograph (X-ray image) of the hand that shows the relationships of the hand bones to the skin creases of the hand (see Figure 8.8). Within the carpal bones, the four proximal bones are united to each other by ligaments to form a unit. Only three of these bones, the scaphoid, lunate, and triquetrum, contribute to the radiocarpal joint. The scaphoid and lunate bones articulate directly with the distal end of the radius, whereas the triquetrum bone articulates with a fibrocartilaginous pad that lies distal to the ulna. The distal end of the ulna thus does not directly articulate with any of the carpal bones.
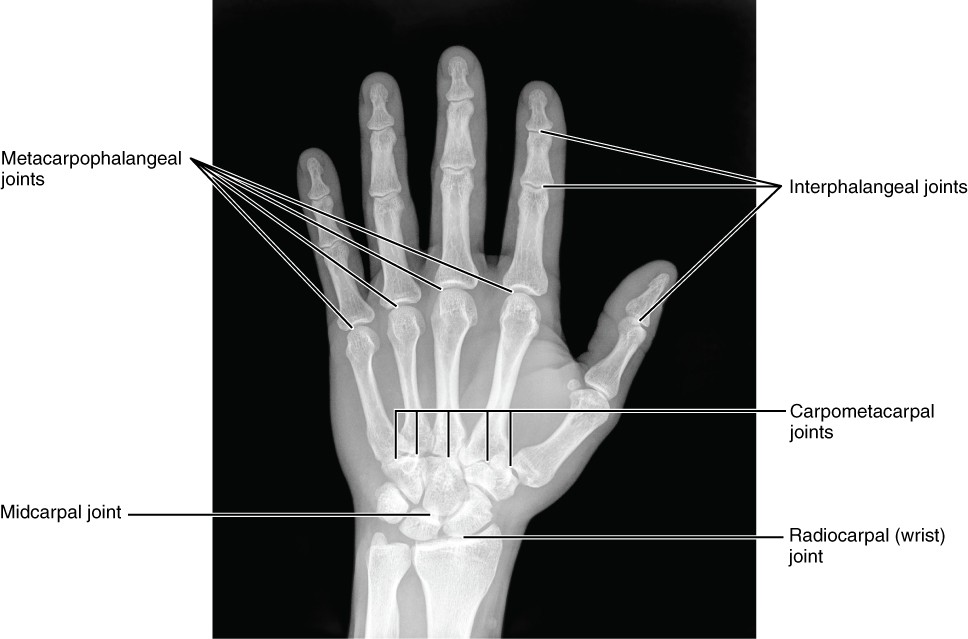
Figure 8.8 Bones of the Hand This radiograph shows the position of the bones within the hand. Note the carpal bones that form the base of the hand. [modification of work by Trace Meek]
Metacarpal Bones
The palm of the hand contains five elongated metacarpal bones. These bones lie between the carpal bones of the wrist and the bones of the fingers and pollex (see Figure 8.7). The proximal end of each metacarpal bone articulates with one of the distal carpal bones. Each of these articulations is a carpometacarpal joint (see Figure 8.8). The expanded distal end of each metacarpal bone articulates at the metacarpophalangeal joint with the proximal phalanx bone of the thumb or one of the fingers. The distal end also forms the knuckles of the hand, at the base of the fingers. The metacarpal bones are numbered 1–5, beginning at the pollex (thumb).
The first metacarpal bone, at the base of the pollex, is separated from the other metacarpal bones. This allows it a freedom of motion that is independent of the other metacarpal bones, which is very important for thumb mobility. The remaining metacarpal bones are united together to form the palm of the hand.
Phalanges
The fingers and thumb contain 14 bones, each of which is called a phalanx (plural = phalanges), named after the ancient Greek phalanx (a rectangular block of soldiers). The pollex is digit number 1 and has two phalanges, a proximal phalanx and a distal phalanx (see Figure 8.7). Digits 2 (index finger) through 5 (little finger) have three phalanges each, called the proximal, middle and distal phalanges. An interphalangeal joint is one of the articulations between adjacent phalanges of the digits (see Figure 8.8).
Appendicular: The Pelvic Girdle and Bony Pelvis
Learning Objectives
By the end of this section, you will be able to:
- Define the pelvic girdle and describe the bones of the pelvis
- Explain the three regions of the os coxa and identify their bony landmarks
The pelvic girdle is formed by a paired bone, the os coxae (coxa = “hip”), coxal bones or hip bones, which serve as the attachment point for each lower limb at the hip (coxal) joint. The right and left hip bones also converge anteriorly to attach to each other at the pubic symphysis. Each os coxa, in turn, is firmly joined to the axial skeleton via its attachment to the sacrum of the vertebral column. The bony pelvis is the entire structure formed by the two os coxae, the sacrum, and, attached inferiorly to the sacrum and the coccyx (Figure 8.12).
Unlike the bones of the pectoral girdle, which are highly mobile to enhance the range of upper limb movements, the bones of the pelvis are strongly united to each other to form a largely immobile, weight-bearing structure. This is important for stability because it enables the weight of the body to be easily transferred laterally from the vertebral column, through the pelvic girdle and hip joints, and into either lower limb whenever the other limb is not bearing weight. Thus, the immobility of the bony pelvis provides a strong foundation for the upper body as it rests on top of the lower limbs.
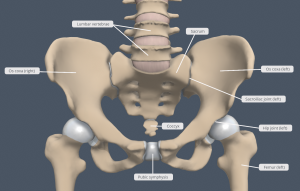
Figure 8.12 Bony Pelvis (Anterior view) The pelvic girdle is formed by the paired os coxae, which articulate anteriorly at the pubic symphysis. The hip bone attaches the lower limb to the axial skeleton through its articulation with the sacrum at the sacroiliac joints. The right and left hip bones, plus the sacrum and the coccyx, together form the bony pelvis. [Created in Anatomy.TV, Primal Pictures]
Hip Bone
The hip bone, or os coxa, forms the pelvic girdle portion of the pelvis. The paired hip bones are the large, curved bones that form the lateral and anterior aspects of the bony pelvis. Each adult hip bone is formed by three separate bones that fuse together during the late teenage years. These bony components are the ilium, ischium, and pubis (Figure 8.13). These names are retained and used to define the three regions of the adult hip bone. The ilium is the fan-like, superior region that forms the largest part of the hip bone. It is firmly united to the sacrum at the largely immobile sacroiliac joint (see Figure 8.12). The ischium forms the posteroinferior region of each hip bone. It supports the body when sitting. The pubis forms the anterior portion of the hip bone. The pubis curves medially, where it joins to the pubis of the contralateral hip bone at a specialised joint called the pubic symphysis.
INTERACTIVE ACTIVITY
Question:
(a) Why do we describe the os coxa as having three parts? What is the developmental origin of these parts?
The three areas of each hip bone, the ilium, pubis, and ischium, converge centrally to form a deep, cup-shaped cavity called the acetabulum. This is located on the lateral side of the hip bone and is part of the hip (coxal) joint. The large opening in the anteroinferior hip bone between the ischium and pubis is the obturator foramen. The obturator nerve and blood vessels pass through this foramen to enter the lower limb from the pelvis.
INTERACTIVE ACTIVITY
Appendicular: Bones of the Lower Limb
Learning Objectives
By the end of this section, you will be able to:
- Identify the divisions of the lower limb and describe the bones of each region
- Describe the bones and bony landmarks that articulate at each joint of the lower limb
Like the upper limb, the lower limb is divided into three regions. The femoral region (thigh) is that portion of the lower limb located between the hip joint and knee joint. The crural region (leg) is specifically the region between the knee joint and the talocrural (ankle) joint. Distal to the talocrural joint is the foot. The lower limb contains 30 bones. These are the femur, patella, tibia, fibula, tarsal bones, metatarsal bones and phalanges (see Figure 8.2). The femur is the single bone of the thigh. The patella is the kneecap and articulates with the distal femur. The tibia is the larger, weight-bearing bone located on the medial side of the leg, and the fibula is the thin bone of the lateral leg. The bones of the foot are divided into three groups. The posterior portion of the foot is formed by a group of seven bones, each of which is known as a tarsal bone, whereas the mid-foot contains five elongated bones, each of which is a metatarsal bone. The toes contain 14 small bones, each of which is a phalanx of the foot.
Femur
The femur is the single bone of the thigh region (Figure 8.16). It is the longest and strongest bone of the body, and accounts for approximately one-quarter of a person’s total height. The rounded, proximal end is the head of the femur, which articulates with the acetabulum of the hip bone to form the hip joint.
The greater trochanter is the large, superior, bony projection located lateral to the head of the femur. Multiple muscles that act across the hip joint attach to the greater trochanter, which, because of its projection from the femur, gives additional leverage to these muscles. The greater trochanter can be palpated just deep to the skin on the lateral side of your superior femoral region. The lesser trochanter is a small, bony prominence that lies on the medial and posterior aspect of the femur, distal to the greater trochanter.
The elongated shaft of the femur has a slight anterior bowing or curvature. The shaft of the femur is marked posteriorly by a longitudinal roughened ridge called the linea aspera (“rough line”). Multiple muscles of the hip and thigh regions make long, thin attachments to the femur along the linea aspera.
The distal end of the femur has medial and lateral bony expansions. On the lateral side, the smooth portion that covers the distal and posterior aspects of the lateral expansion is the lateral condyle of the femur. Similarly, the smooth region of the distal and posterior medial femur is the medial condyle of the femur, and the irregular outer, medial side of this is the medial epicondyle of the femur. The lateral and medial condyles articulate with the tibia to form the knee joint. Posteriorly, the medial and lateral condyles are separated by a deep depression called the intercondylar notch. Anteriorly, the smooth surfaces of the condyles join together to form a wide groove called the patellar surface, which provides articulation with the patella as part of the knee joint articulations.

Figure 8.16 Femur (Posterior view) The femur is the single bone of the femoral (thigh) region. It articulates superiorly with the hip bone at the hip joint at the head of the femur, and inferiorly with the tibia at the knee joint at the medial and lateral femoral condyles. The patella articulates with the distal end of the femur anteriorly (not visible in this posterior view of the femur). [Created in Anatomy.TV, Primal Pictures]
Patella
The patella (kneecap) is the largest sesamoid bone of the body (see Figure 8.16). A sesamoid bone is a bone that is incorporated into the tendon of a muscle where that tendon crosses a joint. The patella is found in the tendon of the quadriceps femoris muscle, the large muscle of the anterior thigh that passes across the anterior knee to attach to the tibia. The patella articulates with the patellar surface of the femur and thus prevents rubbing of the muscle tendon against the distal femur. The patella also lifts the tendon away from the knee joint, which increases the leverage power of the quadriceps femoris muscle as it acts across the knee. The patella does not articulate with the tibia.
Tibia
The tibia is the medial bone of the crural region (leg) and is larger than the fibula, with which it is paired (Figure 8.18). The tibia is the main weight-bearing bone of the leg and the second longest bone of the body, after the femur. The medial side of the tibia is located immediately deep to the skin, allowing it to be easily palpated down the entire length of the medial leg.
The proximal end of the tibia is greatly expanded. The two sides of this expansion form the medial condyle of the tibia and the lateral condyle of the tibia. The superior surface of each condyle is smooth and flattened. These areas articulate with the medial and lateral condyles of the femur to form the knee joint. Between the articulating surfaces of the tibial condyles are roughened areas for attachment of the cruciate ligaments and menisci called the anterior and posterior intercondylar fossae.
The tibial tuberosity is an elevated area on the anterior side of the tibia, near its proximal end. It is the final site of attachment for the quadriceps femoris muscle tendon (also known as the patellar ligament as it passes from the patella to the tibial tuberosity). A small ridge running down the lateral side of the tibial shaft is the interosseous border of the tibia. This is for the attachment of the interosseous membrane of the leg, the sheet of dense connective tissue that unites the tibia and fibula.
The large expansion found on the medial side of the distal tibia is the medial malleolus (“little hammer”). This forms the large bony bump found on the medial side of the tarsal (ankle) region. Both the smooth surface on the inside of the medial malleolus and the smooth area at the distal end of the tibia articulate with the talus bone of the foot as part of the talocrural (ankle) joint.
INTERACTIVE ACTIVITY
Fibula
The fibula is the slender bone located on the lateral side of the leg (see Figure 8.18). The fibula does not bear weight. It serves primarily for muscle attachments and thus is largely surrounded by muscles. Only the proximal and distal ends of the fibula can be palpated.
The head of the fibula is the small, knob-like, proximal end of the fibula. It articulates with the inferior aspect of the lateral tibial condyle, forming the proximal tibiofibular joint. The thin shaft of the fibula has the interosseous border of the fibula, a narrow ridge running down its medial side for the attachment of the interosseous membrane that spans the fibula and tibia. The distal end of the fibula forms the lateral malleolus, which forms the easily palpated bony bump on the lateral side of the ankle. The deep (medial) side of the lateral malleolus articulates with the talus bone of the foot as part of the talocrural joint.
Tarsal Bones
The posterior half of the foot is formed by seven tarsal bones (Figure 8.19). The most superior bone is the talus. This has a relatively square-shaped, superior surface that articulates with the tibia and fibula to form the talocrural (ankle) joint. Three areas of articulation form the talocrural joint: The superomedial surface of the talus bone articulates with the medial malleolus of the tibia, the superior surface of the talus articulates with the distal end of the tibia, and the lateral side of the talus articulates with the lateral malleolus of the fibula. Inferiorly, the talus articulates with the calcaneus (heel bone), the largest bone of the foot, which forms the heel. Body weight is transferred from the tibia to the talus to the calcaneus, which rests on the ground.
The cuboid bone articulates with the anterior end of the calcaneus bone. The talus bone articulates anteriorly with the navicular bone, which in turn articulates anteriorly with the three cuneiform (“wedge-shaped”) bones. These bones are the medial cuneiform, the intermediate cuneiform, and the lateral cuneiform.
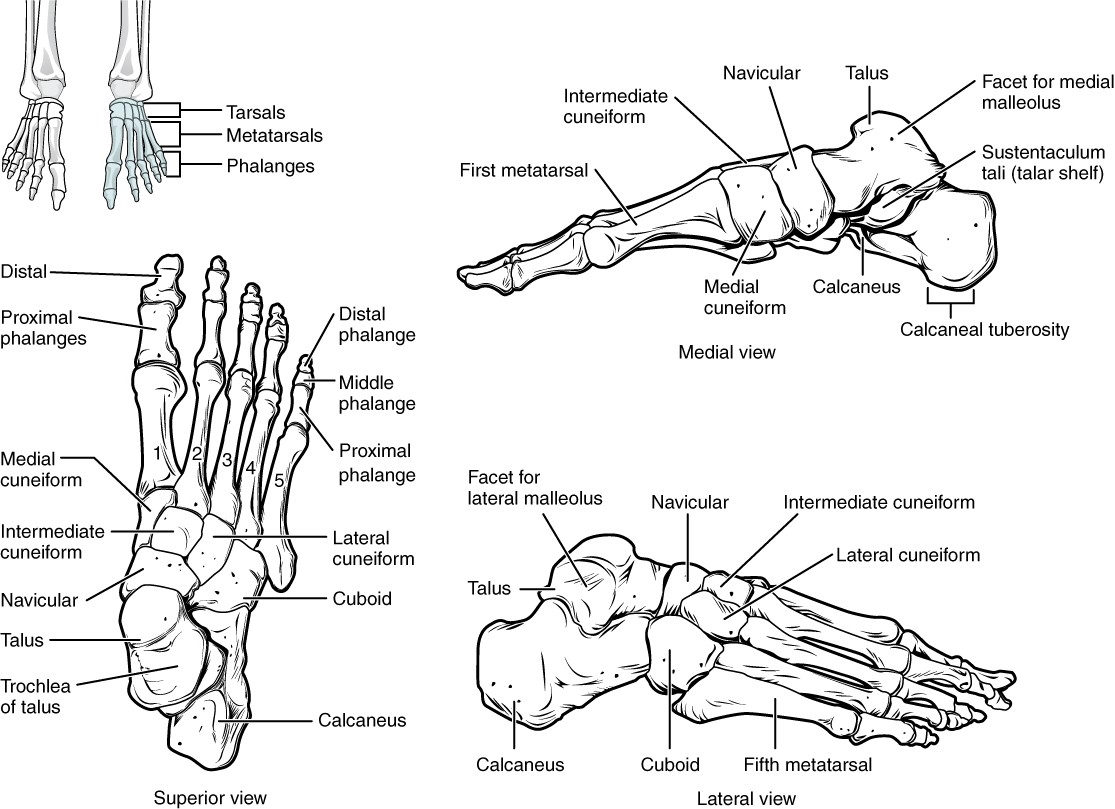
Figure 8.19 Bones of the Foot The bones of the foot are divided into three groups. The posterior foot is formed by the seven tarsal bones. The mid-foot has the five metatarsal bones. The toes contain the phalanges.
INTERACTIVE ACTIVITY
Metatarsal Bones
The anterior half of the foot is formed by the five metatarsal bones, which are located between the tarsal bones of the posterior foot and the phalanges of the toes (see Figure 8.19). These elongated bones are numbered 1–5, starting with the medial side of the foot. The first metatarsal bone is shorter and thicker than the others. The second metatarsal is the longest. Each metatarsal bone articulates with the proximal phalanx of a toe to form a metatarsophalangeal joint. The distal ends of the metatarsal bones rest on the ground and form the ball (anterior end) of the foot.
Phalanges
The toes contain a total of 14 phalanges, arranged in a similar manner as the phalanges of the fingers (see Figure 8.19). The toes are numbered 1–5, starting with the big toe (hallux). The big toe has two phalanges, the proximal and distal phalanges. The remaining toes all have proximal, middle and distal phalanges. A joint between adjacent phalanges is called an interphalangeal joint.
Classification of Joints
Learning Objectives
After studying this section, you will be able to:
- Discuss both functional and structural classifications for joints
- Describe the characteristic features of fibrous, cartilaginous, and synovial joints and give examples of each
The adult human body has 206 bones, and with the exception of the hyoid bone in the neck, each bone is connected to at least one other bone. A joint, also called an articulation, is any place where adjacent bones or bone and cartilage come together (articulate with each other) to form a connection. Many joints allow for movement between the bones. At these joints, the articulating surfaces of the adjacent bones can move smoothly against each other. However, the bones of other joints may be joined to each other by connective tissue or cartilage. These joints are designed for stability and provide little or no movement. Conversely, joints that provide the most movement between bones are the least stable. Understanding the relationship between joint structure and function will help to explain why particular types of joints are found in certain areas of the body.
Joints are classified both structurally and functionally. Structural classifications of joints take into account whether the adjacent bones are strongly anchored to each other by fibrous connective tissue or cartilage, or whether the adjacent bones articulate with each other within a fluid-filled space called a joint cavity. Functional classifications describe the degree of movement available between the bones, ranging from immobile, to slightly mobile, to freely moveable joints. The amount of movement available at a particular joint of the body is related to the functional requirements for that joint. Thus immobile or slightly moveable joints serve to protect internal organs, give stability to the body, and allow for limited body movement. In contrast, freely moveable joints allow for much more extensive movements of the body and limbs.
Functional Classification of Joints
The functional classification of joints is determined by the amount of mobility found between the adjacent bones. Joints are thus functionally classified as a synarthrosis or immobile joint, an amphiarthrosis or slightly moveable joint, or as a diarthrosis, which is a freely moveable joint (arthroun = “to fasten by a joint”).
Structural Classification of Joints
The structural classification of joints is based on whether the articulating surfaces of the adjacent bones are directly connected by fibrous connective tissue or cartilage, or whether the articulating surfaces contact each other within a fluid- filled joint cavity. These differences serve to divide the joints of the body into three structural classifications. A fibrous joint is where the adjacent bones are united by fibrous connective tissue. At a cartilaginous joint, the bones are joined by hyaline cartilage or fibrocartilage. At a synovial joint, the articulating surfaces of the bones are not directly connected, but instead come into contact with each other within a joint cavity that is filled with a lubricating fluid. Synovial joints allow for free movement between the bones and are the most common joints of the body.
Fibrous Joints
At a fibrous joint, the adjacent bones are directly connected to each other by fibrous connective tissue, and thus the bones do not have a joint cavity between them (Figure 9.5). The gap between the bones may be narrow or wide. There are three types of fibrous joints: sutures, syndesmoses and gomphoses.
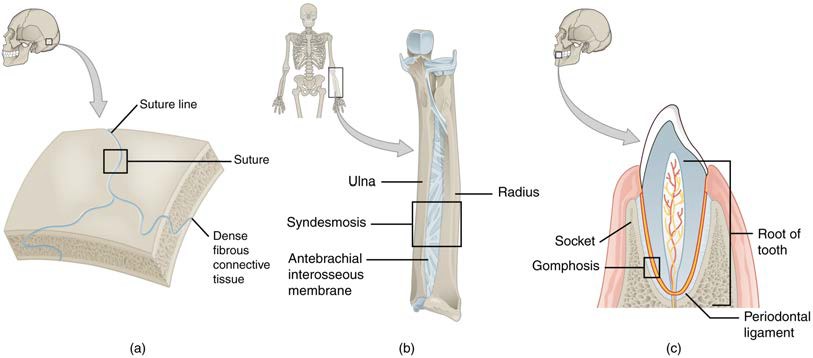
Figure 9.5 Fibrous Joint Classification Fibrous joints form strong connections between bones. (a) Sutures join most bones of the skull. (b) An interosseous membrane forms a syndesmosis between the radius and ulna of the antebrachium. (c) A gomphosis is a specialised fibrous joint that anchors a tooth to its socket in the upper and lower jaws.
Cartilaginous Joints
As the name indicates, at a cartilaginous joint, the adjacent bones are united by cartilage, a tough but flexible type of connective tissue. These types of joints lack a joint cavity and involve bones that are joined together by either hyaline cartilage or fibrocartilage (Figure 9.7). There are two types of cartilaginous joints: synchondroses (hyaline cartilage) and symphyses (fibrocartilage).
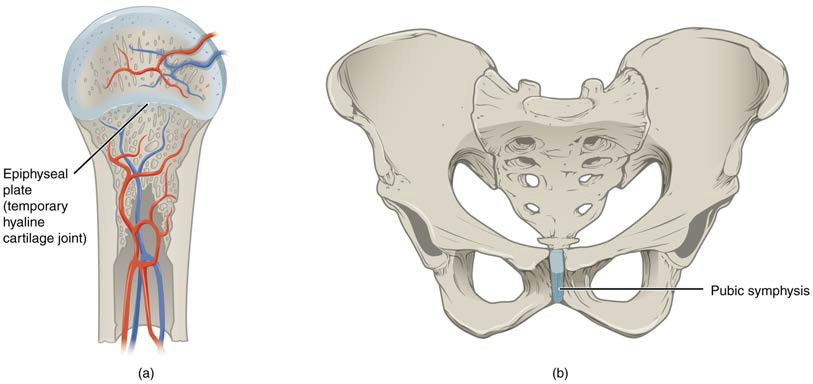
Figure 9.7 Cartiliginous Joints At cartilaginous joints, bones are united by hyaline cartilage to form a synchondrosis or by fibrocartilage to form a symphysis. (a) The hyaline cartilage of the epiphyseal plate (growth plate) forms a temporary synchondrosis that unites the shaft (diaphysis) and end (epiphysis) of a long bone and allows the bone to grow in length. (b) The pubic portions of the right and left hip bones of the pelvis are joined together by fibrocartilage, forming the pubic symphysis.
Synovial Joints
Learning Objectives
After studying this section, you will be able to:
- Describe the components of a typical synovial joint
- Describe the synovial joint subtypes
- Examine the structure of the knee joint and coxal joint
Synovial joints are the most common type of joint in the body (Figure 9.8). A key structural characteristic for a synovial joint that is not seen at fibrous or cartilaginous joints is the presence of a joint cavity. This fluid-filled space is the site at which the articulating surfaces of the bones contact each other. Also unlike fibrous or cartilaginous joints, the articulating bone surfaces at a synovial joint are not directly connected to each other with fibrous connective tissue or cartilage. This gives the bones of a synovial joint the ability to move smoothly against each other, allowing for increased joint mobility. Therefore all synovial joints are functionally classified as diarthroses.
Structural Features of Synovial Joints
Synovial joints are characterised by the presence of a joint cavity. The walls of this space are formed by the articular or fibrous capsule, a dense irregular connective tissue structure that is attached to each bone just external to the area of the bone’s articulating surface. Friction between the bones at a synovial joint is prevented by the presence of the articular cartilage, a thin layer of hyaline cartilage that covers the entire articulating surface of each bone. The articular cartilage allows the articulating bones to move smoothly against each other without damaging the underlying bone tissue.
Lining the internal surface of the articular capsule is a thin synovial membrane. The cells of this membrane secrete synovial fluid (synovia = “a thick fluid”), a thick, slimy fluid that provides lubrication to further reduce friction between the bones of the joint. This fluid also provides nourishment to the articular cartilage, which does not contain blood vessels.
Outside of their articulating surfaces, the bones are connected together by ligaments, which are strong bands of dense regular connective tissue. These strengthen and support the joint by anchoring the bones together and preventing their separation. Ligaments allow for normal movements at a joint, but limit the range of these motions, thus preventing excessive or abnormal joint movements. Ligaments are classified based on their relationship to the fibrous capsule. An extracapsular ligament is located outside of the articular capsule, an intracapsular ligament is located inside of the fibrous capsule.
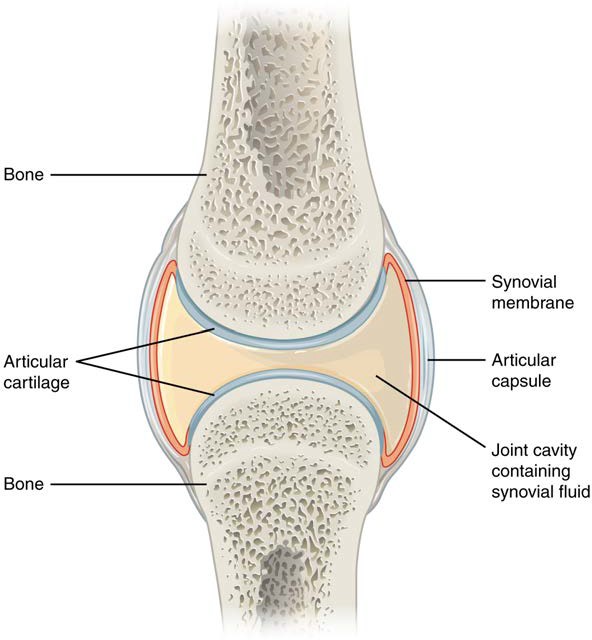
Figure 9.8 Synovial Joints Synovial joints allow for smooth movements between the adjacent bones. The joint is surrounded by an articular capsule that defines a joint cavity filled with synovial fluid. The articulating surfaces of the bones are covered by a thin layer of articular cartilage. Ligaments support the joint by holding the bones together and resisting excess or abnormal joint motions.
Additional Structures Associated with Synovial Joints
A few synovial joints of the body have a fibrocartilage structure located between the articulating bones. This is called an articular disc, which is generally small and oval-shaped, a labrum, which is a lip of fibrocartilaginous tissue that acts to deepen and increase the stabilisation of a joint surface, or a meniscus, which is larger and C-shaped. These structures can serve several functions, depending on the specific joint. The fibrocartilaginous structures can provide shock absorption and cushioning between the bones, which is the function of each meniscus within the knee joint. Fibrocartilaginous labra (pl; labrum = singular) can be found in the glenohumeral and hip joints.
Additional structures located outside of a synovial joint serve to prevent friction between the bones of the joint and the overlying muscle tendons or skin. A bursa (plural = bursae) is a thin connective tissue sac filled with lubricating liquid. They are located in regions where skin, ligaments, muscles, or muscle tendons can rub against each other, usually near a body joint (Figure 9.9). Bursae reduce friction by separating the adjacent structures, preventing them from rubbing directly against each other.
Types of Synovial Joints
Synovial joints are subdivided based on the shapes of the articulating surfaces of the bones that form each joint. The six types of synovial joints are pivot, hinge, condyloid, saddle, plane, and ball-and socket-joints (Figure 9.10).
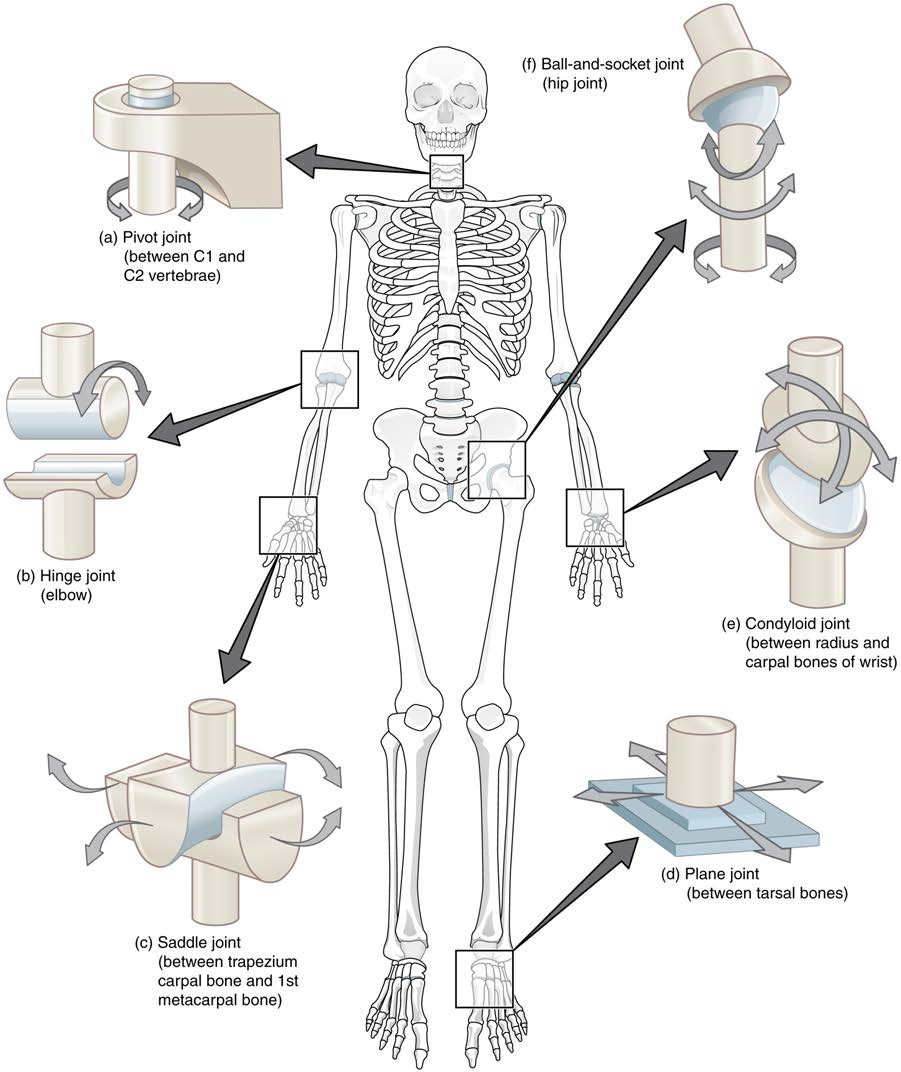
Figure 9.10 Types of Synovial Joints The six types of synovial joints allow the body to move in a variety of ways. (a) Pivot joints allow for rotation around an axis, such as between the first and second cervical vertebrae, which allows for side-to-side rotation of the head. (b) The hinge joint of the elbow works like a door hinge. (c) The articulation between the trapezium carpal bone and the first metacarpal bone at the base of the pollex is a saddle joint. (d) Plane joints, such as those between the tarsal bones of the foot, allow for limited gliding movements between bones. (e) The radiocarpal joint of the carpus is a condyloid joint. (f) The hip and glenohumeral joints are the only ball-and-socket joints of the body.
INTERACTIVE ACTIVITY
Knee Joint
The knee joint is the largest joint of the body (Figure 9.19). It actually consists of three articulations. The femoropatellar joint is found between the patella and the distal femur. The medial tibiofemoral joint and lateral tibiofemoral joint are located between the medial and lateral condyles of the femur and the medial and lateral condyles of the tibia. All of these articulations are enclosed within a single articular capsule. The knee functions as a hinge joint, allowing flexion and extension of the knee joint.
Located between the articulating surfaces of the femur and tibia are two articular discs, the medial meniscus and lateral meniscus (see Figure 9.19b). Each is a C-shaped fibrocartilage structure that is thin along its internal margin and thick along the external margin. They are attached to their tibial condyles, but do not attach to the femur. While both menisci are free to move during knee motions, the medial meniscus shows less movement because it is anchored at its external margin to the articular capsule and tibial/medial collateral ligament. The menisci provide padding between the bones and help to fill the gap between the round femoral condyles and flattened tibial condyles.
The knee joint has multiple ligaments that provide support it (see Figure 9.19c). Outside of the articular capsule, located lateral to the knee, are two extrinsic ligaments. The fibular collateral ligament is on the lateral side and spans from the lateral epicondyle of the femur to the head of the fibula. The tibial collateral ligament of the medial knee runs from the medial epicondyle of the femur to the medial tibia. In the fully extended knee position, both collateral ligaments are taut (tight), thus serving to stabilise and support the extended knee and preventing side-to-side or rotational motions between the femur and tibia.
The articular capsule of the posterior knee is thickened by intrinsic ligaments that help to resist knee hyperextension. Inside the knee are two intracapsular ligaments, the anterior cruciate ligament and posterior cruciate ligament. The cruciate ligaments are named for whether they are attach to the anterior or posterior intercondylar fossa. Each ligament runs diagonally superiorly to attach to the internal aspect of a femoral condyle (intercondylar notch). The cruciate ligaments are named for the X-shape formed as they pass each other (cruciate means “cross”).
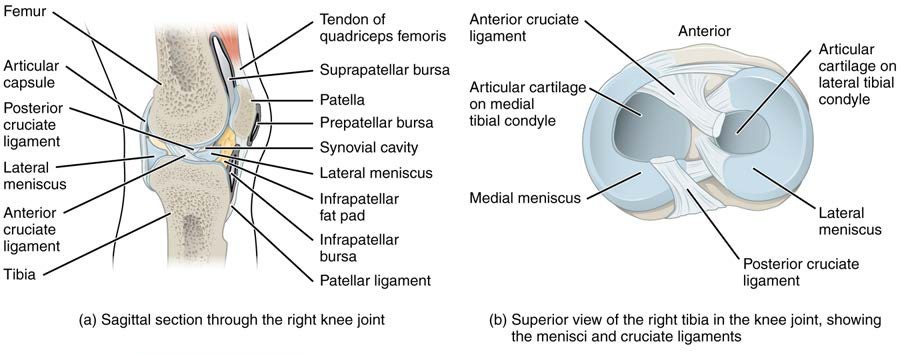
Figure 9.19 Knee Joint (a) The knee joint is the largest joint of the body. (b) It is supported by the tibial and fibular collateral ligaments located on the sides of the knee external to the articular capsule, and the anterior and posterior cruciate ligaments found inside the capsule. The medial and lateral menisci provide padding and support between the femoral condyles and tibial condyles.
Hip Joint
The hip (coxal) joint is a multiaxial ball-and-socket joint between the head of the femur and the acetabulum of the hip bone (Figure 9.18). The hip carries the weight of the body and thus requires strength and stability during standing and walking. For these reasons, its range of motion is more limited than at the glenohumeral joint.
The acetabulum is the socket portion of the hip joint. This space is deep and has a large articulation area for the femoral head, thus giving stability and weight bearing ability to the joint. The acetabulum is further deepened by the acetabular labrum, a fibrocartilage lip attached to the external margin of the acetabulum. The surrounding articular capsule is strong, and is reinforced by a number of extracapsular ligaments called the iliofemoral, ischiofemoral and pubofemoral ligaments.
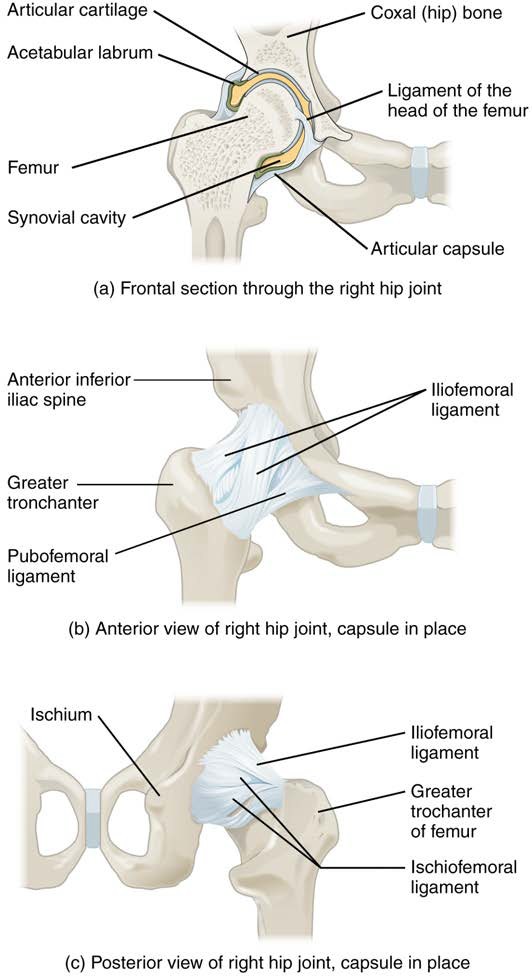
Figure 9.18 Hip Joint (a) The ball-and-socket joint of the hip is a multiaxial joint that provides both stability and a wide range of motion. (b–c) When standing, the supporting ligaments are tight, pulling the head of the femur into the acetabulum.
Types of Body Movements
Learning Objectives
By the end of this section, you will be able to:
- Define the different types of body movements
- Identify the joints that allow for these motions
Synovial joints allow the body a tremendous range of movement. The type of movement that can be produced at a synovial joint is determined by its structural type. While the ball-and-socket joint gives the greatest range of movement at an individual joint, in other regions of the body, several joints may work together to produce a particular movement. There are many types of movements that can occur at synovial joints (Table 9.1). Movement types are generally paired, with one being the opposite of the other. Body movements are always described in relation to the anatomical position of the body: erect stance, with upper limbs to the side of body and palms facing anteriorly. Refer to Figure 9.12 as you go through this section.
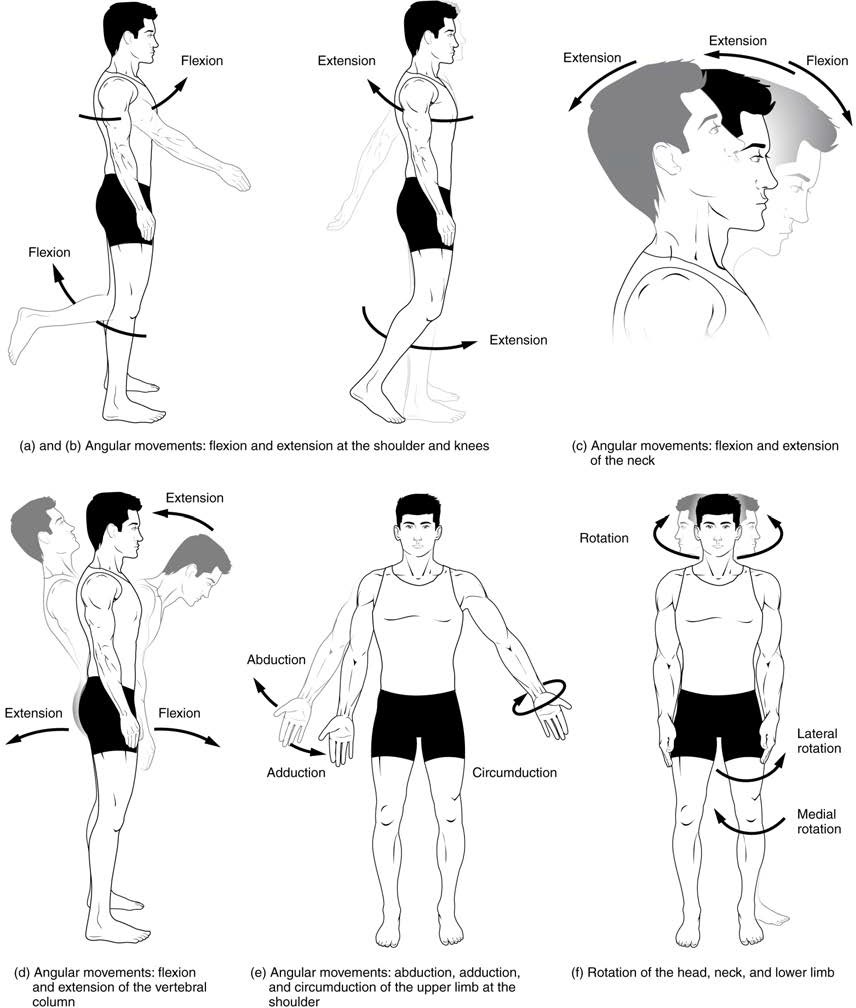
Figure 9.12 Movements of the Body, Part 1 Synovial joints give the body many ways in which to move. (a)–(b) Flexion and extension motions are in the sagittal (anterior–posterior) plane of motion. These movements take place at the glenohumeral, hip, elbow, knee, radiocarpal, metacarpophalangeal, metatarsophalangeal, and interphalangeal joints. (c)–(d) Anterior bending of the head or vertebral column is flexion, while any posterior-going movement is extension. (e) Abduction and adduction are motions of the limbs, hand, fingers, or toes in the coronal (medial–lateral) plane of movement. Moving the limb or hand laterally away from the body, or spreading the fingers or toes, is abduction. Adduction brings the limb or hand toward or across the midline of the body, or brings the fingers or toes together. Circumduction is the movement of the limb, hand, or fingers in a circular pattern, using the sequential combination of flexion, adduction, extension, and abduction motions. Adduction/abduction and circumduction take place at the glenohumearl, hip, radiocarpal, metacarpophalangeal, and metatarsophalangeal joints. (f) Turning of the head side to side or twisting of the body is rotation. Medial and lateral rotation of the upper limb at the glenohumeral joint or lower limb at the hip involves turning the anterior surface of the limb toward the midline of the body (medial or internal rotation) or away from the midline (lateral or external rotation).
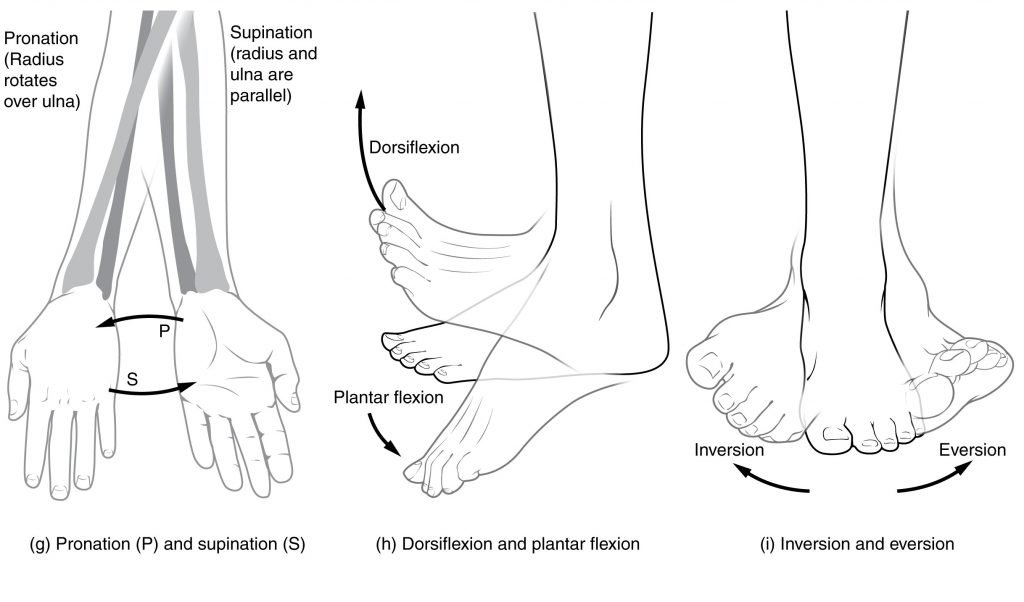
Figure 9.13 Movements of the Body, Part 2 (g) Supination of the antebrachium (forearm) turns the palm to the anterior position in which the radius and ulna are parallel, while forearm pronation turns the palm into a posterior position in which the radius crosses over the ulna to form an “X.” (h) Dorsiflexion of the foot at the talocrural joint moves the dorsum (top) of the foot toward the leg, while plantar flexion lifts the heel and points the toes. (i) Eversion of the foot moves the bottom (sole) of the foot away from the midline of the body, while foot inversion faces the sole toward the midline.
Table 9.1 Movements of the Joints
| Type of Joint | Movement | Example |
| Pivot | Uniaxial joint; allows rotational movement | Atlantoaxial joint (C1–C2 vertebrae articulation); proximal radioulnar joint |
| Hinge | Uniaxial joint; allows flexion/extension movements | Knee; elbow; ankle; interphalangeal joints of fingers and toes |
| Condyloid | Biaxial joint; allows flexion/extension, abduction/ adduction, and circumduction movements | Metacarpophalangeal (knuckle) joints of fingers; radiocarpal joint of wrist; metatarsophalangeal joints for toes |
| Saddle | Biaxial joint; allows flexion/extension, abduction/ adduction, and circumduction movements | First carpometacarpal joint of the thumb; sternoclavicular joint |
| Plane | Multiaxial joint; allows inversion and eversion of foot, or flexion, extension, and lateral flexion of the vertebral column | Intertarsal joints of foot; superior-inferior articular process articulations between vertebrae |
| Ball-and- socket | Multiaxial joint; allows flexion/extension, abduction/adduction, circumduction, and medial/ lateral rotation movements | Shoulder and hip joints |
Key Terms
abduction movement in the coronal plane that moves a limb laterally away from the body; spreading of the fingers
acetabular labrum lip of fibrocartilage that surrounds outer margin of the acetabulum on the hip bone
acetabulum large, cup-shaped cavity located on the lateral side of the hip bone; formed by the junction of the ilium, pubis, and ischium portions of the hip bone
acromial end of the clavicle lateral end of the clavicle that articulates with the acromion of the scapula
acromial process acromion of the scapula; flattened bony process that extends laterally from the scapular spine to form the bony tip of the shoulder
acromioclavicular joint articulation between the acromion of the scapula and the acromial end of the clavicle
adduction movement in the coronal plane that moves a limb medially toward or across the midline of the body; bringing fingers together all bones of the upper and lower limbs, plus the girdle bones that attach each limb to the axial skeleton
alveolar process of the mandible upper border of mandibular body that contains the lower teeth
alveolar process of the maxilla curved, inferior margin of the maxilla that supports and anchors the upper teeth
amphiarthrosis slightly mobile joint
antebrachium region of the upper limb located between the elbow and wrist joints; contains the radius and ulna bones
anterior (ventral) sacral foramen one of the series of paired openings located on the anterior (ventral) side of the sacrum
anterior arch anterior portion of the ring-like C1 (atlas) vertebra
anterior cranial fossa shallowest and most anterior cranial fossa of the cranial base that extends from the frontal bone to the lesser wing of the sphenoid bone anterior longitudinal ligament the vertebral bodies ligament that runs the length of the vertebral column, uniting the anterior aspects of
anterior cruciate ligament intracapsular ligament of the knee; extends from anterior, superior surface of the tibia to the inner aspect of the lateral condyle of the femur; resists hyperextension of knee
anterior superior iliac spine rounded, anterior end of the iliac crest
anulus fibrosus tough, fibrous outer portion of an intervertebral disc, which is strongly anchored to the bodies of the adjacent vertebrae
appendicular skeleton the portion of the skeleton consisting of the bones that support the skeleton
articular capsule connective tissue structure that encloses the joint cavity of a synovial joint
articular cartilage thin layer of hyaline cartilage that covers the articulating surfaces of bones at a synovial joint
articular disc meniscus; a fibrocartilage structure found between the bones of some synovial joints; provides padding or smooths movements between the bones; strongly unites the bones together
articulation where two bone surfaces meet to form a joint
atlantoaxial joint series of three articulations between the atlas (C1) vertebra and the axis (C2) vertebra, consisting of the joints between the inferior articular processes of C1 and the superior articular processes of C2, and the articulation between the dens of C2 and the anterior arch of C1
atlanto-occipital joint articulation between the occipital condyles of the skull and the superior articular processes of the atlas (C1 vertebra)
atlas first cervical (C1) vertebra
auditory ossicles three small bones located in the middle ear cavity that serve to transmit sound vibrations to the inner ear
auricular surface of the ilium roughened area located on the posterior, medial side of the ilium of the hip bone; articulates with the auricular surface of the sacrum to form the sacroiliac joint
axial skeleton central, vertical axis of the body, including the skull, vertebral column, and thoracic cage
axis second cervical (C2) vertebra
ball-and-socket joint synovial joint formed between the spherical end of one bone (the ball) that fits into the depression of a second bone (the socket); found at the hip and shoulder joints; functionally classified as a multiaxial joint
biaxial joint type of diarthrosis; a joint that allows for movements within two planes (two axes)
brachium region of the upper limb located between the shoulder and elbow joints; contains the humerus bone
bursa connective tissue sac containing lubricating fluid that prevents friction between adjacent structures, such as skin and bone, tendons and bone, or between muscles
calcaneus heel bone; posterior, inferior tarsal bone that forms the heel of the foot
calvaria (also, skullcap) rounded top of the skull
capitate from the lateral side, the third of the four distal carpal bones; articulates with the scaphoid and lunate proximally, the trapezoid laterally, the hamate medially, and primarily with the third metacarpal distally
capitulum knob-like bony structure located anteriorly on the lateral, distal end of the humerus
carotid canal zig-zag tunnel providing passage through the base of the skull for the internal carotid artery to the brain; begins anteromedial to the styloid process and terminates in the middle cranial cavity, near the posterior-lateral base of the sella turcica
carpal bone one of the eight small bones that form the wrist and base of the hand; these are grouped as a proximal row consisting of (from lateral to medial) the scaphoid, lunate, triquetrum, and pisiform bones, and a distal row containing (from lateral to medial) the trapezium, trapezoid, capitate, and hamate bones
carpometacarpal joint articulation between one of the carpal bones in the distal row and a metacarpal bone of the hand
cartilaginous joint joint at which the bones are united by hyaline cartilage (synchondrosis) or fibrocartilage (symphysis)
cervical curvature posteriorly concave curvature of the cervical vertebral column region; a secondary curve of the vertebral column
cervical vertebrae seven vertebrae numbered as C1–C7 that are located in the neck region of the vertebral column
circumduction circular motion of the arm, thigh, hand, thumb, or finger that is produced by the sequential combination of flexion, abduction, extension, and adduction
clavicle collarbone; elongated bone that articulates with the manubrium of the sternum medially and the acromion of the scapula laterally
coccyx small bone located at inferior end of the adult vertebral column that is formed by the fusion of four coccygeal vertebrae; also referred to as the “tailbone”
condyloid joint synovial joint in which the shallow depression at the end of one bone receives a rounded end from a second bone or a rounded structure formed by two bones; found at the metacarpophalangeal joints of the fingers or the radiocarpal joint of the wrist; functionally classified as a biaxial joint
coracoid process short, hook-like process that projects anteriorly and laterally from the superior margin of the scapula
coronal suture joint that unites the frontal bone to the right and left parietal bones across the top of the skull
costal cartilage hyaline cartilage structure attached to the anterior end of each rib that provides for either direct or indirect attachment of most ribs to the sternum
costal facet site on the lateral sides of a thoracic vertebra for articulation with the head of a rib
costal groove shallow groove along the inferior margin of a rib that provides passage for blood vessels and a nerve
coxal bone hip bone
cranial cavity interior space of the skull that houses the brain
cranium skull
cuboid tarsal bone that articulates posteriorly with the calcaneus bone, medially with the lateral cuneiform bone, and anteriorly with the fourth and fifth metatarsal bones
deltoid tuberosity roughened, V-shaped region located laterally on the mid-shaft of the humerus
dens bony projection (odontoid process) that extends upward from the body of the C2 (axis) vertebra
diaphysis tubular shaft that runs between the proximal and distal ends of a long bone
diarthrosis freely mobile joint
distal radioulnar joint articulation between the head of the ulna and the ulnar notch of the radius
dorsiflexion movement at the ankle that brings the top of the foot toward the anterior leg
elbow joint joint located between the upper arm and forearm regions of the upper limb; formed by the articulations between the trochlea of the humerus and the trochlear notch of the ulna, and the capitulum of the humerus and the head of the radius
endochondral ossification process in which bone forms by replacing hyaline cartilage
endosteum delicate membranous lining of a bone’s medullary cavity enlarged prominence located on the lateral side of the proximal humerus
epiphyseal line completely ossified remnant of the epiphyseal plate
epiphyseal plate (also, growth plate) sheet of hyaline cartilage in the metaphysis of an immature bone; replaced by bone tissue as the organ grows in length
epiphysis wide section at each end of a long bone; filled with spongy bone and red marrow
ethmoid air cell one of several small, air-filled spaces located within the lateral sides of the ethmoid bone, between the orbit and upper nasal cavity
ethmoid bone unpaired bone that forms the roof and upper, lateral walls of the nasal cavity, portions of the floor of the anterior cranial fossa and medial wall of orbit, and the upper portion of the nasal septum
eversion foot movement involving the intertarsal joints of the foot in which the bottom of the foot is turned laterally, away from the midline
extension movement in the sagittal plane that increases the angle of a joint (straightens the joint); motion involving posterior bending of the vertebral column or returning to the upright position from a flexed position
external acoustic meatus ear canal opening located on the lateral side of the skull
external occipital protuberance small bump located at the midline on the posterior skull
extracapsular ligament ligament located outside of the articular capsule of a synovial joint
facet small, flattened area on a bone for an articulation (joint) with another bone, or for muscle attachment
facial bones fourteen bones that support the facial structures and form the upper and lower jaws and the hard palate
false ribs vertebrochondral ribs 8–12 whose costal cartilage either attaches indirectly to the sternum via the costal cartilage of the next higher rib or does not attach to the sternum at all
femoropatellar joint portion of the knee joint consisting of the articulation between the distal femur and the patella
femur thigh bone; the single bone of the thigh
fibrous joint joint where the articulating areas of the adjacent bones are connected by fibrous connective tissue
fibula thin, non-weight-bearing bone found on the lateral side of the leg
fibular collateral ligament extrinsic ligament of the knee joint that spans from the lateral epicondyle of the femur to the head of the fibula; resists hyperextension and rotation of the extended knee
flat bone thin and curved bone; serves as a point of attachment for muscles and protects internal organs
flexion movement in the sagittal plane that decreases the angle of a joint (bends the joint); motion involving anterior bending of the vertebral column
floating ribs vertebral ribs 11–12 that do not attach to the sternum or to the costal cartilage of another rib
fontanelle expanded area of fibrous connective tissue that separates the brain case bones of the skull prior to birth and during the first year after birth
foot portion of the lower limb located distal to the ankle joint
foramen magnum large opening in the occipital bone of the skull through which the spinal cord emerges and the vertebral arteries enter the cranium
fossa (plural = fossae) shallow depression on the surface of a bone
frontal bone unpaired bone that forms forehead, roof of orbit, and floor of anterior cranial fossa
frontal sinus air-filled space within the frontal bone; most anterior of the paranasal sinuses
glenohumeral joint shoulder joint; articulation between the glenoid cavity of the scapula and head of the humerus; multiaxial ball-and-socket joint that allows for flexion/extension, abduction/adduction, circumduction, and medial/ lateral rotation of the humerus glenohumeral ligament capsule one of the three intrinsic ligaments of the shoulder joint that strengthen the anterior articular
glenoid fossa (also, glenoid cavity) shallow depression located on the lateral scapula, between the superior and lateral borders
glenoid labrum lip of fibrocartilage located around the outside margin of the glenoid cavity of the scapula
gomphosis type of fibrous joint in which the root of a tooth is anchored into its bony jaw socket by strong periodontal ligaments
greater sciatic notch large, U-shaped indentation located on the posterior margin of the ilium, superior to the ischial spine
greater trochanter large, bony expansion of the femur that projects superiorly from the base of the femoral neck
greater tubercle situated lateral to the head and lesser tubercle
hallux big toe; digit 1 of the foot
hamate from the lateral side, the fourth of the four distal carpal bones; articulates with the lunate and triquetrum proximally, the fourth and fifth metacarpals distally, and the capitate laterally
hand region of the upper limb distal to the wrist joint
hard palate bony structure that forms the roof of the mouth and floor of the nasal cavity, formed by the palatine process of the maxillary bones and the horizontal plate of the palatine bones
head of the femur rounded, proximal end of the femur that articulates with the acetabulum of the hip bone to form the hip joint
head of the fibula small, knob-like, proximal end of the fibula; articulates with the inferior aspect of the lateral condyle of the tibia
head of the humerus smooth, rounded region on the medial side of the proximal humerus; articulates with the glenoid fossa of the scapula to form the glenohumeral (shoulder) joint
head of the radius disc-shaped structure that forms the proximal end of the radius; articulates with the capitulum of the humerus as part of the elbow joint, and with the radial notch of the ulna as part of the proximal radioulnar joint
head of the rib posterior end of a rib that articulates with the bodies of thoracic vertebrae
head of the ulna small, rounded distal end of the ulna; articulates with the ulnar notch of the distal radius, forming the distal radioulnar joint
hinge joint synovial joint at which the convex surface of one bone articulates with the concave surface of a second bone; includes the elbow, knee, ankle, and interphalangeal joints; functionally classified as a uniaxial joint
hip bone coxal bone; single bone that forms the pelvic girdle; consists of three areas, the ilium, ischium, and pubis
hip joint joint located at the proximal end of the lower limb; formed by the articulation between the acetabulum of the hip bone and the head of the femur
hook of the hamate bone bony extension located on the anterior side of the hamate carpal bone
humeroradial joint articulation between the capitulum of the humerus and head of the radius
humeroulnar joint articulation between the trochlea of humerus and the trochlear notch of the ulna; uniaxial hinge joint that allows for flexion/extension of the forearm
humerus single bone of the upper arm
hyoid bone small, U-shaped bone located in upper neck that does not contact any other bone
hypophyseal (pituitary) fossa shallow depression on top of the sella turcica that houses the pituitary (hypophyseal) gland
iliac crest curved, superior margin of the ilium
ilium superior portion of the hip bone
inferior angle of the scapula inferior corner of the scapula located where the medial and lateral borders meet
inferior articular process bony process that extends downward from the vertebral arch of a vertebra that articulates with the superior articular process of the next lower vertebra
inferior nasal concha one of the paired bones that project from the lateral walls of the nasal cavity to form the largest and most inferior of the nasal conchae
inferior pubic ramus narrow segment of bone that passes inferiorly and laterally from the pubic body; joins with the ischial ramus to form the ischiopubic ramus
intercondylar notch deep depression on the posterior side of the distal femur that separates the medial and lateral condyles
intermediate cuneiform middle of the three cuneiform tarsal bones; articulates posteriorly with the navicular bone, medially with the medial cuneiform bone, laterally with the lateral cuneiform bone, and anteriorly with the second metatarsal bone
interosseous border of the fibula small ridge running down the medial side of the fibular shaft; for attachment of the interosseous membrane between the fibula and tibia
interosseous border of the radius narrow ridge located on the medial side of the radial shaft; for attachment of the interosseous membrane between the ulna and radius bones
interosseous border of the tibia small ridge running down the lateral side of the tibial shaft; for attachment of the interosseous membrane between the tibia and fibula
interosseous border of the ulna narrow ridge located on the lateral side of the ulnar shaft; for attachment of the interosseous membrane between the ulna and radius
interosseous membrane of the antebrachium sheet of dense connective tissue that unites the radius and ulna bones interosseous membrane of the leg bones sheet of dense connective tissue that unites the shafts of the tibia and fibula
interosseous membrane wide sheet of fibrous connective tissue that fills the gap between two parallel bones, forming a syndesmosis; found between the radius and ulna of the forearm and between the tibia and fibula of the leg
interphalangeal joint articulation between adjacent phalanx bones of the hand or foot digits
intertubercular groove/sulcus bicipital groove; narrow groove located between the greater and lesser tubercles of the humerus
intervertebral disc structure located between the bodies of adjacent vertebrae that strongly joins the vertebrae; provides padding, weight bearing ability, and enables vertebral column movements
intervertebral foramen opening located between adjacent vertebrae for exit of a spinal nerve
intracapsular ligament ligament that is located within the articular capsule of a synovial joint
intramembranous ossification process by which bone forms directly from mesenchymal tissue
inversion foot movement involving the intertarsal joints of the foot in which the bottom of the foot is turned toward the midline ischiofemoral ligament aspect of the hip joint intrinsic ligament spanning from the ischium of the hip bone to the femur, on the posterior
irregular bone bone of complex shape; protects internal organs from compressive forces
ischial ramus bony extension projecting anteriorly and superiorly from the ischial tuberosity; joins with the inferior pubic ramus to form the ischiopubic ramus
ischial tuberosity large, roughened protuberance that forms the posteroinferior portion of the hip bone; weight- bearing region of the pelvis when sitting
ischiopubic ramus narrow extension of bone that connects the ischial tuberosity to the pubic body; formed by the junction of the ischial ramus and inferior pubic ramus
ischium posteroinferior portion of the hip bone
joint cavity space enclosed by the articular capsule of a synovial joint that is filled with synovial fluid and contains the articulating surfaces of the adjacent bones
joint site at which two or more bones or bone and cartilage come together (articulate)
jugular (suprasternal) notch shallow notch located on superior surface of sternal manubrium
jugular foramen irregularly shaped opening located in the lateral floor of the posterior cranial cavity
knee joint joint that separates the thigh and leg portions of the lower limb; formed by the articulations between the medial and lateral condyles of the femur, and the medial and lateral condyles of the tibia
lacrimal bone paired bones that contribute to the anterior-medial wall of each orbit
lambdoid suture inverted V-shaped joint that unites the occipital bone to the right and left parietal bones on the posterior skull
lamina portion of the vertebral arch on each vertebra that extends between the transverse and spinous process
lateral (external) rotation movement of the arm at the shoulder joint or the thigh at the hip joint that moves the anterior surface of the limb away from the midline of the body
lateral condyle of the femur smooth, articulating surface that forms the distal and posterior sides of the lateral expansion of the distal femur
lateral condyle of the tibia lateral, expanded region of the proximal tibia that includes the smooth surface that articulates with the lateral condyle of the femur as part of the knee joint
lateral cuneiform most lateral of the three cuneiform tarsal bones; articulates posteriorly with the navicular bone, medially with the intermediate cuneiform bone, laterally with the cuboid bone, and anteriorly with the third metatarsal bone
lateral epicondyle of the humerus small projection located on the lateral side of the distal humerus
lateral flexion bending of the neck or body toward the right or left side
lateral malleolus expanded distal end of the fibula
lateral meniscus C-shaped fibrocartilage articular disc located at the knee, between the lateral condyle of the femur and the lateral condyle of the tibia
lateral tibiofemoral joint portion of the knee consisting of the articulation between the lateral condyle of the tibia and the lateral condyle of the femur; allows for flexion/extension at the knee
leg (crus or crural region) portion of the lower limb located between the knee and ankle joints
lesser trochanter small, bony projection on the medial side of the proximal femur, at the base of the femoral neck
lesser tubercle small, bony prominence located on anterior side of the proximal humerus
ligament strong band of dense connective tissue spanning between bones ligament of the head of the femur of the femur intracapsular ligament that runs from the acetabulum of the hip bone to the head
linea aspera longitudinally running bony ridge located in the middle third of the posterior femur
long bone cylinder-shaped bone that is longer than it is wide; functions as a lever
lumbar curvature posteriorly concave curvature of the lumbar vertebral column region; a secondary curve of the vertebral column
lumbar vertebrae five vertebrae numbered as L1–L5 that are located in lumbar region (lower back) of the vertebral column
lunate from the lateral side, the second of the four proximal carpal bones; articulates with the radius proximally, the capitate and hamate distally, the scaphoid laterally, and the triquetrum medially
mandible unpaired bone that forms the lower jaw bone; the only moveable bone of the skull
manubrium expanded, superior portion of the sternum
mastoid process large bony prominence on the inferior, lateral skull, just behind the earlobe
maxillary bone (also, maxilla) paired bones that form the upper jaw and anterior portion of the hard palate
maxillary sinus air-filled space located with each maxillary bone; largest of the paranasal sinuses
medial (internal) rotation movement of the arm at the shoulder joint or the thigh at the hip joint that brings the anterior surface of the limb toward the midline of the body
medial condyle of the femur smooth, articulating surface that forms the distal and posterior sides of the medial expansion of the distal femur
medial condyle of the tibia medial, expanded region of the proximal tibia that includes the smooth surface that articulates with the medial condyle of the femur as part of the knee joint
medial cuneiform most medial of the three cuneiform tarsal bones; articulates posteriorly with the navicular bone, laterally with the intermediate cuneiform bone, and anteriorly with the first and second metatarsal bones
medial epicondyle of the femur roughened area of the distal femur located on the medial side of the medial condyle
medial epicondyle of the humerus enlarged projection located on the medial side of the distal humerus
medial malleolus bony expansion located on the medial side of the distal tibia
medial meniscus C-shaped fibrocartilage articular disc located at the knee, between the medial condyle of the femur and medial condyle of the tibia
medial tibiofemoral joint portion of the knee consisting of the articulation between the medial condyle of the tibia and the medial condyle of the femur; allows for flexion/extension at the knee
median sacral crest irregular ridge running down the midline of the posterior sacrum that was formed from the fusion of the spinous processes of the five sacral vertebrae
medullary cavity hollow region of the diaphysis; filled with yellow marrow
meniscus articular disc
metacarpal bone one of the five long bones that form the palm of the hand; numbered 1–5, starting on the lateral (thumb) side of the hand
metacarpophalangeal joint articulation between the distal end of a metacarpal bone of the hand and a proximal phalanx bone of the thumb or a finger
metatarsal bone one of the five elongated bones that forms the anterior half of the foot; numbered 1–5, starting on the medial side of the foot
metatarsophalangeal joint articulation between a metatarsal bone of the foot and the proximal phalanx bone of a toe
middle cranial fossa centrally located cranial fossa that extends from the lesser wings of the sphenoid bone to the petrous ridge
middle nasal concha nasal concha formed by the ethmoid bone that is located between the superior and inferior conchae
modelling process, during bone growth, by which bone is resorbed on one surface of a bone and deposited on another
multiaxial joint type of diarthrosis; a joint that allows for movements within three planes (three axes)
nasal bone paired bones that form the base of the nose
nasal cavity opening through skull for passage of air
nasal conchae curved bony plates that project from the lateral walls of the nasal cavity; include the superior and middle nasal conchae, which are parts of the ethmoid bone, and the independent inferior nasal conchae bone
nasal septum flat, midline structure that divides the nasal cavity into halves, formed by the perpendicular plate of the ethmoid bone, vomer bone, and septal cartilage
nasolacrimal canal passage for drainage of tears that extends downward from the medial-anterior orbit to the nasal cavity, terminating behind the inferior nasal conchae
navicular tarsal bone that articulates posteriorly with the talus bone, laterally with the cuboid bone, and anteriorly with the medial, intermediate, and lateral cuneiform bones
nucleus pulposus gel-like central region of an intervertebral disc; provides for padding, weight-bearing, and movement between adjacent vertebrae
nutrient foramen small opening in the middle of the external surface of the diaphysis, through which an artery enters the bone to provide nourishment
obturator foramen large opening located in the anterior hip bone, between the pubis and ischium regions
occipital bone unpaired bone that forms the posterior portions of the brain case and base of the skull
occipital condyle paired, oval-shaped bony knobs located on the inferior skull, to either side of the foramen magnum
olecranal fossa large depression located on the posterior side of the distal humerus; this space receives the olecranon process of the ulna when the elbow is fully extended
olecranon expanded posterior and superior portions of the proximal ulna; forms the bony tip of the elbow
optic canal opening spanning between middle cranial fossa and posterior orbit
orbit bony socket that contains the eyeball and associated muscles
ossification (also, osteogenesis) bone formation
ossification centre cluster of osteoblasts found in the early stages of intramembranous ossification
palatine bone paired bones that form the posterior quarter of the hard palate and a small area in floor of the orbit
paranasal sinuses cavities within the skull that are connected to the conchae that serve to warm and humidify incoming air, produce mucus, and lighten the weight of the skull; consist of frontal, maxillary, sphenoidal, and ethmoidal sinuses
parietal bone paired bones that form the upper, lateral sides of the skull
patella kneecap; the largest sesamoid bone of the body; articulates with the distal femur
patellar ligament ligament spanning from the patella to the anterior tibia; serves as the final attachment for the quadriceps femoris muscle
patellar surface smooth groove located on the anterior side of the distal femur, between the medial and lateral condyles; site of articulation for the patella
pectoral girdle shoulder girdle; the set of bones, consisting of the scapula and clavicle, which attaches each upper limb to the axial skeleton
pedicle portion of the vertebral arch that extends from the vertebral body to the transverse process perpendicular plate of the ethmoid bone superior portion of the nasal septum downward, midline extension of the ethmoid bone that forms the
pelvic girdle hip girdle; consists of a single hip bone, which attaches a lower limb to the sacrum of the axial skeleton
pelvis ring of bone consisting of the right and left hip bones, the sacrum, and the coccyx
periodontal ligament band of dense connective tissue that anchors the root of a tooth into the bony jaw socket
periosteum fibrous membrane covering the outer surface of bone and continuous with ligaments primary ossification center endochondral ossification region, deep in the periosteal collar, where bone development starts during
phalanx bone of the foot (plural = phalanges) one of the 14 bones that form the toes; these include the proximal and distal phalanges of the big toe, and the proximal, middle, and distal phalanx bones of toes two through five
phalanx bone of the hand (plural = phalanges) one of the 14 bones that form the thumb and fingers; these include the proximal and distal phalanges of the thumb, and the proximal, middle, and distal phalanx bones of the fingers two through five
pisiform from the lateral side, the fourth of the four proximal carpal bones; articulates with the anterior surface of the triquetrum
pivot joint synovial joint at which the rounded portion of a bone rotates within a ring formed by a ligament and an articulating bone; functionally classified as uniaxial joint
plane joint synovial joint formed between the flattened articulating surfaces of adjacent bones; functionally classified as a multiaxial joint
plantar flexion foot movement at the ankle in which the heel is lifted off of the ground
pollex (also, thumb) digit 1 of the hand posterior inferior iliac spine posterior ilium posterior sacroiliac ligament small, bony projection located at the inferior margin of the auricular surface on the strong ligament spanning the sacrum and ilium of the hip bone that supports the posterior side of the sacroiliac joint
posterior (dorsal) sacral foramen one of the series of paired openings located on the posterior (dorsal) side of the sacrum
posterior arch posterior portion of the ring-like C1 (atlas) vertebra
posterior cranial fossa deepest and most posterior cranial fossa; extends from the petrous ridge to the occipital bone posterior longitudinal ligament the vertebral bodies ligament that runs the length of the vertebral column, uniting the posterior sides of
posterior cruciate ligament intracapsular ligament of the knee; extends from the posterior, superior surface of the tibia to the inner aspect of the medial condyle of the femur; prevents anterior displacement of the femur when the knee is flexed and weight bearing
primary curvature anteriorly concave curvatures of the thoracic and sacrococcygeal regions that are retained from the original fetal curvature of the vertebral column
projection bone markings where part of the surface sticks out above the rest of the surface, where tendons and ligaments attach
pronated position forearm position in which the palm faces backward
pronation forearm motion that moves the palm of the hand from the palm forward to the palm backward position
proximal radioulnar joint articulation between head of radius and radial notch of ulna; uniaxial pivot joint that allows for rotation of radius during pronation/supination of forearm
proximal tibiofibular joint articulation between the head of the fibula and the inferior aspect of the lateral condyle of the tibia
pubic body enlarged, medial portion of the pubis region of the hip bone
pubic symphysis joint formed by the articulation between the pubic bodies of the right and left hip bones
pubis anterior portion of the hip bone
radial notch of the ulna small, smooth area on the lateral side of the proximal ulna; articulates with the head of the radius as part of the proximal radioulnar joint
radial tuberosity oval-shaped, roughened protuberance located on the medial side of the proximal radius
radiocarpal joint wrist joint, located between the forearm and hand regions of the upper limb; articulation formed proximally by the distal end of the radius and the fibrocartilaginous pad that unites the distal radius and ulna bone, and distally by the scaphoid, lunate, and triquetrum carpal bones
radius bone located on the lateral side of the forearm
red bone marrow connective tissue in the interior cavity of a bone where hematopoiesis takes place
remodelling process by which osteoclasts resorb old or damaged bone at the same time as and on the same surface where osteoblasts form new bone to replace that which is resorbed
ribs thin, curved bones of the chest wall
rotation movement of a bone around a central axis (atlantoaxial joint) or around its long axis (proximal radioulnar joint; shoulder or hip joint); twisting of the vertebral column resulting from the summation of small motions between adjacent vertebrae
sacral canal bony tunnel that runs through the sacrum
sacral foramina series of paired openings for nerve exit located on both the anterior (ventral) and posterior (dorsal) aspects of the sacrum
sacrococcygeal curvature anteriorly concave curvature formed by the sacrum and coccyx; a primary curve of the vertebral column
sacroiliac joint joint formed by the articulation between the auricular surfaces of the sacrum and ilium
sacrum single bone located near the inferior end of the adult vertebral column that is formed by the fusion of five sacral vertebrae; forms the posterior portion of the pelvis
saddle joint synovial joint in which the articulating ends of both bones are convex and concave in shape, such as at the first carpometacarpal joint at the base of the thumb; functionally classified as a biaxial joint
sagittal suture joint that unites the right and left parietal bones at the midline along the top of the skull
scaphoid from the lateral side, the first of the four proximal carpal bones; articulates with the radius proximally, the trapezoid, trapezium, and capitate distally, and the lunate medially
scapula shoulder blade bone located on the posterior side of the shoulder
secondary curvature posteriorly concave curvatures of the cervical and lumbar regions of the vertebral column that develop after the time of birth
secondary ossification centre region of bone development in the epiphyses
sella turcica elevated area of sphenoid bone located at midline of the middle cranial fossa
septal cartilage flat cartilage structure that forms the anterior portion of the nasal septum
sesamoid bone small, round bone embedded in a tendon; protects the tendon from compressive forces
shaft of the femur cylindrically shaped region that forms the central portion of the femur
shaft of the fibula elongated, slender portion located between the expanded ends of the fibula
shaft of the humerus narrow, elongated, central region of the humerus
shaft of the radius narrow, elongated, central region of the radius
shaft of the tibia triangular-shaped, central portion of the tibia
shaft of the ulna narrow, elongated, central region of the ulna
short bone cube-shaped bone that is approximately equal in length, width, and thickness; provides limited motion
skeletal system organ system composed of bones and cartilage that provides for movement, support, and protection
skeleton bones of the body
skull bony structure that forms the head, face, and jaws, and protects the brain; consists of 22 bones
sphenoid bone unpaired bone that forms the central base of skull
sphenoidal sinus air-filled space located within the sphenoid bone; most posterior of the paranasal sinuses
spine of the scapula prominent ridge passing mediolaterally across the upper portion of the posterior scapular surface
spinous process unpaired bony process that extends posteriorly from the vertebral arch of a vertebra
squamousal suture joint that unites the parietal bone to the squamous portion of the temporal bone on the lateral side of the skull
sternal angle junction line between manubrium and body of the sternum and the site for attachment of the second rib to the sternum
sternal end of the clavicle medial end of the clavicle that articulates with the manubrium of the sternum
sternoclavicular joint articulation between the manubrium of the sternum and the sternal end of the clavicle; forms the only bony attachment between the pectoral girdle of the upper limb and the axial skeleton
sternum flattened bone located at the center of the anterior chest
superior articular process bony process that extends upward from the vertebral arch of a vertebra that articulates with the inferior articular process of the next higher vertebra
superior nasal concha smallest and most superiorly located of the nasal conchae; formed by the ethmoid bone
superior orbital fissure irregularly shaped opening between the middle cranial fossa and the posterior orbit
superior pubic ramus narrow segment of bone that passes laterally from the pubic body to join the ilium
supinated position forearm position in which the palm faces anteriorly (anatomical position)
supination forearm motion that moves the palm of the hand from the palm backward to the palm forward position
suture fibrous joint that connects the bones of the skull (except the mandible); an immobile joint (synarthrosis)
symphysis type of cartilaginous joint where the bones are joined by fibrocartilage
synarthrosis immobile or nearly immobile joint
synchondrosis type of cartilaginous joint where the bones are joined by hyaline cartilage
syndesmosis type of fibrous joint in which two separated, parallel bones are connected by an interosseous membrane
synostosis site at which adjacent bones or bony components have fused together
synovial fluid thick, lubricating fluid that fills the interior of a synovial joint
synovial joint joint at which the articulating surfaces of the bones are located within a joint cavity formed by an articular capsule
synovial membrane thin layer that lines the inner surface of the joint cavity at a synovial joint; produces the synovial fluid
talocrural joint ankle joint; articulation between the talus bone of the foot and medial malleolus of the tibia, distal tibia, and lateral malleolus of the fibula; a uniaxial hinge joint that allows only for dorsiflexion and plantar flexion of the foot
talus tarsal bone that articulates superiorly with the tibia and fibula at the ankle joint; also articulates inferiorly with the calcaneus bone and anteriorly with the navicular bone
tarsal bone one of the seven bones that make up the posterior foot; includes the calcaneus, talus, navicular, cuboid, medial cuneiform, intermediate cuneiform, and lateral cuneiform bones
temporal bone paired bones that form the lateral, inferior portions of the skull, with squamous, mastoid, and petrous portions
thigh (femoral region) portion of the lower limb located between the hip and knee joints
thoracic cage consists of 12 pairs of ribs and sternum
thoracic curvature anteriorly concave curvature of the thoracic vertebral column region; a primary curve of the vertebral column
thoracic vertebrae twelve vertebrae numbered as T1–T12 that are located in the thoracic region (upper back) of the vertebral column
tibia shin bone; the large, weight-bearing bone located on the medial side of the leg
tibial collateral ligament extrinsic ligament of knee joint that spans from the medial epicondyle of the femur to the medial tibia; resists hyperextension and rotation of extended knee
tibial tuberosity elevated area on the anterior surface of the proximal tibia
transverse foramen opening found only in the transverse processes of cervical vertebrae
transverse process paired bony processes that extends laterally from the vertebral arch of a vertebra
trapezium from the lateral side, the first of the four distal carpal bones; articulates with the scaphoid proximally, the first and second metacarpals distally, and the trapezoid medially
trapezoid from the lateral side, the second of the four distal carpal bones; articulates with the scaphoid proximally, the second metacarpal distally, the trapezium laterally, and the capitate medially
triquetrum from the lateral side, the third of the four proximal carpal bones; articulates with the lunate laterally, the hamate distally, and has a facet for the pisiform
trochlea pulley-shaped region located medially at the distal end of the humerus; articulates at the elbow with the trochlear notch of the ulna
trochlear notch large, C-shaped depression located on the anterior side of the proximal ulna; articulates at the elbow with the trochlea of the humerus
true ribs vertebrosternal ribs 1–7 that attach via their costal cartilage directly to the sternum
tubercle of the rib small bump on the posterior side of a rib for articulation with the transverse process of a thoracic vertebra
ulna bone located on the medial side of the antebrachium
uniaxial joint type of diarthrosis; joint that allows for motion within only one plane (one axis)
vertebra individual bone in the neck and back regions of the vertebral column
vertebral (spinal) canal bony passageway within the vertebral column for the spinal cord that is formed by the series of individual vertebral foramina
vertebral arch bony arch formed by the posterior portion of each vertebra that surrounds and protects the spinal cord
vertebral column entire sequence of bones that extend from the skull to the tailbone
vertebral foramen opening associated with each vertebra defined by the vertebral arch that provides passage for the spinal cord
vomer bone unpaired bone that forms the inferior and posterior portions of the nasal septum
xiphoid process small process that forms the inferior tip of the sternum
yellow bone marrow connective tissue in the interior cavity of a bone where fat is stored
zygoapophyseal joints facet joints; plane joints between the superior and inferior articular processes of adjacent vertebrae that provide for only limited motion between the vertebrae
zygomatic arch elongated, free-standing arch on the lateral skull, formed anteriorly by the temporal process of the zygomatic bone and posteriorly by the zygomatic process of the temporal bone
zygomatic bone cheekbone; paired bones that contribute to the lateral orbit and anterior zygomatic arch

