Chapter 6: CONNECTIVE TISSUE
Introduction
Chapter Objectives
After studying this chapter, you will be able to:
- Identify and describe the general organisation of the cells and intercellular substances of connective tissue
- Classify connective tissue subtypes
- Examine the macroscopic and microscopic appearance of a range of connective tissue types
Connective tissue is the most widely distributed primary tissue in the human body. As may be obvious from its name, one of the major functions of connective tissue is to support and connect tissues and organs. Unlike epithelial tissue, which is composed of cells closely packed with little or no extracellular space in-between, connective tissue cells are dispersed in a matrix. The matrix usually includes a large amount of extracellular material produced by the connective tissue cells that are embedded within it. The matrix plays a major role in the functioning of this tissue. The major component of the matrix is a ground substance often crisscrossed by fibres. This ground substance is usually a fluid, but it can also be mineralised and solid, as in bones. Connective tissues come in a vast variety of forms, yet they typically have in common three characteristic components: cells, large amounts of amorphous ground substance, and fibres. The amount and structure of each component correlates with the function of the tissue, from the rigid ground substance in bones supporting the body to the housing of specialised cells, for example, a phagocytic cell that engulfs pathogens and also rids tissue of cellular debris.
General Features of Connective Tissues
Learning Objectives
By the end of this section, you will be able to:
- Describe the types of connective tissue: proper, supportive, and fluid
- Identify and describe the major cell types found in connective tissue proper
- Describe the intercellular substances in connective tissues including fibres and amorphous ground substance
Connective tissues are characterised by their abundance of intercellular material and relatively few cells. The intercellular material or matrix consists of a range of connective tissue fibres and amorphous ground substances. The three broad categories of connective tissue are classified according to the characteristics of their ground substance and the types of fibres found within the matrix (Table 4.1). Connective tissue proper (or general connective tissue) includes loose connective tissue and dense connective tissue. Both tissues have a variety of cell types and protein fibres suspended in a viscous ground substance. Dense connective tissue is reinforced by bundles of fibres that provide tensile strength, elasticity and protection. In loose connective tissue, the fibres are loosely organised, leaving large spaces in between.
Supportive connective tissue—bone and cartilage—provide structure and strength to the body and protect soft tissues. A few distinct cell types and densely packed fibres in a matrix characterise these tissues. In bone, the matrix is rigid and described as calcified because of the deposited calcium salts. In fluid connective tissue, in other words, lymph and blood, various specialised cells circulate in a watery fluid containing salts, nutrients, and dissolved proteins. Supportive and fluid connective tissues are collectively referred to as specialised connective tissues.
Table 4.1 Connective Tissue Examples
| Connective tissue proper | Supportive connective tissue | Fluid connective tissue |
|---|---|---|
Loose connective tissue
|
Cartilage
|
Blood |
Dense connective tissue
|
Bones
|
Lymph |
Cell Types
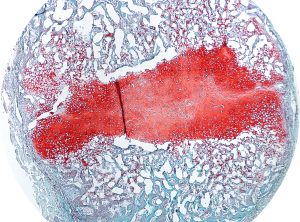
Fibroblasts and adipocytes cells are fixed cells, which means they remain within the connective tissue. Other cells (migratory or wandering cells) move in and out of the connective tissue in response to chemical signals. Macrophages, leucocytes and phagocytic cells are found in connective tissue proper but are actually part of the immune system protecting the body (Figure 4.9). The most abundant cell present in all subtypes of connective tissue proper is the fibroblast. Fibroblasts are spindle-shaped with moderate amounts of cytoplasm and a large oval nucleus when active. In their inactive or resting form, fibroblasts have reduced cytoplasm and small, flattened and elongated nuclei. Polysaccharides and proteins secreted by fibroblasts combine with extra-cellular fluids to produce a viscous ground substance that, with embedded fibrous proteins, forms the extra-cellular matrix.
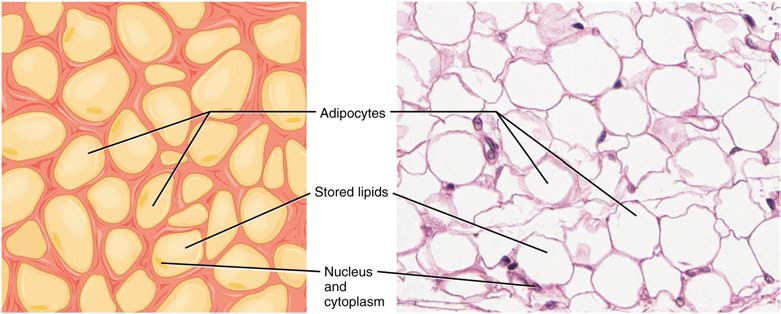
Adipocytes are cells that store lipids as droplets that fill most of the cytoplasm. The number and type of adipocytes depends on the tissue and location, and vary among individuals in the population. Adipocytes can be recognised by the large lipid droplet that occupies the majority of the cell and pushes the nucleus to the periphery of the cell in an eccentric and flattened position. They appear as large white circular cells in stained sections (Figure 4.9).
The macrophage is a large cell derived from a monocyte, a type of leukocyte found in the blood, which enters the connective tissue matrix from the blood vessels. Roaming, or free, macrophages move rapidly through the intercellular matrix, engulfing infectious agents and cellular debris. Connective tissues also house fixed macrophages that are permanent residents of their tissues. The appearance of macrophages is highly variable due to the range of subtypes and depending on its funcitonal state (active or resting). Similar to macrophages, wandering leucocytes such as lymphocytes can also enter connective tissue proper to perform lymphatic functions including phagocytosis, allergic or inflammatory reactions and immune defence. Lymphocytes can be recognised by their large round nucleus that occupies almost all of the cytoplasm of the cell.
Mesenchymal stem cells are also commonly found in connective tissues where they can differentiate into a range of mature cell types such as adipocytes, fibroblasts and specialised connective tissue cells including bone and cartilaginous cells.
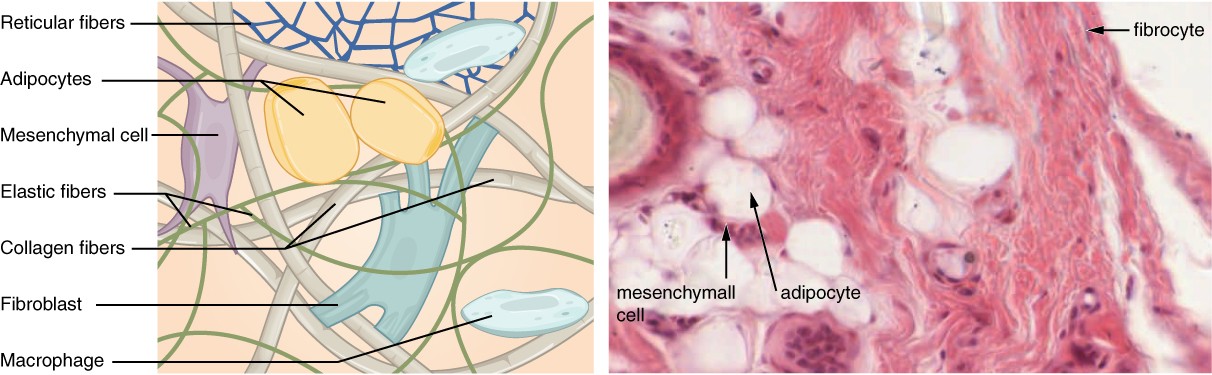
Figure 4.9 Connective Tissue Proper Fibroblasts produce the extracellular matrix of this connective tissue. Connective tissue proper includes the fixed cells fibrocytes, adipocytes, and mesenchymal cells. Migratory cells such as macrophages can enter connective tissues when needed. LM × 400. [Micrograph provided by the Regents of University of Michigan Medical School © 2012]
Connective Tissue Fibres and Ground Substance
Intercellular substances are the predominant components of most types of connective tissue (adipose tissue being the exception). There are two types of intercellular substances, amorphous ground substances and fibres. Three main types of fibres are secreted by fibroblasts: collagenous fibres, reticular fibres and elastic fibres.
All of these fibre types and connective tissue cells are embedded in amorphous ground substance. Secreted by fibroblasts, ground substance is made of carbohydrates and proteins. Amorphous ground substance appears as clear spaces between the fibres and cells of a connective tissue in typical histological preparations as they usually dissolve out of the tissue section during preparation.
Connective Tissue Proper
Learning Objectives
By the end of this section, you will be able to:
- Identify and describe the microscopic features of loose and dense connective tissue subtypes: areolar, adipose, reticular, dense regular and dense irregular connective tissue
- Describe common locations for each of the connective tissue proper subtypes
Connective tissue proper or general connective tissues can be classified into two major types based on the density of connective tissue fibres. A connective tissue that is characterised microscopically by a relative abundance of cells and ground substance and a loose arrangement of fibres is referred to as loose connective tissue. Dense connective tissues are distinguished microscopically by the close packing of their fibres and relatively few cells and little ground substance.
Loose Connective Tissue
Loose connective tissue is found between many organs where it acts both to absorb shock and bind tissues together. It allows water, salts and various nutrients to diffuse through to adjacent or embedded cells and tissues. There are three types of loose connective tissue: areolar adipose and reticular connective tissue.
Areolar tissue is the most common form of loose connective tissue and shows little specialisation. It contains all the cell types and fibres previously described and is distributed in a random, web-like fashion. It occupies the superficial fascia (hypodermis of skin), fills the spaces between muscle fibres, surrounds blood and lymph vessels, and supports organs in the abdominal cavity. Areolar tissue underlies most epithelia and represents the connective tissue component of epithelial membranes.
INTERACTIVE ACTIVITY
Adipose tissue consists mostly of adipocytes, with little extracellular matrix (Figure 4.10). A large number of capillaries are also present to allow rapid storage and mobilisation of lipid molecules.
Figure 4.10 Adipose Tissue This is a loose connective tissue that consists of fat cells with little extracellular matrix. It stores fat for energy and provides insulation. LM × 800. [Micrograph provided by the Regents of University of Michigan Medical School © 2012]
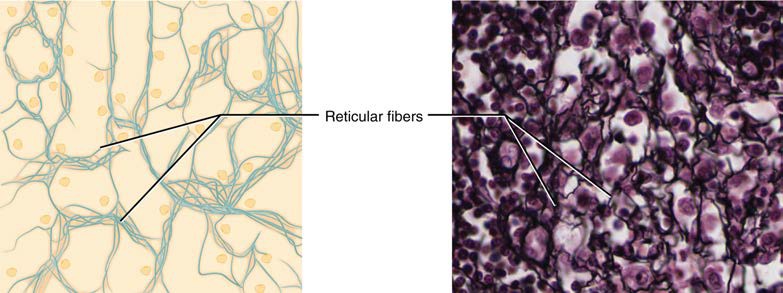
Reticular tissue is a mesh-like, supportive framework for soft organs such as lymphatic tissue, the spleen and the liver (Figure 4.11). Fibroblasts produce the reticular fibres that form the network onto which other cells attach. It derives its name from the Latin reticulus, which means “little net.”
Figure 4.11 Reticular Tissue This is a loose connective tissue made up of a network of reticular fibres that provides a supportive framework for soft organs. Note the black staining of the densely branching reticular fibres. LM × 1600. [Micrograph provided by the Regents of University of Michigan Medical School © 2012]
Dense Connective Tissue
Dense connective tissue contains more collagenous fibres than does loose connective tissue. As a consequence, it displays greater resistance to stretching. There are two major categories of dense connective tissue: regular and irregular. Dense regular connective tissue fibres are parallel to each other, enhancing tensile strength and resistance to stretching in the direction of the fibre orientation. Ligaments and tendons are made of dense regular connective tissue, but in ligaments not all fibres are parallel. Whilst collagenous fibres are the most abundant fibre type in structures composed of dense regular connective tissue, elastic fibres are also found in some examples and in different proportions. For example ligaments have a relatively higher proportion of elastic fibres than is seen in tendons, bestowing different physical properties to each of these structures. In photomicrographs the collagenous fibres appear wavy due to the natural protein arrangement of collagen. This ‘crimping’ straightens out with the tissue is placed under tension.
In dense irregular connective tissue, the direction of fibres is random. This arrangement gives the tissue greater strength in all directions and less strength in one particular direction. In some tissues, fibres crisscross and form a mesh. In other tissues, stretching in several directions is achieved by alternating layers where fibres run in the same orientation in each layer, and it is the layers themselves that are stacked at an angle. The dermis of the skin, fibrous capsules of some organs, the periosteum and endosteum and deep fascia are examples of dense irregular connective tissue rich in collagenous fibres (Figure 4.12). Note the appearance of the bundles of collagenous fibres in dense irregular connective tissue in photomicrographs are cut in cross-section as well as running longitudinally due to the irregular organisation of fibres.
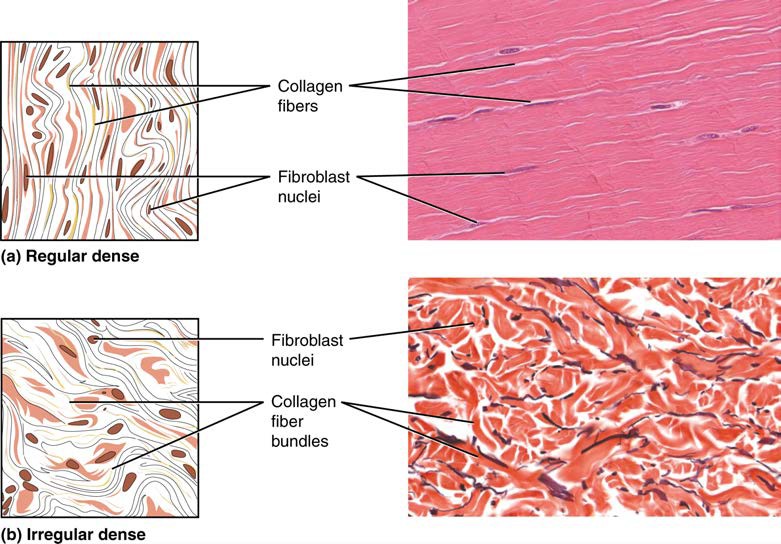
Figure 4.12 Dense Connective Tissue (a) Dense regular connective tissue consists of collagenous fibres packed into parallel bundles. (b) Dense irregular connective tissue consists of collagenous fibres interwoven into a mesh-like network. From top, LM × 1000, LM × 200. [Micrographs provided by the Regents of University of Michigan Medical School © 2012]
Specialised Connective Tissues
Learning Objectives
By the end of this section, you will be able to:
- Identify and describe the microscopic features of cartilaginous tissue subtypes: hyaline, elastic and fibrous cartilaginous tissue
- Identify and describe the microscopic features of bone tissue subtypes: cortical and trabecular bone tissue
- Describe common locations for each of the specialised connective tissue subtypes
Specialised connective tissues include supportive and fluid connective tissues. Two major forms of supportive connective tissue, cartilage and bone, allow the body to maintain its posture and protect internal organs.
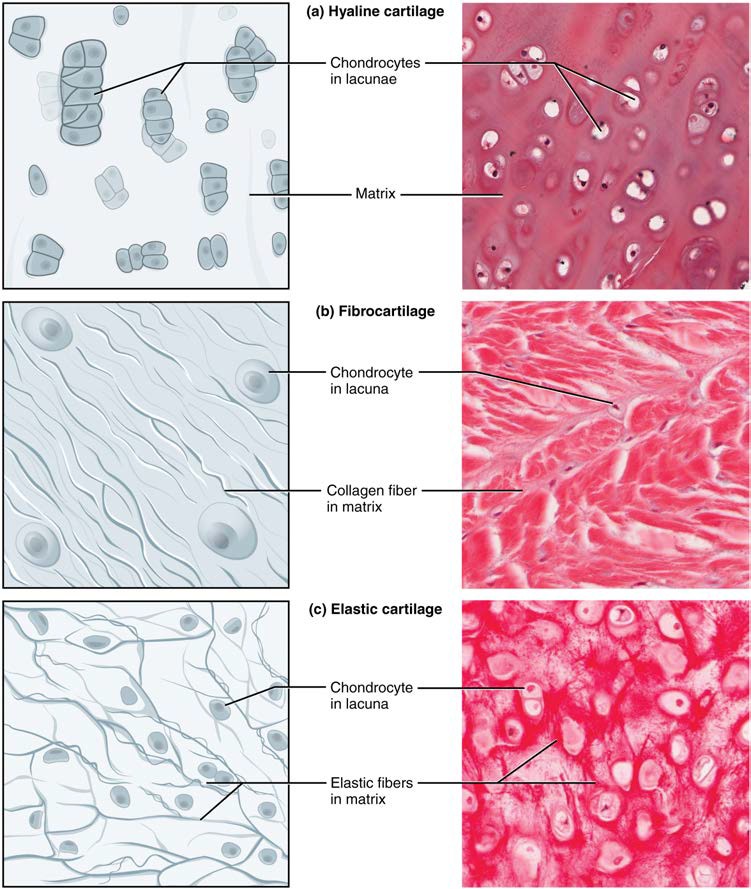
Cartilaginous Tissue
The distinctive appearance of cartilaginous tissue is due to carbohydrates, which bind with ground substance proteins. Embedded within the cartilage matrix are chondrocytes, or cartilage cells, and the space they occupy in the semisolid matrix are called lacunae (singular = lacuna). Cartilaginous tissue is avascular, thus all nutrients need to diffuse through the matrix to reach the chondrocytes. This is a factor contributing to the very slow healing of cartilaginous tissues. The three main types of cartilaginous tissue are hyaline cartilage, fibrocartilage, and elastic cartilage (Figure 4.13).
Figure 4.13 Types of Cartilaginous tissue Cartilaginous tissue is a supportive connective tissue consisting of collagenous fibres embedded in a firm matrix of chondroitin sulfates. (a) Hyaline cartilaginous tissue provides support with some flexibility. Fibres are difficult to visualise in typical stained sections as they are so small. (b) Fibrocartilage provides some compressibility and can absorb pressure. (c) Elastic cartilage provides firm but elastic support. Note the chondrocytes in lacunae in all cartilaginous tissue subtypes. From top, LM × 300, LM × 1200, LM × 1016. [Micrographs provided by the Regents of University of Michigan Medical School © 2012]
Bone Tissue
Bone tissue is a highly vascular mineralised form of connective tissue. It is the only connective tissue subtype with a biphasic composition have an organic phase (fibres, amorphous ground substance and cells) making up on third of bone tissue and an inorganic phase (minerals) making up the remaining two thirds of bone tissue. It provides protection to internal organs and supports the body. Bone tissue also as important functions in calcium homeostasis and acts as a primary location for blood cell production (haematopoesis) within the bone marrow compartment. Bone’s rigid extracellular matrix contains mostly collagenous fibres embedded in a mineralised ground substance. The combination of having both organic and inorganic phases makes bone hard and flexible at the same time. Without the organic phase, bones would be brittle and shatter easily. Without mineral crystals, bones would flex and provide little support. Unlike cartilage, bone tissue can recover from injuries in a relatively short time due to its highly vascular composition.
Bone contains a relatively small number of cells entrenched in a matrix of collagenous fibres that provide a surface for inorganic salt crystals to adhere. These salt crystals form when calcium phosphate and calcium carbonate combine to create hydroxyapatite, which incorporates other inorganic salts like magnesium hydroxide, fluoride, and sulfate as it crystallises, or calcifies, on the collagenous fibers.
Bone Cells
Although bone cells compose a small amount of the bone volume, they are crucial to the function of bones. Four types of cells are found within bone tissue: osteoblasts, osteocytes, osteogenic cells, and osteoclasts (Figure 6.11).
The osteoblast is the bone cell responsible for forming new bone tissue and is found on bone surfaces within the periosteum and endosteum (dense irregular connective tissue membranes that line bone surfaces). Osteoblasts are cuboidal-shaped cells, do not divide, and are responsible for the synthesis and secretion of the collagenous matrix (or osteoid). As the secreted matrix surrounding the osteoblast calcifies, the osteoblast becomes trapped within it; as a result, it changes in structure and becomes an osteocyte, the primary cell of mature bone and the most common type of bone cell. Each osteocyte has a round body with multiple cytoplasmic processes that radiate out from the body. They are located in a space called a lacuna (plural = lacunae) and are surrounded by bone tissue. Osteocytes have an important role in survellance of the bone tissue to maintain bone strength including stimulating bone repair at sites of bone weakness or damage, and detecting mechanical signals from the external environment in response to exercise. In this way, osteocytes have an essential role in maintaining the strength of bone tissue and dynamically adapting to the loads placed on our bodies. Like osteoblasts, osteocytes lack mitotic activity. They can communicate with each other and receive nutrients via their long cytoplasmic processes that extend through canaliculi (singular = canaliculus), channels within the bone matrix.
If osteoblasts and osteocytes are incapable of mitosis, then how are they replenished when old ones die? The answer lies in the properties of a third category of bone cells—the osteogenic cell. These osteogenic cells are undifferentiated with high mitotic activity and they are the only bone cells that divide. Immature osteogenic cells are found in the deep layers of the periosteum and the bone marrow. They have the ability to differentiate and develop into osteoblasts.
The dynamic nature of bone means that new tissue is constantly formed, and old, injured, or unnecessary bone is dissolved for repair or for calcium release. The cell responsible for bone resorption, or breakdown, is the osteoclast. Osteoclasts are found on bone surfaces, are multinucleated, and originate from the function of multiple monocytes and not from osteogenic cells. Osteoclasts are continually breaking down old bone while osteoblasts are continually forming new bone. The process is known as bone remodelling. The ongoing balance between osteoblasts and osteoclasts is responsible for continuous release of calcium into the bloodstream to maintain calcium homeostasis, as well as to repair areas of bone damage and adapt to changes in the mechanical environment. Table 6.3 reviews the bone cells, their functions and locations.
| Cell type | Function | Location |
|---|---|---|
| Osteogenic cells | Develop into osteoblasts | Deep layers of the periosteum and the marrow |
| Osteoblasts | Bone formation | Growing portions of bone, including periosteum and endosteum |
| Osteocytes | Maintain bone strength | Entrapped in matrix in lacunae |
| Osteoclasts | Bone resorption | Bone surfaces and at sites of old, injured, or unneeded bone |
INTERACTIVE ACTIVITY
Photomicrograph of Bone Tissue (Haemotoxylin and Eosin stain; x200 magnification). Learn to accurately identify the three active bone cell types by clicking on each information hotspot in this histological section of trabecular bone tissue. [www.BEST.edu.au]
Questions:
(a) Why do osteoclasts have multiple nuclei?
Bone Tissue Subtypes
Bones contain two types of bone tissue. Trabecular bone looks like a sponge under the microscope and contains empty spaces between trabeculae, or ‘little beams’ of bone tissue. It is lighter than cortical bone and found in the interior of some bones and at the end of long bones. Cortical bone is solid and has greater structural strength. The differences between cortical and trabecular bone are best explored via their histology. Most bones contain a combination of cortical and trabecular bone tissue, but their distribution and concentration vary based on the bone’s overall function. Cortical bone is dense so that it can withstand compressive forces, while trabecular bone has open spaces and supports loading from multiple directions.
Cortical Bone Tissue
Cortical bone, also known as compact or dense bone, is the denser, stronger of the two types of bone tissue (Figure 6.12). It can be found forming the outer shell (cortex) of all bone organs and contains no macroscopic cavities. A higher proportion of cortical bone tissue can be observed in the diaphyses (shaft) of long bones, where it provides support and protection. The microscopic structural unit of cortical bone is called an osteon, or Haversian system. Each osteon is composed of concentric rings of calcified matrix called lamellae (singular = lamella). Running down the centre of each osteon is the central canal, or Haversian canal, which contains blood vessels, nerves and lymphatic vessels. These vessels and nerves branch off at right angles through a perforating canal, also known as Volkmann’s canals, to extend deeper within the cortical bone to connect the periosteum to the endosteum.
The osteocytes are located inside spaces called lacunae (singular = lacuna), found at the borders of adjacent lamellae. As described earlier, canaliculi connect lacunae and eventually with the central canal. This system allows nutrients to be transported to the osteocytes and wastes to be removed from them, as well as allowing the cytoplasmic processes of adjacent osteocytes to communicate with each other.
Figure 6.12 Diagram of Cortical Bone Tissue (a) This cross-sectional view of compact bone shows the basic structural unit, the osteon. (b) In this micrograph of the osteon, you can clearly see the concentric lamellae and central canals. LM × 40. [Micrograph provided by the Regents of University of Michigan Medical School © 2012]
INTERACTIVE ACTIVITY
INTERACTIVE ACTIVITY
INTERACTIVE ACTIVITY
Photomicrograph of Cortical Bone Tissue (Ground human bone, unstained; x200 magnification). Learn to accurately identify the main features of cortical bone tissue by clicking on each information hotspot. [Berkshire Community College Bioscience Image Library]
Questions:
(a) What is the purpose of lacunae and canaliculi?
(b) What is the structural unit of cortical bone tissue called?
Trabecular Bone Tissue
Like cortical bone, trabecular bone, also known as spongy or cancellous bone, contains osteocytes housed in lacunae, but they are not arranged in concentric circles. Instead, the lacunae and osteocytes are found in a lattice-like network of beams called trabeculae (singular = trabecula) (Figure 6.13). The trabeculae may appear to be a random network, but each trabecula forms along lines of stress to provide strength to the bone. The spaces of the trabeculated network provide balance to the dense and heavy cortical bone tissue by making bones lighter so that muscles can move them more easily. In addition, the spaces in some trabecular bone tissue contain red bone marrow, where haematopoiesis occurs. A higher proportion of trabecular bone tissue is located in the ends of long bones (epiphyses and metaphyses) than cortical bone tissue, where the structural arrangement of trabecular bone tissue supports the multiple directions of loading experienced at the joint sites.
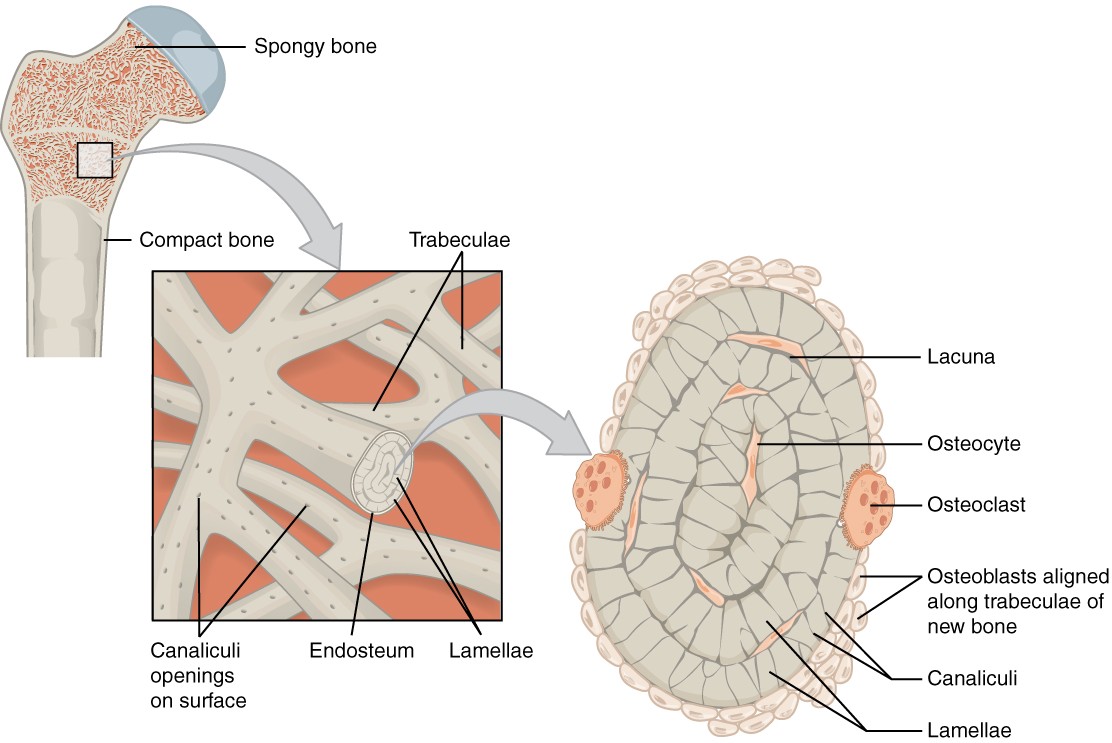
Figure 6.13 Diagram of Trabecular Bone Tissue Trabecular bone is composed of trabeculae that contain osteocytes in lacunae. Red bone marrow fills the spaces in some bones.
INTERACTIVE ACTIVITY
Photomicrograph of Trabecular Bone Tissue (Van Giesson and Haemotoxylin stain; x200 magnification). Learn to accurately identify the main features of trabecular bone tissue by clicking on each information hotspot. [Mouse tissue; Attribution to Dr Laura Gregory, Queensland University of Technology]
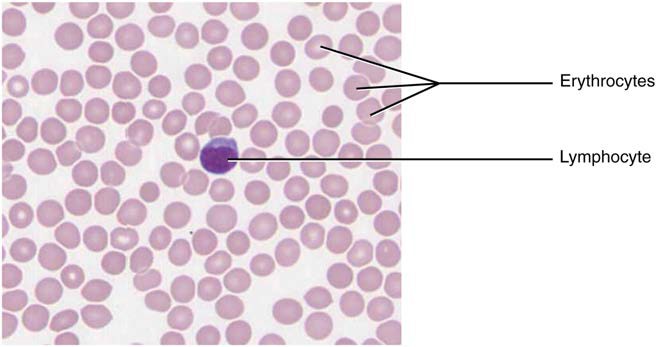
Fluid Connective Tissue
Blood and lymph are fluid connective tissues. Cells circulate in a liquid extracellular matrix containing nutrients, salts and wastes. More information regarding fluid connective tissues can be found in the cardiovascular system chapter (blood) and the lymphatic system chapter (lymph).
Figure 4.14 Blood: A Fluid Connective Tissue Blood is a fluid connective tissue containing erythrocytes and various types of leukocytes that circulate in a liquid extracellular matrix. LM × 1600. [Micrograph provided by the Regents of University of Michigan Medical School © 2012]
Key Terms
adipocytes lipid storage cells
adipose tissue specialised areolar tissue rich in stored fat
areolar tissue a type of connective tissue proper that shows little specialisation with cells dispersed in the matrix
cartilage semi-rigid connective tissue found on the skeleton in areas where flexibility and smooth surfaces support movement
canaliculi (singular = caniculus) channels within the bone matrix that house one of an osteocyte’s many cytoplasmic extensions that it uses to communicate and receive nutrients
central canal longitudinal channel in the centre of each osteon; contains blood vessels, nerves and lymphatic vessels; also known as the Haversian canal
chondrocytes cells of the cartilage
collagenous fibre flexible fibrous proteins that give connective tissue tensile strength
connective tissue type of tissue that serves to hold in place, connect, and integrate the body’s organs and systems
connective tissue proper connective tissue containing a viscous matrix, fibres, and cells
cortical bone tissue dense osseous tissue that can withstand compressive forces
dense connective tissue connective tissue proper that contains many fibres that provide both elasticity and protection
elastic cartilaginous tissue type of cartilaginous tissue, with elastin as the major protein, characterised by rigid support as well as elasticity
elastic fibre fibrous protein within connective tissue that contains a high percentage of the protein elastin that allows the fibres to stretch and return to original size
endosteum delicate membrane composed of dense irregular connective tissue lining the medullary cavity and trabeculae of a bone
fibroblast most abundant cell type in connective tissue, secretes protein fibres and matrix into the extracellular space
fibrocartilage tough form of cartilage, made of thick bundles of collagen fibers embedded in chondroitin sulfate ground substance
fluid connective tissue specialised cells that circulate in a watery fluid containing salts, nutrients, and dissolved proteins
ground substance fluid or semi-fluid portion of the matrix
hyaline cartilaginous tissue most common type of cartilaginous tissue, smooth and made of short collagenous fibres embedded in a chondroitin sulfate ground substance
lacunae (singular = lacuna) small spaces in bone or cartilage tissue that cells occupy
loose connective tissue type of connective tissue proper that shows little specialization with cells dispersed in the matrix
matrix extracellular material which is produced by the cells embedded in it, containing ground substance and fibres
mesenchymal cell adult stem cell from which most connective tissue cells are derived
mesenchyme embryonic tissue from which connective tissue cells derive
osteoblast cell responsible for forming new bone (organic bone matrix, osteoid)
osteoclast cell responsible for resorbing bone
osteocyte mature form of osteoblast that becomes surrounded by osteoid during bone formation; responsible for maintaining the matrix
osteogenic cell undifferentiated cell with high mitotic activity; the only bone cells that divide; they differentiate and develop into osteoblasts
osteoid uncalcified organic bone matrix secreted by osteoblasts
osteon (also, Haversian system) basic structural unit of cortical bone tissue; made of concentric layers (lamellae) of calcified matrix
perforating canal (also, Volkmann’s canal) channel that branches off from the central canal and houses vessels and nerves that extend to the periosteum and endosteum
periosteum dense irregular connective tissue membrane that covers the outer surface of bone tissue and is continuous with ligaments
reticular fibre fine fibrous protein, made of collagen subunits, which cross-link to form supporting “nets” within connective tissue
reticular tissue type of loose connective tissue that provides a supportive framework to soft organs, such as lymphatic tissue, spleen, and the liver
supportive connective tissue type of connective tissue that provides strength to the body and protects soft tissue; includes bone and cartilaginous tissues
trabecular bone tissue (also, spongy bone tissue) trabeculated osseous tissue that supports shifts in weight distribution