Chapter 17: REPRODUCTIVE SYSTEM
Introduction
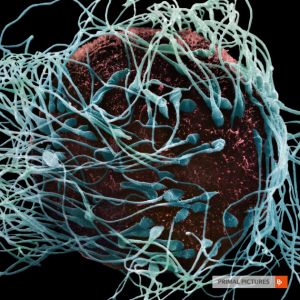
Fertilisation This electron micrograph shows the first stage of fertilisation – where the spermatozoa reach the oocyte. The spermatozoa move through the female reproductive tract towards the unfertilised oocyte using the flagella. [Anatomy.TV, Primal Pictures]
Chapter Objectives
After studying this chapter, you will be able to:
- Describe the anatomy of the male and female reproductive systems, including their accessory structures
- Trace the path of a spermatozoan from its initial production through fertilisation of an oocyte
- Explain the events in the ovary prior to ovulation
The male reproductive system consists of glands and ducts that facilitate the production of spermatozoa and supporting fluids, and transports the spermatozoa to the female reproductive tract. The female reproductive organs function to produce oocytes, receive spermatozoa and provide a suitable environment for fertilisation and development of an embryo and fetus.
Anatomy of the Male Reproductive System
Learning Objectives
By the end of this section, you will be able to:
- Describe the structure and function of the organs of the male reproductive system
- Describe the structure and function of the spermatozoan
Unique for its role in human reproduction, a gamete is a specialised sex cell carrying 23 chromosomes—one half the number in body cells. At fertilisation, the chromosomes in one male gamete, called a spermatozoan (or sperm), combine with the chromosomes in one female gamete, called an oocyte. The function of the male reproductive system is to produce spermatozoan and transfer them to the female reproductive tract. The paired testes are a crucial component in this process, as they produce both spermatozoa and androgens, the hormones that support male reproductive physiology. In humans, the most important male androgen is testosterone. Several accessory organs and ducts aid the process of spermatozoan maturation and transport the spermatozoa and other seminal components to the penis, which delivers spermatozoa to the female reproductive tract. In this section, we examine each of these different structures, and discuss the process of spermatozoa transport.
INTERACTIVE ACTIVITY
Scrotum
The testes are located in a skin-covered, highly pigmented, muscular sack called the scrotum that extends from the body posterior to the penis. This location is important in sperm production, which occurs within the testes, and proceeds more efficiently when the testes are kept 2 to 4°C below core body temperature.
Testes
The testes (singular = testis) are the male gonads—that is, the male reproductive organs. They produce both spermatozoa and androgens, such as testosterone, and are active throughout the reproductive lifespan of the male.
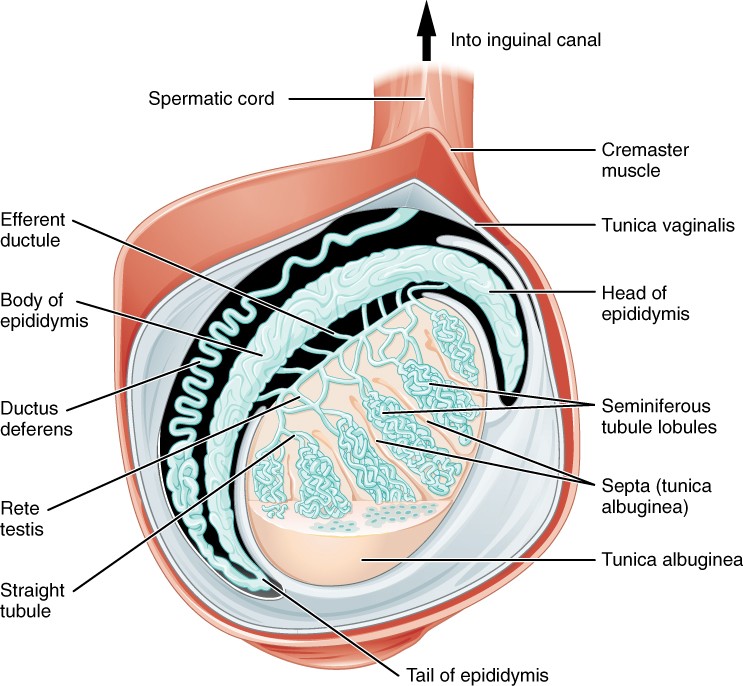
Paired ovals, the testes are each approximately 4 to 5 cm in length and are housed within the scrotum. Connective tissue invaginates the testes to form septa that divide the testis into 300 to 400 structures called lobules. Within the lobules, spermatozoa develop in structures called seminiferous tubules.
The tightly coiled seminiferous tubules form the bulk of each testis. They are composed of developing spermatozoa cells surrounding a lumen, the hollow center of the tubule, where formed spermatozoa are released into the duct system of the testis (Figure 24.4).
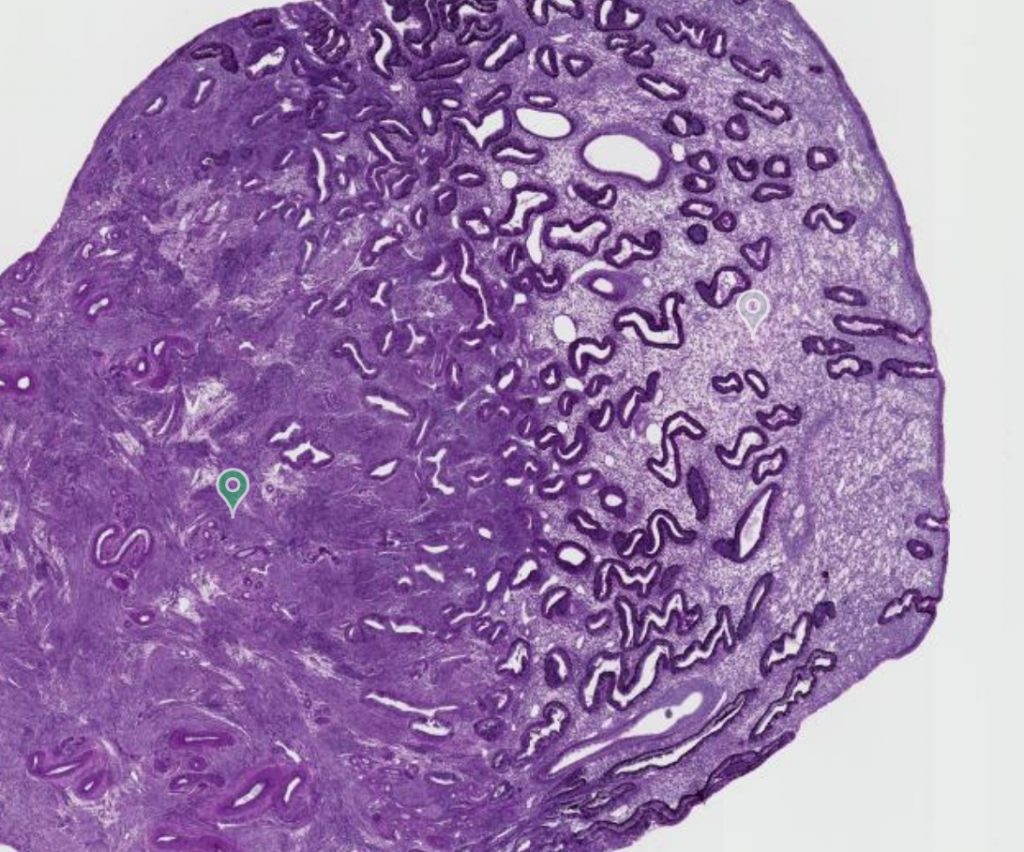
Figure 27.4 Anatomy of the Testis This sagittal view shows the seminiferous tubules, the site of spermatozoa production. Formed spermatozoa are transferred to the epididymis, where they mature. They leave the epididymis during an ejaculation via the ductus deferens.
Structure of Formed Spermatozoa
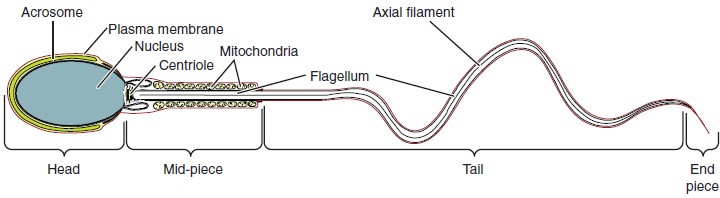
Spermatozoa are smaller than most cells in the body; in fact, the volume of a spermatozoan is 85,000 times less than that of the female gamete. Approximately 100 to 300 million sperm are produced each day, whereas women typically ovulate only one oocyte per month. As is true for most cells in the body, the structure of spermatozoa speaks to their function. Spermatozoa have a distinctive head, mid-piece, and tail region (Figure 27.6). The head of the sperm contains the extremely compact nucleus with very little cytoplasm. These qualities contribute to the overall small size of the spermatozoan (the head is only 5 μm long). A structure called the acrosome covers most of the head of the spermatozoan as a “cap” that is filled with lysosomal enzymes important for preparing spermatozoa to participate in fertilisation. Tightly packed mitochondria fill the mid-piece of the spermatozoa. ATP produced by these mitochondria will power the flagellum, which extends from the neck and the mid-piece through the tail of the spermatozoa, enabling it to move the entire spermatozoan.
Figure 27.6 Structure of Spermatozoa Spermatozoa are divided into a head, containing DNA; a mid-piece, containing mitochondria; and a tail, providing motility. The acrosome is oval and somewhat flattened.
Spermatozoa Transport
To fertilise an oocyte, spermatozoa must be moved from the seminiferous tubules in the testes, through the epididymis, and—later during ejaculation—along the length of the penis and out into the female reproductive tract.
Epididymis
From the lumen of the seminiferous tubules, the immotile spermatozoa are surrounded by testicular fluid and moved to the epididymis (plural = epididymides), a coiled tube attached to the testis where newly formed spermatozoa continue to mature (see Figure 27.4). Though the epididymis does not take up much room in its tightly coiled state, it would be approximately 6 m long if straightened.
Ductus Deferens
During ejaculation, spermatozoa exit the tail of the epididymis and are pushed by smooth muscle contraction to the ductus deferens (also called the vas deferens). The ductus deferens is a thick, muscular tube that is bundled together with connective tissue, blood vessels, and nerves into a structure called the spermatic cord.
From each epididymis, each ductus deferens extends superiorly into the abdominal cavity through the inguinal canal in the abdominal wall. From here, the ductus deferens continues posteriorly to the pelvic cavity, ending posterior to the urinary bladder where it dilates in a region called the ampulla (meaning “flask”).
Spermatozoa make up only 5% of the final volume of seminal fluid (semen). The bulk of seminal fluid is produced by three critical accessory glands of the male reproductive system: the seminal vesicles, the prostate, and the bulbourethral glands (Figure XX).
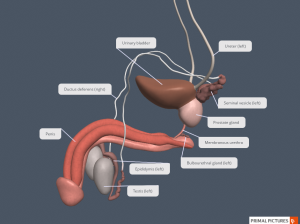
Figure XX Male Reproductive Tract The male reproductive system consists of two reproductive tracts (paired epididymis, paired ductus deferens and a single urethra). Along with the penis, these ducts function to carry spermatozoa and supporting fluids to the female reproductive tract. [Created in Anatomy.TV, Primal Pictures]
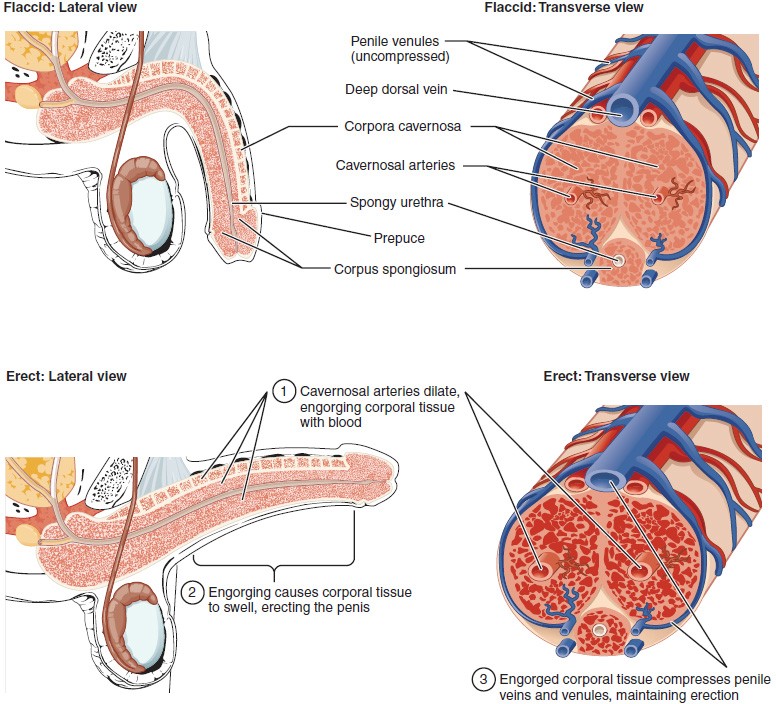
The Penis
The penis is the male organ of copulation (sexual intercourse). The shaft of the penis surrounds the penile (or spongy) urethra (Figure 27.7). The shaft is composed of three column-like chambers of erectile tissue that span the length of the shaft.
Figure 27.7 Cross-Sectional Anatomy of the Penis Three columns of erectile tissue make up most of the volume of the penis.
INTERACTIVE LINK
Anatomy of the Female Reproductive System
Learning Objectives
By the end of this section, you will be able to:
- Describe the structure and function of the organs of the female reproductive system
- Trace the path of an oocyte from ovary to fertilisation
The female reproductive system functions to produce gametes and reproductive hormones, just like the male reproductive system; however, it also has the additional task of supporting the developing fetus and delivering it to the outside world. Unlike its male counterpart, the female reproductive system is located primarily inside the pelvic cavity. Recall that the ovaries are the female gonads. The gamete they produce is called an oocyte.
INTERACTIVE ACTIVITY
Ovaries
Located with the pelvic cavity, the ovaries are the female gonads. Paired ovals, they are each about 2 to 3 cm in length, about the size of an almond.
Oocytes develop within the cortex (outer portion) of the ovary, each surrounded by supporting cells. This grouping of an oocyte and its supporting cells is called a follicle.
The Ovarian Cycle
The ovarian cycle is a set of predictable changes in a female’s oocytes and ovarian follicles. During a woman’s reproductive years, it is a roughly 28-day cycle that can be correlated with, but is not the same as, the menstrual cycle. The cycle includes two interrelated processes: the production of female gametes (oogenesis) and the growth and development of ovarian follicles (folliculogenesis).
The initiation of ovulation—the release of an oocyte from the ovary—marks the transition from puberty into reproductive maturity for women. From then on, throughout a woman’s reproductive years, ovulation of one follicle occurs approximately every 28 days.
Hormonal Control of the Ovarian Cycle
Follicle-stimulating hormone (FSH) and luteinizing hormone (LH) leave the anterior pituitary gland and travel through the bloodstream to the ovaries, where they bind to receptors on the cells of the follicles. FSH stimulates the follicles to grow (hence its name of follicle-stimulating hormone), and the release of LH stimulates the cells of the follicles to produce estrogen.
The more cells a follicle has (that is, the larger and more developed it is), the more estrogen it will produce in response to LH stimulation. The high concentrations of estrogen will stimulate the hypothalamus and pituitary to reduce the production of LH and FSH. This decline in FSH leads to most of the follicles dying. Typically only one follicle, now called the dominant follicle, will survive this reduction in FSH, and this follicle will be the one that releases an oocyte.
When only the one dominant follicle remains in the ovary, it again begins to secrete estrogen. It produces so much estrogen that it triggers the anterior pituitary to respond by secreting large amounts of LH and FSH into the bloodstream.
The large burst of LH (called the LH surge) leads to ovulation of the dominant follicle. The LH surge induces many changes in the dominant follicle. Importantly, the LH surge triggers enzymes to break down structural proteins in the ovary wall on the surface of the bulging dominant follicle. This degradation of the wall, combined with pressure from a large, fluid-filled antrum, results in the expulsion of the oocyte into the peritoneal cavity. This release is ovulation.
The surge of luteinizing hormone (LH) also stimulates a change in the cells that remain in the follicle after the oocyte has been ovulated. This change is called luteinization, and it transforms the collapsed follicle into a new endocrine structure called the corpus luteum, a term meaning “yellowish body” (see Figure XX). Instead of estrogen, the luteinized cells of the corpus luteum begin to produce large amounts of the sex steroid hormone progesterone, a hormone that is critical for the establishment and maintenance of pregnancy.
If pregnancy does not occur within 10 to 12 days, the corpus luteum will stop secreting progesterone and degrade into the corpus albicans, a nonfunctional “whitish body” that will disintegrate in the ovary over a period of several months.
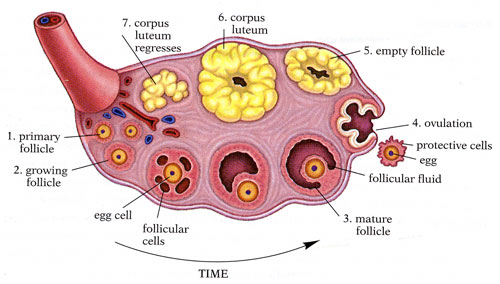
Figure 27.12 Anatomy of the Ovary The maturation of a follicle is shown in an anti-clockwise direction. Follicle-stimulating hormone (FSH) stimulates the growth of a follicle. Once the follicle is mature, it ruptures and releases the oocyte. Cells remaining in the follicle then develop into the corpus luteum. The corpus luteum then regresses into the corpus albicans. [Kimanh Nguyen, CC BY-SA 3.0 <https://creativecommons.org/licenses/by-sa/3.0>, via Wikimedia Commons]
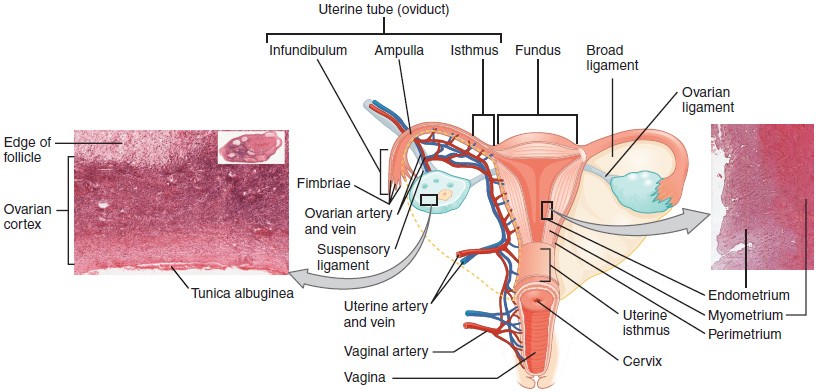
The Uterine Tubes
The uterine tubes (also called fallopian tubes or oviducts) serve as the conduit of the oocyte from the ovary to the uterus (Figure 27.14). Each of the two uterine tubes is close to, but not directly connected to the ovary, and is divided into sections. The isthmus is the narrow medial end of each uterine tube that is connected to the uterus. The wide distal infundibulum flares out with slender, finger-like projections called fimbriae. The middle region of the tube, called the ampulla, is where fertilisation often occurs.
Following ovulation, the oocyte is released into the peritoneal cavity. The nearby uterine tube, either left or right, receives the oocyte. Unlike sperm, oocytes lack flagella, and therefore cannot move on their own. Contractions of the smooth muscle along the length of the uterine tube results in a coordinated movement that sweeps the surface of the ovary and the pelvic cavity. Current flowing toward the uterus is generated by coordinated beating of the cilia that line the lumen of the length of the uterine tube. As a result of these mechanisms, the oocyte is pulled into the interior of the tube. Once inside, the muscular contractions and beating cilia move the oocyte slowly toward the uterus. When fertilisation does occur, spermatozoa typically meet the oocyte while it is still moving through the ampulla.
If the oocyte is successfully fertilised, the resulting zygote will begin to divide into two cells, then four, and so on, as it makes its way through the uterine tube and into the uterus. There, it will implant and continue to grow. If the oocyte is not fertilised, it will simply degrade—either in the uterine tube or in the uterus, where it may be shed with the next menstrual period.
Figure 27.14 Ovaries, Uterine Tubes, and Uterus This anterior view shows the relationship of the ovaries, uterine tubes and uterus. Spermatozoa enter through the vagina, and fertilisation of an ovulated oocyte usually occurs in the ampulla of the uterine tube. From left to right, LM × 400, LM × 20. [Micrographs provided by the Regents of University of Michigan Medical School © 2012]
INTERACTIVE LINK
The Uterus and Cervix
The uterus is the muscular organ that nourishes and supports the growing embryo (see Figure 27.14). Its average size is approximately 5 cm wide by 7 cm long when a female is not pregnant. It has three sections. The portion of the uterus superior to the opening of the uterine tubes is called the fundus. The middle section of the uterus is called the body of uterus (or corpus). The cervix is the narrow inferior portion of the uterus that projects into the vagina.
The wall of the uterus is made up of three layers. The most superficial layer is the serous membrane, or perimetrium, which consists of epithelial tissue that covers the exterior portion of the uterus. The middle layer, or myometrium, is a thick layer of smooth muscle responsible for uterine contractions. Most of the uterus is myometrial tissue, and the muscle fibres run horizontally, vertically, and diagonally, allowing the powerful contractions that occur during labor and the less powerful contractions (or cramps) that help to expel menstrual blood during a woman’s period. Anteriorly directed myometrial contractions also occur near the time of ovulation, and are thought to possibly facilitate the transport of sperm through the female reproductive tract. The innermost layer of the uterus is called the endometrium. The endometrium contains a connective tissue lining, the lamina propria, which is covered by epithelial tissue that lines the lumen. Structurally, the endometrium consists of two layers: the stratum basalis and the stratum functionalis (the basal and functional layers). The stratum basalis layer is part of the lamina propria and is adjacent to the myometrium; this layer does not shed during menses. In contrast, the thicker stratum functionalis layer contains the glandular portion of the lamina propria and the endothelial tissue that lines the uterine lumen. It is the stratum functionalis that grows and thickens in response to increased levels of estrogen and progesterone. This inner functional layer provides the proper site of implantation for the fertilised oocyte, and—should fertilisation not occur—it is only the stratum functionalis layer of the endometrium that sheds during menstruation.
INTERACTIVE LINK
Vagina
The vagina is a muscular canal (approximately 10 cm long) that serves as the entrance to the reproductive tract. It also serves as the exit from the uterus during menses and childbirth. The outer walls of the anterior and posterior vagina are formed into longitudinal columns, or ridges, and the superior portion of the vagina—called the fornix—meets the protruding uterine cervix. The walls of the vagina are lined with transverse folds called rugae.
INTERACTIVE ACTIVITY
External Female Genitalia
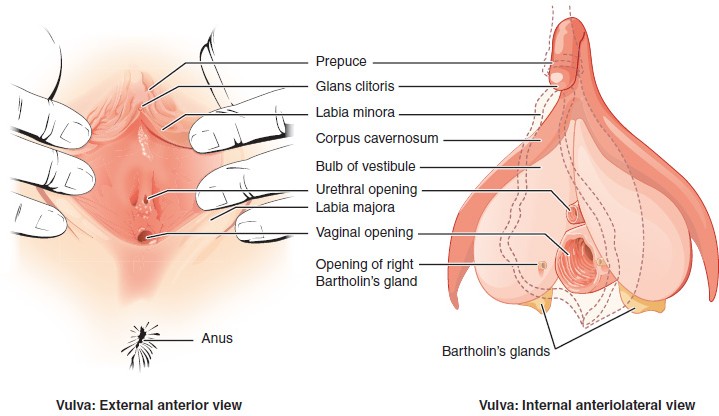
The external female reproductive structures are referred to collectively as the vulva (Figure 27.10). The mons pubis is a pad of fat that is located anteriorly, superficial to the pubic bone. After puberty, it becomes covered in pubic hair. The labia majora (labia = “lips”; majora = “larger”) are folds of hair-covered skin that begin just posterior to the mons pubis. The thinner and more pigmented labia minora (labia = “lips”; minora = “smaller”) extend medial to the labia majora. Although they naturally vary in shape and size from woman to woman, the labia minora serve to protect the female urethra and the entrance to the female reproductive tract.
The superior, anterior portions of the labia minora come together to encircle the clitoris, an organ that has abundant nerves that make it important in sexual sensation. The vaginal opening is located posterior to the opening of the urethra and anterior to the anus.
Figure 27.10 The Vulva The external female genitalia are referred to collectively as the vulva.
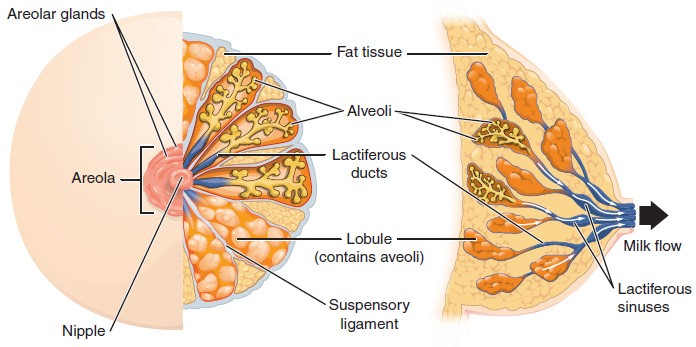
The Female Breasts
Whereas the breasts are located far from the other female reproductive organs, they are considered accessory organs of the female reproductive system. The function of the breasts is to supply milk to an infant in a process called lactation. The external features of the breast include a nipple surrounded by a pigmented areola (Figure 27.17), whose colouration may deepen during pregnancy.
Breast milk is produced by the mammary glands, which are modified sweat glands. The milk itself exits the breast through the nipple via 15 to 20 lactiferous ducts that open on the surface of the nipple. These lactiferous ducts connect to a glandular lobe within the breast itself that contains groups of milk-secreting cells in clusters called alveoli (see Figure 27.17). The lobes themselves are surrounded by fat tissue, which determines the size of the breast; breast size differs between individuals and does not affect the amount of milk produced. Supporting the breasts are multiple bands of connective tissue called suspensory ligaments that connect the breast tissue to the dermis of the overlying skin.
Figure 27.17 Anatomy of the Breast During lactation, milk moves from the alveoli through the lactiferous ducts to the nipple.
Key Terms
alveoli (of the breast) milk-secreting cells in the mammary gland
ampulla (of the uterine tube) middle portion of the uterine tube in which fertilisation often occurs
antrum fluid-filled chamber that characterises a mature tertiary (antral) follicle
areola highly pigmented, circular area surrounding the raised nipple and containing areolar glands that secrete fluid important for lubrication during suckling
body of uterus middle section of the uterus
bulbourethral glands (also, Cowper’s glands) glands that secrete a lubricating mucus that cleans and lubricates the urethra prior to and during ejaculation
cervix elongate inferior end of the uterus where it connects to the vagina
clitoris (also, glans clitoris) nerve-rich area of the vulva that contributes to sexual sensation during intercourse
corpus albicans nonfunctional structure remaining in the ovarian stroma following structural and functional regression of the corpus luteum
corpus luteum transformed follicle after ovulation that secretes progesterone
ductus deferens (also, vas deferens) duct that transports sperm from the epididymis through the spermatic cord and into the ejaculatory duct; also referred as the vas deferens
ejaculatory duct duct that connects the ampulla of the ductus deferens with the duct of the seminal vesicle at the prostatic urethra
endometrium inner lining of the uterus, part of which builds up during the secretory phase of the menstrual cycle and then sheds with menses
epididymis (plural = epididymides) coiled tubular structure in which sperm start to mature and are stored until ejaculation
fimbriae fingerlike projections on the distal uterine tubes
follicle ovarian structure of one oocyte and surrounding cells
folliculogenesis development of ovarian follicles under the stimulation of hormones
fundus (of the uterus) domed portion of the uterus that is superior to the uterine tubes
gamete reproductive cell that contributes genetic material to form an offspring
gonads reproductive organs (testes in men and ovaries in women) that produce gametes and reproductive hormones
infundibulum (of the uterine tube) wide, distal portion of the uterine tube terminating in fimbriae
inguinal canal opening in abdominal wall that connects the testes to the abdominal cavity
isthmus narrow, medial portion of the uterine tube that joins the uterus
labia majora hair-covered folds of skin located posterior to the mons pubis
labia minora thin, pigmented, hairless folds of skin located medial and deep to the labia majora
lactiferous ducts ducts that connect the mammary glands to the nipple and allow for the transport of milk
mammary glands glands inside the breast that secrete milk
menses shedding of the inner portion of the endometrium out though the vagina; also referred to as menstruation
menses phase phase of the menstrual cycle in which the endometrial lining is shed
menstrual cycle approximately 28-day cycle of changes in the uterus consisting of a menses phase, a proliferative phase, and a secretory phase
mons pubis mound of fatty tissue located anterior to the vulva
myometrium smooth muscle layer of uterus that allows for uterine contractions during labor and expulsion of menstrual blood
oocyte cell that results from the division of the oogonium and undergoes meiosis I at the LH surge and meiosis II at fertilisation to become a haploid ovum
oogenesis process by which oogonia divide by mitosis to primary oocytes, which undergo meiosis to produce the secondary oocyte and, upon fertilisation, the ovum
oogonia ovarian stem cells that undergo mitosis during female fetal development to form primary oocytes
ovarian cycle approximately 28-day cycle of changes in the ovary consisting of a follicular phase and a luteal phase
ovaries female gonads that produce oocytes and sex steroid hormones (notably estrogen and progesterone)
ovulation release of an oocyte and associated cells from an ovary
penis male organ of copulation
perimetrium outer (superficial) epithelial layer of uterine wall
prostate gland doughnut-shaped gland at the base of the bladder surrounding the prostatic urethra and contributing fluid to semen during ejaculation
rugae (of the vagina) folds of skin in the vagina that allow it to stretch during intercourse and childbirth
scrotum external pouch of skin and muscle that houses the testes
semen ejaculatory fluid composed of spermatozoa and secretions from the seminal vesicles, prostate, and bulbourethral glands
seminal vesicle gland that produces seminal fluid, which contributes to semen
seminiferous tubules tube structures within the testes where spermatogenesis occurs
spermatozoan male gamete
spermatic cord bundle of nerves and blood vessels that supplies the testes; contains ductus deferens
spermatogenesis formation of new sperm, occurs in the seminiferous tubules of the testes
suspensory ligaments bands of connective tissue that suspend the breast onto the thoracic wall by attachment to the overlying dermis
testes (singular = testis) male gonads
uterine tubes (also, fallopian tubes or oviducts) ducts that facilitate transport of an ovulated oocyte to the uterus
uterus muscular hollow organ in which a fertilised oocyte develops into a fetus
vagina tunnel-like organ that provides access to the uterus for the insertion of semen and from the uterus for the birth of a baby
vulva external female genitalia