Chapter 15: DIGESTIVE SYSTEM
Introduction

Villi Finger-like projections (villi) increase the surface area in the small intestine for absorption of nutrients. [www.scientificanimations.com, CC BY-SA 4.0 <https://creativecommons.org/licenses/by-sa/4.0>, via Wikimedia Commons]
Chapter Objectives
After studying this chapter, you will be able to:
- List and describe the anatomy of the organs and accessory organs of the digestive system
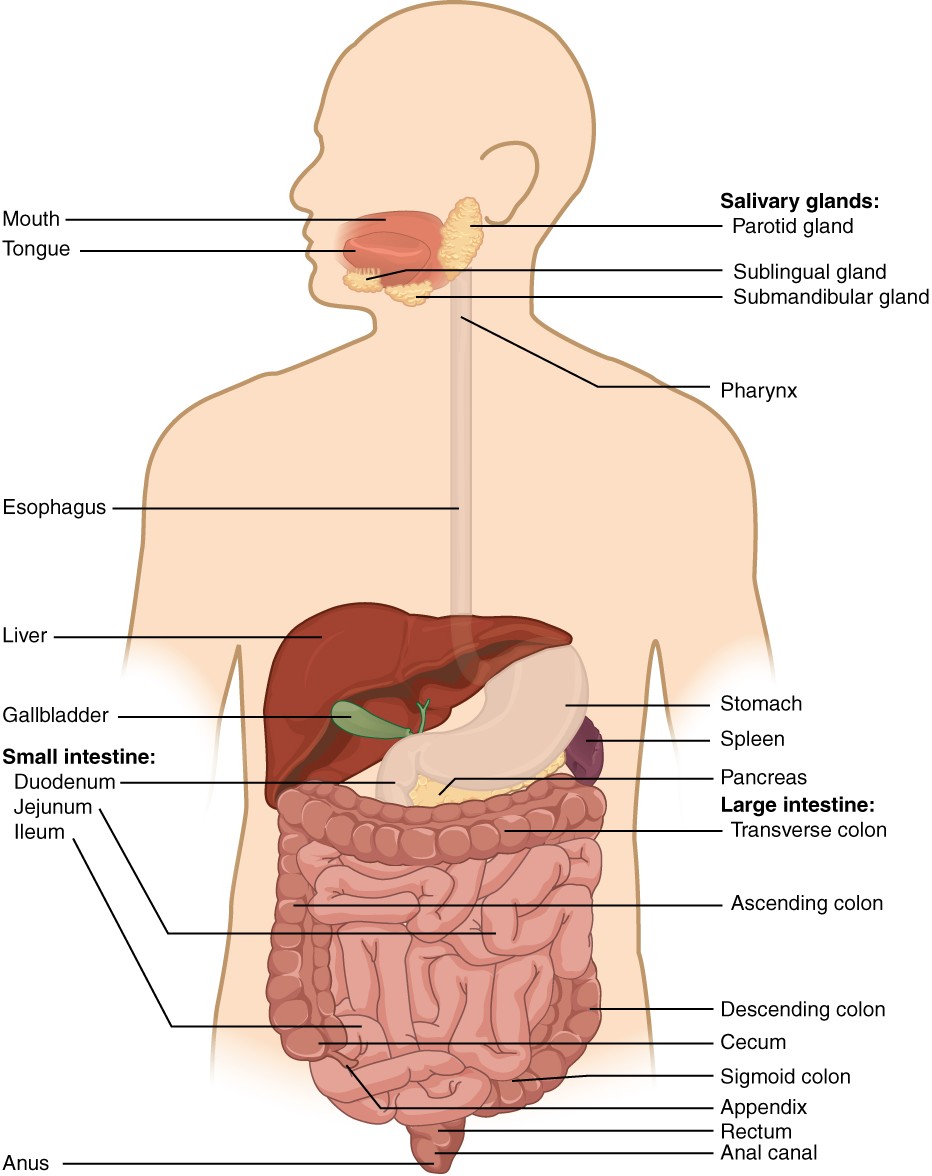
The digestive system consists of the gastrointestinal tract and accessory digestive organs that produce secretions to assist with the breakdown of food in order for absorption to occur. The major parts of the digestive system includes the mouth, pharynx and oesophagus, stomach, small intestine, large intestine and accessory digestive glands (e.g. salivary glands, liver, pancreas).
Overview of the Digestive System
Learning Objectives
By the end of this section, you will be able to:
- Identify the organs and accessory organs of the gastrointestinal tract from proximal to distal
- Describe the four fundamental tissue layers of the gastrointestinal tract
- Explain how the peritoneum anchors the digestive organs
The function of the digestive system is to break down the foods you eat, release their nutrients, and absorb those nutrients into the body. Although the small intestine is the workhorse of the system, where the majority of digestion occurs, and where most of the released nutrients are absorbed into the blood or lymph, each of the digestive system organs makes a vital contribution to this process (Figure 23.2).
Figure 23.2 Components of the Digestive System All digestive organs play integral roles in the life-sustaining process of digestion.
As is the case with all body systems, the digestive system does not work in isolation; it functions cooperatively with the other systems of the body. Consider for example, the interrelationship between the digestive and cardiovascular systems. Arteries supply the digestive organs with oxygen and processed nutrients, and veins drain the digestive tract. These intestinal veins, constituting the hepatic portal system, are unique; they do not return blood directly to the heart. Rather, this blood is diverted to the liver where its nutrients are off-loaded for processing before blood completes its circuit back to the heart. At the same time, the digestive system provides nutrients to the heart muscle and vascular tissue to support their functioning. The interrelationship of the digestive and endocrine systems is also critical. Hormones secreted by several endocrine glands, and organs with endocrine function contribute to the control of digestion and nutrient metabolism. In turn, the digestive system provides the nutrients to fuel endocrine function. Table 23.1 gives a quick glimpse at how these other systems contribute to the functioning of the digestive system.
Contribution of Other Body Systems to the Digestive System
| Body System | Benefits received by the digestive system |
| Cardiovascular | Blood supplies digestive organs with oxygen and processed nutrients |
| Endocrine | Endocrine hormones help regulate secretion in digestive glands and accessory organs |
| Integumentary | Skin helps protect digestive organs and synthesises vitamin D for calcium absorption |
| Lymphatic | Lymphatic tissues defend against entry of pathogens; lacteals absorb lipids; and lymphatic vessels transport lipids to bloodstream |
| Muscular | Skeletal muscles support and protect abdominal organs |
| Nervous | Sensory and motor neurons help regulate secretions and muscle contractions in the digestive tract |
| Respiratory | Respiratory organs provide oxygen and remove carbon dioxide |
| Skeletal | Bones help protect and support digestive organs |
| Urinary | Kidneys convert vitamin D into its active form, allowing calcium absorption in the small intestine |
Table 23.1
Digestive System Organs
The easiest way to understand the digestive system is to divide its organs into two main categories. The first group is the organs that make up the gastrointestinal tract. Accessory digestive organs comprise the second group and are critical for orchestrating the breakdown of food and the absorption of nutrients into the body. Accessory digestive organs, despite their name, are critical to the function of the digestive system.
Gastrointestinal (GI) Tract Organs
Also called the alimentary canal (aliment = “to nourish”) or gut, the gastrointestinal (GI) tract is a one-way tube about 7.6 metres in length during life and closer to 10.7 metres in length when measured after death, once smooth muscle tone is lost. The main function of the organs of the gastrointestinal tract is to nourish the body. This tube begins at the mouth and terminates at the anus. Between those two points, the canal is modified as the pharynx, oesophagus, stomach, and small and large intestines to fit the functional needs of the body.
Accessory Structures
Each accessory digestive organ aids in the breakdown of food. Within the mouth, the teeth and tongue begin mechanical digestion, whereas the salivary glands begin chemical digestion. Once food products enter the small intestine, the gallbladder, liver, and pancreas release secretions—such as bile and enzymes—essential for digestion to continue.
INTERACTIVE ACTIVITY
Blood Supply
The blood vessels serving the digestive system have two functions. They transport the protein and carbohydrate nutrients absorbed by mucosal cells after food is digested in the lumen. Lipids are absorbed via lacteals, tiny structures of the lymphatic system. The blood vessels’ second function is to supply the organs of the gastrointestinal tract with the nutrients and oxygen needed to drive their cellular processes.
Specifically, the more superior parts of the gastrointestinal tract are supplied with blood by arteries branching off the aortic arch and thoracic aorta. Inferiorly, the gastrointestinal tract is supplied with blood by arteries branching from the abdominal aorta. The coeliac trunk supplies the liver, stomach, and duodenum, whereas the superior and inferior mesenteric arteries supply blood to the remaining small and large intestines.
The veins that collect nutrient-rich blood from the small intestine (where most absorption occurs) drain into the hepatic portal system. This venous network transports the blood into the liver where the nutrients are either processed or stored for later use. Only then does the blood drained from the gastrointestinal tract viscera circulate back to the heart.
INTERACTIVE ACTIVITY
Review the image panels of the Arteries and Veins of the Abdomen. This activity requires you to move from one slide to the next. You can do this by clicking either the arrowsbeside the image, or the buttons below the image. [Created in Anatomy.TV, Primal Pictures]
The abdominal aorta gives rise to the coeliac trunk, superior mesenteric and inferior mesenteric arteries. The inferior vena cava returns deoxygenated blood to the heart [1st panel]. The hepatic portal vein is responsible for transporting nutrient-rich blood from the intestines to the liver [2nd panel].
Questions:
(a) Describe the termination of the abdominal aorta (ie. name the arteries the abdominal aorta divides into).
(b) Observe the vessels that unite to form the hepatic portal vein and describe where the blood is draining from.
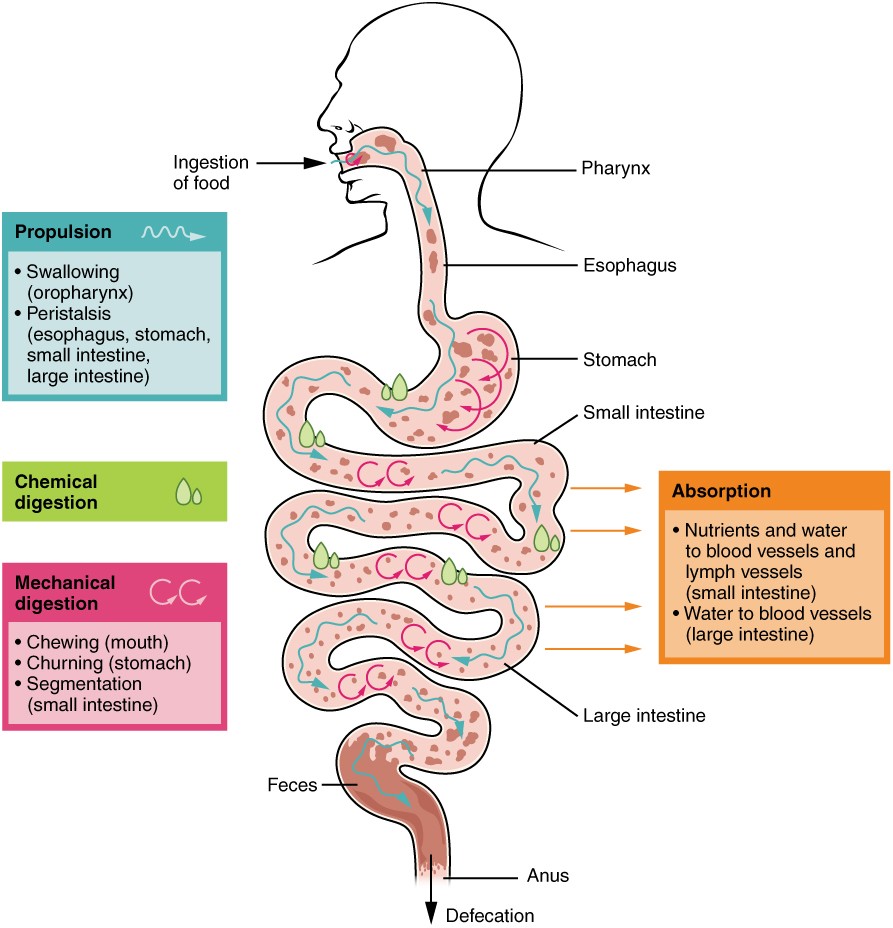
Digestive Processes
The processes of digestion include six activities: ingestion, propulsion, mechanical or physical digestion, chemical digestion, absorption, and defecation.
The first of these processes, ingestion, refers to the entry of food into the gastrointestinal tract through the mouth. There, the food is chewed and mixed with saliva, which contains enzymes that begin breaking down the the food. Mastication (chewing) increases the surface area of the food and allows an appropriately sized bolus to be produced.
Food leaves the mouth when the tongue and pharyngeal muscles propel it into the oesophagus. This act of swallowing, the last voluntary act until defecation, is an example of propulsion, which refers to the movement of food through the digestive tract. It includes both the voluntary process of swallowing and the involuntary process of peristalsis. Peristalsis consists of sequential, alternating waves of contraction and relaxation of gastrointestinal wall smooth muscles, which act to propel food along.
INTERACTIVE LINK
Digestion includes both mechanical and chemical processes. Mechanical digestion is a purely physical process that does not change the chemical nature of the food. Instead, it makes the food smaller to increase both surface area and mobility. It includes mastication, or chewing, as well as tongue movements that help break food into smaller bits and mix food with saliva. Although there may be a tendency to think that mechanical digestion is limited to the first steps of the digestive process, it occurs after the food leaves the mouth, as well. The mechanical churning of food in the stomach serves to further break it apart and expose more of its surface area to digestive juices, creating an acidic “soup” called chyme. Segmentation, which occurs mainly in the small intestine, consists of localised contractions of circular muscle of the muscularis layer of the gastrointestinal tract. These contractions isolate small sections of the intestine, moving their contents back and forth while continuously subdividing, breaking up, and mixing the contents. By moving food back and forth in the intestinal lumen, segmentation mixes food with digestive juices and facilitates absorption.
In chemical digestion, starting in the mouth, digestive secretions break down complex food molecules into their chemical building blocks.
Food that has been broken down is of no value to the body unless it enters the bloodstream and its nutrients are put to work. This occurs through the process of absorption, which takes place primarily within the small intestine. There, most nutrients are absorbed from the lumen of the gastrointestinal tract into the bloodstream through the epithelial cells that make up the mucosa (gastrointestinal lining). Lipids are absorbed into lacteals and are transported via the lymphatic vessels to the bloodstream.
In defecation, the final step in digestion, undigested materials are removed from the body as faeces.
Figure 23.6 Digestive Processes The digestive processes are ingestion, propulsion, mechanical digestion, chemical digestion, absorption, and defecation.
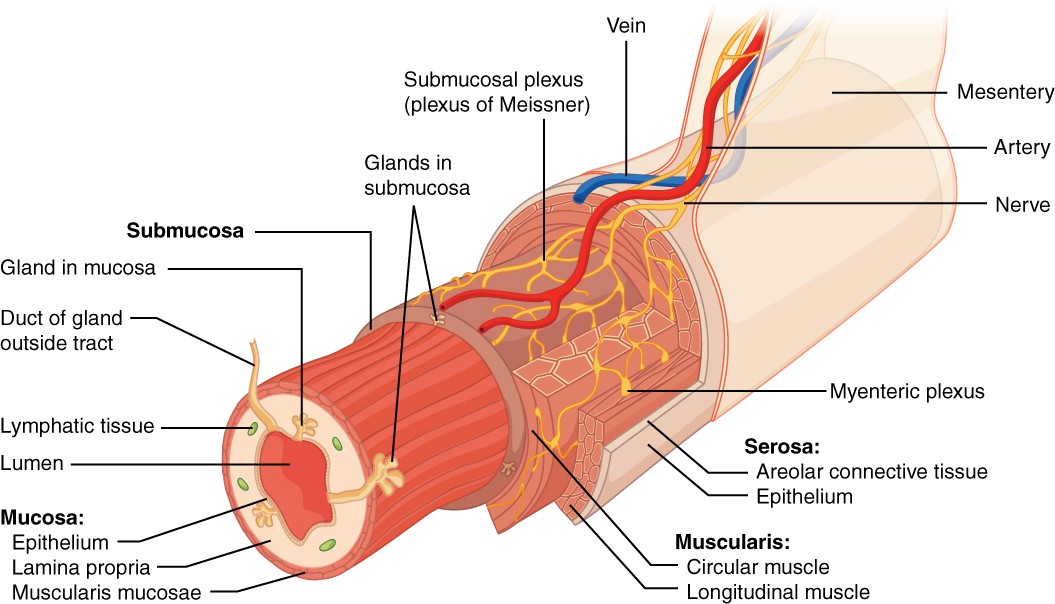
Histology of the Gastrointestinal Tract
Throughout its length, the gastrointestinal tract is composed of the same four tissue layers; the details of their structural arrangements vary to fit their specific functions. Starting from the lumen and moving superficially, these layers are the mucosa, submucosa, muscularis externa, and serosa, which is continuous with the mesentery (see Figure 23.3).
Figure 23.3 Layers of the Gastrointestinal Tract The wall of the gastrointestinal tract has four basic tissue layers: the mucosa, submucosa, muscularis, and serosa.
The mucosa is referred to as a mucous membrane, because mucus production is a characteristic feature of the epithelium. The membrane consists of epithelium, which is in direct contact with ingested food, and the lamina propria, a layer of connective tissue analogous to the dermis. In addition, the mucosa has a thin, smooth muscle layer, called the muscularis mucosa (not to be confused with the muscularis externa layer, described below).
Epithelium—In the mouth, pharynx, oesophagus, and anal canal, the epithelium is primarily a non-keratinised, stratified squamous epithelium. In the stomach and intestines, it is a simple columnar epithelium. Notice that the epithelium is in direct contact with the lumen, the space inside the gastrointestinal tract. Epithelial cells have a very brief lifespan, averaging from only a couple of days (in the mouth) to about a week (in the gut). This process of rapid renewal helps preserve the health of the gastrointestinal tract, despite the wear and tear resulting from continued contact with foodstuffs.
Lamina propria—In addition to loose connective tissue, the lamina propria contains numerous blood and lymphatic vessels that transport nutrients absorbed through the gastrointestinal tract to other parts of the body.
Muscularis mucosa—This thin layer of smooth muscle is in a constant state of tension, pulling the mucosa of the stomach and small intestine into undulating folds. These folds dramatically increase the surface area available for digestion and absorption.
As its name implies, the submucosa lies immediately superficial to the mucosa. A broad layer of dense connective tissue, it connects the overlying mucosa to the underlying muscularis externa. It includes blood and lymphatic vessels (which transport absorbed nutrients), and a scattering of submucosal glands that release digestive secretions. Additionally, it serves as a conduit for a dense branching network of nerves, the submucosal plexus.
The third layer of the gastrointestinal tract is the muscularis externa. The muscularis externa in the small intestine is composed of a double layer of smooth muscle: an inner circular layer and an outer longitudinal layer. The contractions of these layers promote mechanical digestion, expose more of the food to digestive chemicals, and move the chyme along the canal. In the most proximal and distal regions of the gastrointestinal tract, including the mouth, pharynx, anterior part of the oesophagus, and external anal sphincter, the muscularis externa is composed of skeletal muscle, which faciliates voluntary control over swallowing and defecation. The basic two-layer structure found in the small intestine is modified in the organs proximal and distal to it.
The serosa is the portion of the gastrointestinal tract superficial to the muscularis externa. Present only in the region of the gastrointestinal tract within the abdominal cavity, it consists of a layer of visceral peritoneum overlying a layer of loose connective tissue. Instead of serosa, the mouth, pharynx, and oesophagus have a dense sheath of collagen fibres called the adventitia. These tissues serve to hold the gastrointestinal tract in place near the holding them to the dorsal surface of the abdominal wall.
The Mouth, Pharynx, and Oesophagus
Learning Objectives
By the end of this section, you will be able to:
- Describe the structures of the mouth, including its three accessory digestive organs
- Name the different types of teeth according to name, location, and function
The Mouth
The cheeks, tongue, and palate frame the mouth, which is also called the oral cavity (or buccal cavity). The structures of the mouth are illustrated in Figure 23.7.
The lips cover the orbicularis oris muscle, which regulates what comes in and goes out of the mouth. The cheeks make up the oral cavity’s sidewalls. While their outer covering is skin, their inner covering is mucous membrane. This membrane is made up of non-keratinised, stratified squamous epithelium.
When you are chewing, you do not find it difficult to breathe simultaneously. The next time you have food in your mouth, notice how the arched shape of the roof of your mouth allows you to handle both digestion and respiration at the same time. This arch is called the palate. The anterior region of the palate serves as a wall (or septum) between the oral and nasal cavities as well as a rigid shelf against which the tongue can push food and given its bony structure, is known as the hard palate. If you run your tongue along the roof of your mouth, you’ll notice that the hard palate ends in the posterior oral cavity, and the tissue becomes fleshier. This part of the palate, known as the soft palate, is composed mainly of skeletal muscle. You can therefore manipulate, subconsciously, the soft palate—for instance, to yawn, swallow, or sing (see Figure 23.7).
A fleshy bead of tissue called the uvula drops down from the center of the posterior edge of the soft palate. When you swallow, the soft palate and uvula move upward, helping to keep foods and liquid from entering the nasal cavity. The palatine, lingual and nasopharyngeal tonsils are clusters of lymphoid tissue that protect the pharynx.
The Tongue
The tongue is positioned over the floor of the oral cavity. The tongue facilitates ingestion, mechanical digestion, chemical digestion, sensation (taste, texture and temperature of food), swallowing and vocalisation (see Figure 23.7).
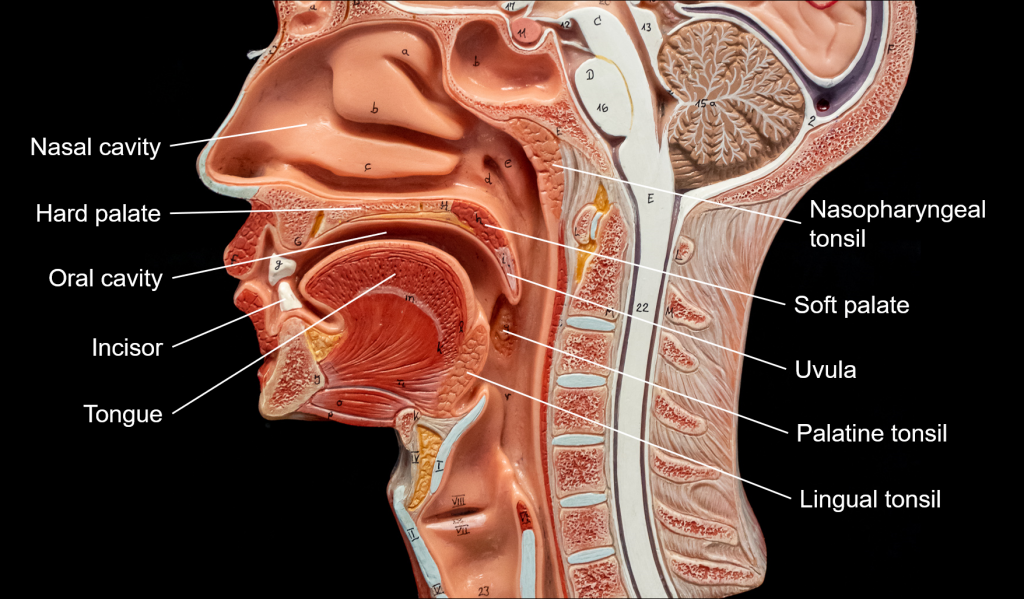
Figure 23.7 Mouth The mouth includes the lips, tongue, palate, gums, and teeth.
The Salivary Glands
Many small salivary glands are housed within the mucous membranes of the mouth and tongue. These minor exocrine glands are constantly secreting saliva, either directly into the oral cavity or indirectly through ducts, even while you sleep. In fact, an average of 1 to 1.5 litres of saliva is secreted each day. Usually just enough saliva is present to moisten the mouth and teeth. Secretion increases when you eat, because saliva is essential to moisten food and initiate the chemical breakdown.
The Major Salivary Glands
Outside the oral mucosa are three pairs of major salivary glands, which secrete the majority of saliva into ducts that open into the mouth:
- The submandibular glands, which are in the floor of the mouth, secrete saliva into the mouth.
- The sublingual glands, which lie inferior to the tongue.
- The parotid glands lie deep to the skin anterior to the ears.
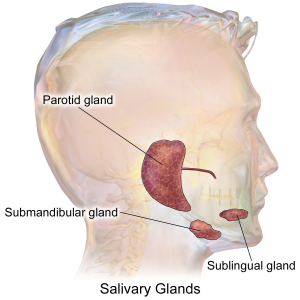
Figure 23.9 Salivary glands The major salivary glands are located outside the oral mucosa and deliver saliva into the mouth through ducts. [Blausen.com staff (2014). “Medical gallery of Blausen Medical 2014”. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436., CC BY 3.0 <https://creativecommons.org/licenses/by/3.0>, via Wikimedia Commons]
The Teeth
The teeth are organs similar to bones that you use to tear, grind, and otherwise mechanically break down food.
Types of Teeth
During the course of your lifetime, you have two sets of teeth. Your deciduous teeth, or baby teeth, first begin to appear at about 6 months of age. These teeth are replaced by permanent teeth. Moving from the center of the mouth laterally, these are as follows (Figure 23.10):
- The eight incisors, four top and four bottom, are the sharp front teeth you use for biting into food.
- The four canines are posterior to the incisors and have a pointed edge to tear up food.
- Posterior to the canines are the eight premolars, which have an overall flatter shape with two rounded cusps useful for mashing foods.
- The most posterior and largest are the 12 molars, which have several pointed cusps used to crush food so it is ready for swallowing. The third members of each set of three molars, top and bottom, are commonly referred to as the wisdom teeth, because their eruption is commonly delayed until early adulthood.
INTERACTIVE ACTIVITY
Explore the image panels of the Types of Teeth. This activity requires you to move from one slide to the next. You can do this by clicking either the arrows beside the image, or the buttons below the image. [Created in Anatomy.TV, Primal Pictures]
Questions:
(a) Name the bones that form the upper and lower jaw.
(b) What are the structural differences between the premolars and molars?
Table 23.4 Digestive Functions of the Mouth
| Structure | Action | Outcome |
| Lips and cheeks | Confine food between teeth | Food is chewed evenly during mastication |
| Salivary glands | Secrete saliva | Moisten and lubricate the lining of the mouth and pharynx Moisten, soften, and dissolve food
Clean the mouth and teeth Salivary amylase breaks down starch |
| Teeth | Shred and crush food | Break down solid food into smaller particles for deglutition |
The Pharynx
The pharynx (throat) is involved in both digestion and respiration. It receives food and air from the mouth, and air from the nasal cavities. When food enters the pharynx, involuntary muscle contractions close off the air passageways.
A short tube of skeletal muscle lined with a mucous membrane, the pharynx runs from the posterior oral and nasal cavities to the opening of the oesophagus and larynx. It has three subdivisions. The most superior, the nasopharynx, is involved only in breathing and speech. The other two subdivisions, the oropharynx and the laryngopharynx, are used for both breathing and digestion. The oropharynx begins inferior to the nasopharynx and is continuous below with the laryngopharynx (Figure 23.12). The inferior border of the laryngopharynx connects to the oesophagus, whereas the anterior portion connects to the larynx, allowing air to flow into the bronchial tree.
Usually during swallowing, the soft palate and uvula rise reflexively to close off the entrance to the nasopharynx. At the same time, the larynx is pulled superiorly and the cartilaginous epiglottis, its most superior structure, folds inferiorly, covering the glottis (the opening to the larynx); this process effectively blocks access to the trachea and bronchi. When the food “goes down the wrong way,” it goes into the trachea. When food enters the trachea, the reaction is to cough, which usually forces the food up and out of the trachea, and back into the pharynx.
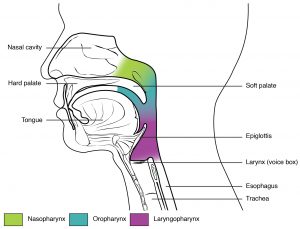
Figure 23.12 Pharynx The pharynx runs from the nostrils to the oesophagus and the larynx. [Organs and Structures of the Respiratory System. Authored by: OpenStax CNX. Provided by: OpenStaxCollege. Located at: http://cnx.org/contents/t2sgkCQ-@8/Organs-and-Structures-of-the-R.. License: CC BY: Attribution. License Terms: Download for free at http://cnx.org/contents/b76b2090-243e-429a-8144-2e45bda6ab75@8]
The Oesophagus
The oesophagus is a muscular tube that connects the pharynx to the stomach. It is approximately 25.4 cm in length, located posterior to the trachea, and remains in a collapsed form when not engaged in swallowing. As you can see in Figure 23.12, the oesophagus runs a mainly straight route through the mediastinum of the thorax. To enter the abdomen, the oesophagus penetrates the thoracic diaphragm through an opening called the oesophageal hiatus.
Histology of the Oesophagus
The mucosa of the oesophagus is made up of an epithelial lining that contains non-keratinised, stratified squamous epithelium. This epithelium protects against erosion from food particles.
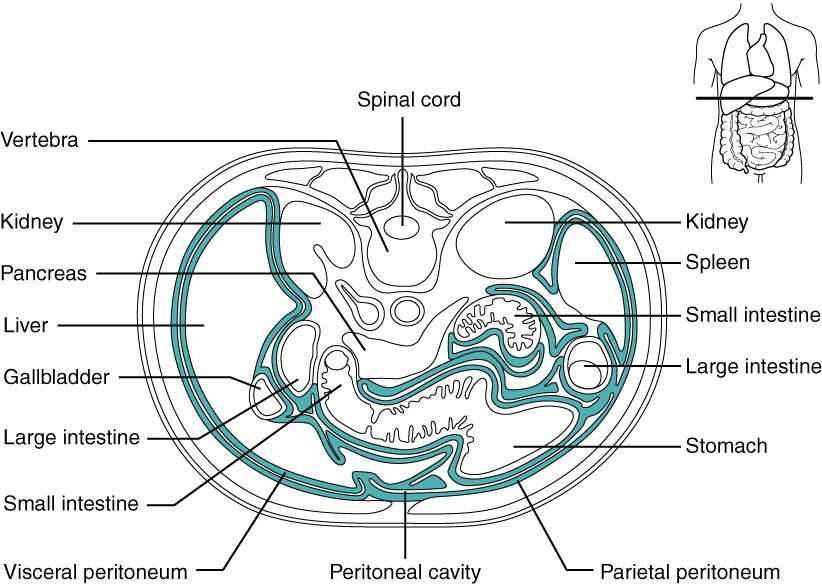
The Peritoneum
The digestive organs within the abdominal cavity are held in place by the peritoneum, a broad serous membranous sac made up of squamous epithelial tissue surrounded by connective tissue. It is composed of two different regions: the parietal peritoneum, which lines the abdominal wall, and the visceral peritoneum, which envelopes the abdominal organs (Figure 23.4). The peritoneal cavity is the space bounded by the visceral and parietal peritoneal surfaces. A few millilitres of watery fluid act as a lubricant to minimise friction between the serosal surfaces of the peritoneum.
Figure 23.4 The Peritoneum A cross-section of the abdomen shows the relationship between abdominal organs and the peritoneum (darker lines).
The visceral peritoneum includes multiple large folds that envelope various abdominal organs, holding them to the dorsal surface of the abdominal wall, these organs are described as intraperitoneal. Within these folds are blood vessels, lymphatic vessels, and nerves that innervate the organs with which they are in contact, supplying their adjacent organs. The five major peritoneal folds are described in Table 23.2. The first portion of the small intestine (called the duodenum), the pancreas, and portions of the large intestine (the ascending and descending colon, and the rectum) remain completely or partially posterior to the peritoneum. Thus, the location of these organs is described as retroperitoneal.
Table 23.2 The Five Major Peritoneal Folds
|
Fold |
Description |
|
Greater omentum |
Apron-like structure that lies superficial to the small intestine and transverse colon; a site of fat deposition in people who are overweight |
|
Falciform ligament |
Anchors the liver to the anterior abdominal wall and inferior border of the thoracic diaphragm |
|
Lesser omentum |
Suspends the stomach from the inferior border of the liver; provides a pathway for structures connecting to the liver |
|
Mesentery |
Vertical band of tissue anterior to the lumbar vertebrae and anchoring all of the small intestine except the initial portion (the duodenum) |
|
Mesocolon |
Attaches two portions of the large intestine (the transverse and sigmoid colon) to the posterior abdominal wall |
INTERACTIVE ACTIVITY
Explore the image panels of the Peritoneum. This activity requires you to move from one slide to the next. You can do this by clicking either the arrowsbeside the image, or the buttons below the image. [Created in Anatomy.TV, Primal Pictures]
Questions:
(a) Identify the part of peritoneum that lines the abdominal wall.
(b) What is the term used to describe organs that are enveloped in visceral peritoneum?
The Stomach
Learning Objectives
By the end of this section, you will be able to:
- Label on a diagram the main regions of the stomach
The stomach links the oesophagus to the first part of the small intestine (the duodenum) and is relatively fixed in place at its oesophageal and duodenal ends. In between, however, it can be a highly active structure, contracting and continually changing position and size. These contractions provide mechanical assistance to digestion. The empty stomach is only about the size of your fist, but can stretch to hold as much as 4 litres of food and fluid, or more than 75 times its empty volume, and then return to its resting size when empty.
The stomach plays several important roles in chemical digestion. Foods are mixed together with digestive juices in the stomach until they are converted into chyme, which is released into the small intestine. Little if any nutrient absorption occurs in the stomach, with the exception of the negligible amount of nutrients in alcohol.
Structure
The three main regions in the stomach include the fundus, body, and pylorus (Figure 23.15). Located inferior to the thoracic diaphragm is the dome-shaped fundus. Inferior the fundus is the body, the main part of the stomach. The funnel-shaped pylorus connects the stomach to the duodenum. The smooth muscle pyloric sphincter is located distally and controls stomach emptying. In the absence of food, the stomach deflates inward, and its mucosa and submucosa fall into a large fold called a rugae.
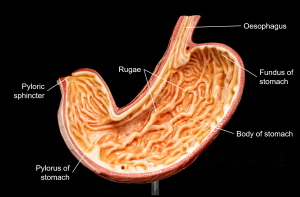
Figure 23.15 Stomach The major regions of the stomach: the fundus, body, and pylorus. The addition of an inner oblique smooth muscle layer gives the muscularis the ability to vigorously churn and mix food.
Histology
The wall of the stomach is made of the same four layers as most of the rest of the gastrointestinal tract, but with adaptations to the mucosa and muscularis externa for the unique functions of this organ. In addition to the typical circular and longitudinal smooth muscle layers, the muscularis externa has an inner oblique smooth muscle layer (Figure 23.16). As a result, in addition to moving food through the canal, the stomach can vigorously churn food, mechanically breaking it down into smaller particles. The stomach mucosa’s epithelial lining consists only of surface mucus cells, which secrete a protective coat of alkaline mucus to protect against self-digestion. A vast number of gastric pits are located along the surface of the epithelium.
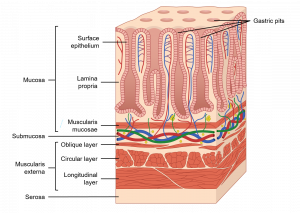
Figure 23.16 Histology of the Stomach The stomach wall is adapted for the functions of the stomach. In the epithelium, gastric pits lead to gastric glands that secrete gastric juice. [Adapted from Collectivedogs, CC BY-SA 4.0 <https://creativecommons.org/licenses/by-sa/4.0>, via Wikimedia Commons]
INTERACTIVE LINK
The Small and Large Intestines
Learning Objectives
By the end of this section, you will be able to:
- Compare and contrast the location and gross anatomy of the small and large intestines
- Identify three main adaptations of the small intestine wall that increase its absorptive capacity
- Trace the pathway of food waste from its point of entry into the large intestine through its exit from the body as faeces
The word intestine is derived from a Latin root meaning “internal,” and indeed, the two organs together nearly fill the interior of the abdominal cavity. In addition, called the small and large intestine, they constitute the greatest mass and length of the gastrointestinal tract and, with the exception of ingestion, perform all digestive system functions.
The Small Intestine
Structure
The coiled tube of the small intestine is subdivided into three regions. From proximal (at the stomach) to distal, these are the duodenum, jejunum, and ileum.
The shortest region is the 25 cm duodenum, which begins at the pyloric sphincter. Just past the pyloric sphincter, it bends posteriorly behind the peritoneum, becoming retroperitoneal, and then makes a C-shaped curve around the head of the pancreas before ascending anteriorly again to return to the peritoneal cavity and join the jejunum.
Of particular interest is the hepatopancreatic ampulla. Located in the duodenal wall, the ampulla marks the transition from the anterior portion of the gastrointestinal tract to the mid-region, and is where the common bile duct (through which bile passes from the liver) and the main pancreatic duct (through which pancreatic juice passes from the pancreas) join. This ampulla opens into the duodenum at a tiny volcano-shaped structure called the major duodenal papilla.
The jejunum is about 0.9 metres long (in life) and runs from the duodenum to the ileum. No clear demarcation exists between the jejunum and the final segment of the small intestine, the ileum.
The ileum is the longest part of the small intestine, measuring about 1.8 metres in length. The ileum joins the caecum, the first portion of the large intestine, at the ileocaecal sphincter (or valve). The jejunum and ileum are tethered to the posterior abdominal wall by the mesentery. The large intestine frames these three parts of the small intestine.
INTERACTIVE ACTIVITY
Explore the image panels of the Regions of the Small Intestine. This activity requires you to move from one slide to the next. You can do this by clicking either the arrows beside the image, or the buttons below the image. [Created in Anatomy.TV, Primal Pictures]
The duodenum is the first and shortest part of the small intestine [1st panel]. The jejunum is the middle part of the small intestine [2nd panel]. The ileum is the most distal (last) part of the small intestine [3rd panel].
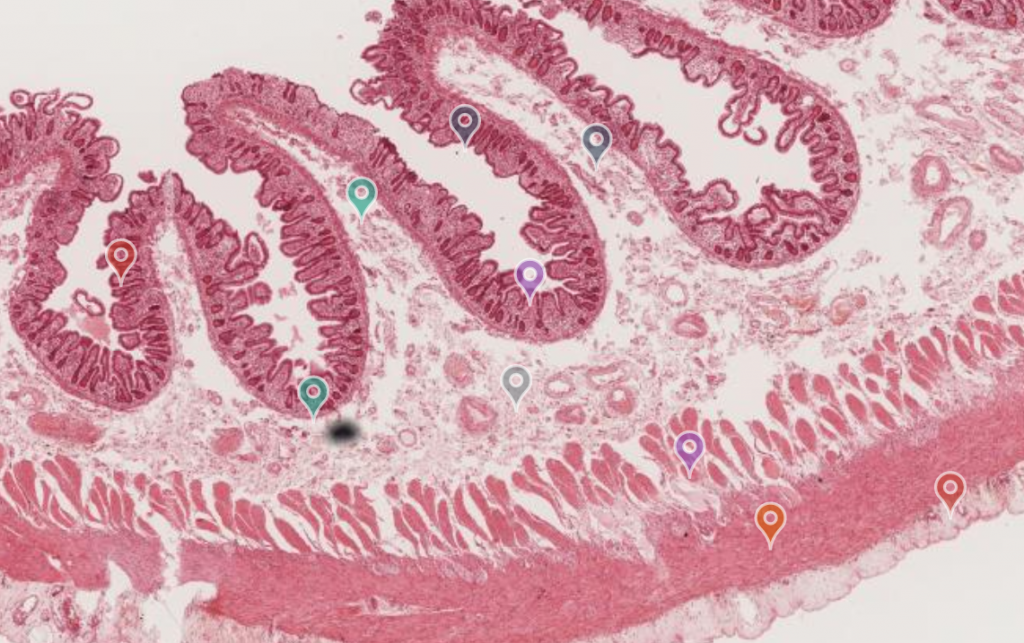
Histology
The wall of the small intestine is composed of the same four layers typically present in the gastrointestinal system. However, three features of the mucosa and submucosa are unique. These features, which increase the absorptive surface area of the small intestine more than 600-fold, include plicae circulares (circular folds), villi, and microvilli (Figure 23.19). These adaptations are most abundant in the proximal two-thirds of the small intestine, where the majority of absorption occurs.
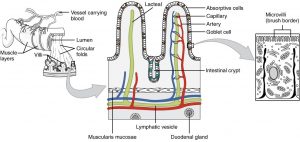
Figure 23.19 Histology of the Small Intestine The absorptive surface of the small intestine is vastly enlarged by the presence of circular folds, villi, and microvilli.
Plicae circulares
A plicae circulare (circular fold) is a deep ridge in the mucosa and submucosa. Beginning near the proximal part of the duodenum and ending near the middle of the ileum, these folds facilitate absorption. Their shape causes the chyme to spiral, rather than move in a straight line, through the small intestine. Spiraling slows the movement of chyme and provides the time needed for nutrients to be fully absorbed (Figure XX).
Villi
Within the plicae circulare are small (0.5–1 mm long) hairlike vascularised projections called villi (singular = villus). There are about 20 to 40 villi per square millimetre, increasing the surface area of the epithelium tremendously. The mucosal epithelium, primarily composed of absorptive cells, covers the villi. In addition to muscle and connective tissue to support its structure, each villus contains a capillary bed composed of one arteriole and one venule, as well as a lymphatic capillary called a lacteal. The breakdown products of carbohydrates and proteins (sugars and amino acids) can enter the bloodstream directly, but lipid breakdown products are absorbed by the lacteals and transported to the bloodstream via the lymphatic system (Figure XX).
Microvilli
As their name suggests, microvilli (singular = microvillus) are much smaller (1 µm) than villi. They are cylindrical apical surface extensions of the plasma membrane of the mucosa’s epithelial cells that greatly expand the surface area of the plasma membrane and thus greatly enhance absorption. Although their small size makes it difficult to see each microvillus, their combined microscopic appearance suggests a mass of bristles, which is termed the brush border (Figure XX).
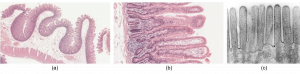
Figure XX Micrographs of the Small Intestine (a) Micrograph of the plicae circulares (circular folds). (b) Micrograph of the villi. (c) Electron micrograph of the microvilli. From left to right, LM x 56, LM x 508, EM x 196,000. [Micrographs provided by the Regents of University of Michigan Medical School © 2012]
INTERACTIVE LINK
INTERACTIVE ACTIVITY
Histological Layers of the Small Intestine. Learn more about the histology of the wall of the small intestine by clicking on each information hotspot.
The Large Intestine
The large intestine is the terminal part of the gastrointestinal tract. The primary function of this organ is to absorb water, synthesise certain vitamins, form faeces, and eliminate faeces from the body.
Structure
The large intestine runs from the vermiform appendix to the anus. It frames the small intestine on three sides. Despite its being about one-half as long as the small intestine, it is called large because it is more than twice the diameter of the small intestine.
Subdivisions
The large intestine is subdivided into four main regions: the caecum, the colon, the rectum, and the anus. The ileocaecal sphincter, located at the opening between the ileum and the large intestine, controls the flow of chyme from the small intestine to the large intestine.
Caecum
The first part of the large intestine is the caecum, a sac-like structure that is suspended inferior to the ileocaecal valve. It is about 6 cm long, receives the contents of the ileum, and continues the absorption of water and salts. The vermiform appendix is a winding tube that attaches to the caecum.
Colon
The caecum is continuous with the colon. Upon entering the colon, the food residue first travels up the ascending colon on the right side of the abdomen. At the inferior surface of the liver, the colon bends to form the hepatic flexure (right colic flexure) and becomes the transverse colon. Food residue passing through the transverse colon travels across to the left side of the abdomen, where the colon angles sharply immediately inferior to the spleen, at the splenic flexure (left colic flexure). From there, food residue passes through the descending colon, which runs down the left side of the posterior abdominal wall. After entering the pelvis inferiorly, it becomes the s-shaped sigmoid colon, which extends medially to the midline. The ascending and descending colon, and the rectum are located in the retroperitoneum. The transverse and sigmoid colon are tethered to the posterior abdominal wall by the mesocolon.
Rectum
Food residue leaving the sigmoid colon enters the rectum in the pelvis. The final 20 cm of the gastrointestinal tract, the rectum extends anterior to the sacrum and coccyx.
Anal Canal
Finally, food residue reaches the last part of the large intestine, the anal canal, which is located in the perineum, completely outside of the abdominopelvic cavity. This 4–5 cm long structure opens to the exterior of the body at the anus. The anal canal includes two sphincters. The internal anal sphincter is made of smooth muscle, and its contractions are involuntary. The external anal sphincter is made of skeletal muscle, which is under voluntary control. Except when defecating, both usually remain closed.
INTERACTIVE ACTIVITY
Explore the image panels of the Regions of the Large Intestine. This activity requires you to move from one slide to the next. You can do this by clicking either the arrowsbeside the image, or the buttons below the image. [Created in Anatomy.TV, Primal Pictures]
The caecum is the most proximal part of the large intestine [1st panel]. The ascending colon ascends on the right side of the abdomen [2nd panel]. The transverse colon typically travels horizontally across the abdomen however can vary in position [3rd panel]. The descending colon descends on the left side of the abdomen [4th panel]. The sigmoid colon forms an s-shape and enters the pelvis [5th panel]. The rectum and anal canal are the most distal parts of the large intestine [6th panel].
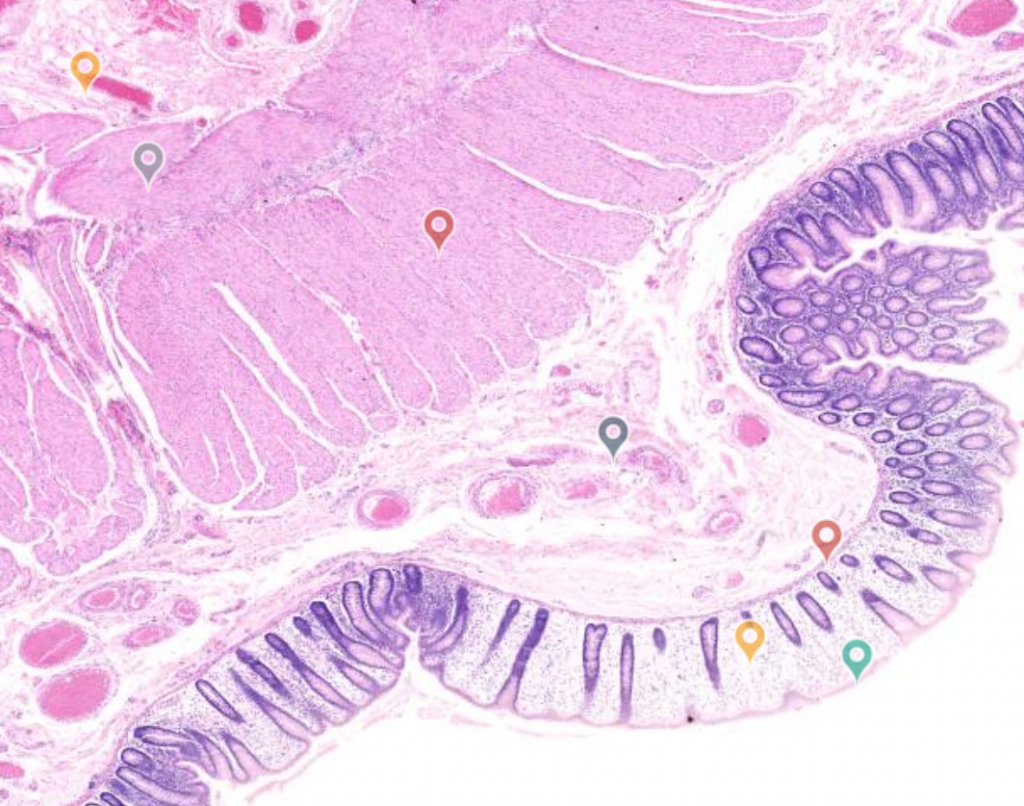
Histology
There are several notable differences between the walls of the large and small intestines (Figure 23.22). For example, there are no plicae circulares or villi. Other than in the anal canal, the mucosa of the colon is simple columnar epithelium and goblet cells. The goblet cells secrete mucus that eases the movement of faeces and protects the intestine from the effects of the acids and gases produced by enteric bacteria. The epithelia absorbs water and salts as well as vitamins produced by the intestinal bacteria.
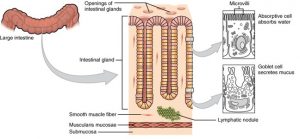
Figure 23.22 Histology of the large Intestine The histologies of the large intestine and small intestine are adapted for the digestive functions of each organ.
INTERACTIVE LINK
Anatomy
Three features are unique to the large intestine: teniae coli, haustra, and epiploic appendages (Figure 23.23). The teniae coli are three bands of smooth muscle that make up the longitudinal muscle layer of the muscularis of the large intestine, except at its terminal end. Tonic contractions of the teniae coli bunch up the colon into a succession of pouches called haustra (singular = haustrum), which are responsible for the wrinkled appearance of the colon. Attached to the teniae coli are small, fat-filled sacs of visceral peritoneum called epiploic appendages. The purpose of these is unknown. Although the rectum and anal canal have neither teniae coli nor haustra, they do have well-developed layers of muscularis that create the strong contractions needed for defecation.
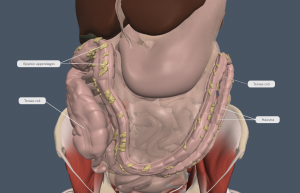
Figure 23.23 Teniae Coli, Haustra, and Epiploic Appendages [Created in Anatomy.TV, Primal Pictures]
The stratified squamous epithelial mucosa of the anal canal connects to the skin on the outside of the anus. This mucosa varies considerably from that of the rest of the colon to accommodate the high level of abrasion as faeces pass through.
Table 23.3 Functions of the Digestive Organs
|
Organ |
Major functions |
Other functions |
|
Mouth |
Ingests food Chews and mixes food Begins chemical breakdown of food Moves food into the pharynx |
Moistens and dissolves food, allowing you to taste it Cleans and lubricates the teeth and oral cavity Has some antimicrobial activity |
|
Pharynx |
Propels food from the oral cavity to the oesophagus |
Lubricates food and passageways |
|
Oesophagus |
Propels food to the stomach |
Lubricates food and passageways |
|
Stomach |
Mixes and churns food with gastric juices to form chyme Continues chemical breakdown of food Releases food into the duodenum as chyme Absorbs some fat-soluble substances (for example, alcohol, aspirin) Possesses antimicrobial functions |
Stimulates digesting enzymes Secretes intrinsic factor required for vitamin B12 absorption in small intestine |
|
Small intestine |
Mixes chyme with digestive juices Propels food at a rate slow enough for digestion and absorption Absorbs breakdown products of carbohydrates, proteins, lipids, and nucleic acids, along with vitamins, minerals, and water Performs physical digestion via segmentation |
Provides optimal medium for enzymatic activity |
|
Accessory organs |
Liver: produces bile salts, which emulsify lipids, aiding their digestion and absorption Gallbladder: stores, concentrates, and releases bile Pancreas: produces digestive enzymes and bicarbonate
|
Bicarbonate-rich pancreatic juices help neutralize acidic chyme and provide optimal environment for enzymatic activity |
|
Large intestine |
Absorbs most residual water, electrolytes, and vitamins produced by enteric bacteria Propels faeces toward rectum Eliminates faeces
|
Food residue is concentrated and temporarily stored prior to defecation Mucus eases passage of faeces through colon
|
Accessory Organs in Digestion: The Pancreas, Liver, and Gallbladder
Learning Objectives
By the end of this section, you will be able to:
- Describe the anatomy of the liver, pancreas, and gallbladder
Chemical digestion in the small intestine relies on the activities of three accessory digestive organs: the liver, pancreas, and gallbladder (Figure 23.24). The digestive role of the liver is to produce bile and export it to the duodenum. The gallbladder primarily stores, concentrates, and releases bile. The pancreas produces pancreatic juice, which contains digestive enzymes and bicarbonate ions, and delivers it to the duodenum.
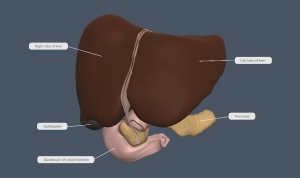
Figure 23.24 Accessory Organs The liver, pancreas, and gallbladder are considered accessory digestive organs, but their roles in the digestive system are vital. [Created in Anatomy.TV, Primal Pictures]
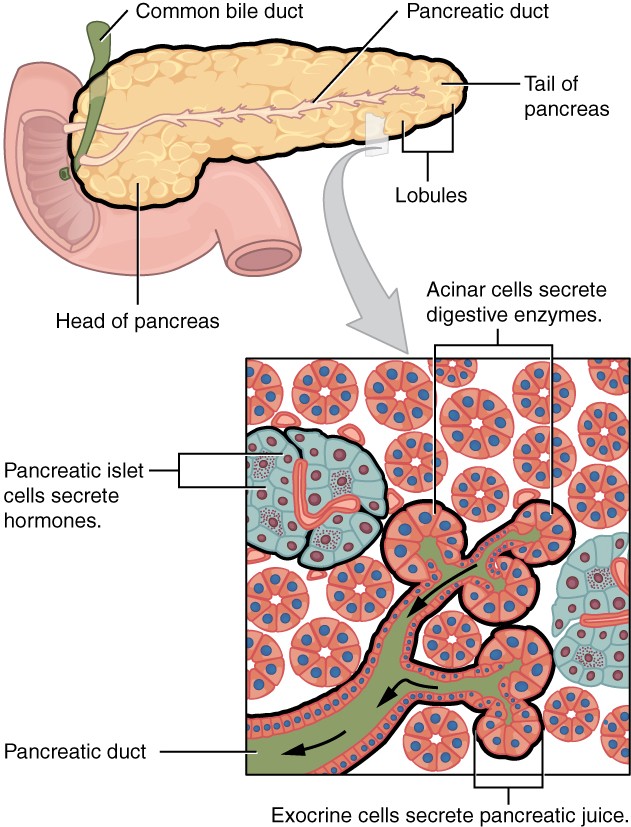
The Pancreas
The soft, glandular pancreas lies transversely in the retroperitoneum posterior to the stomach. the head is located in the “c-shaped” curvature of the duodenum with the body extending to the left and ending as a tapering tail in the hilum of the spleen. The pancreas performs both exocrine (secreting digestive enzymes) and endocrine (releasing hormones into the blood) functions (Figure 23.26).
Figure 23.26 Exocrine and Endocrine Pancreas The pancreas has a head, a body, and a tail. It delivers pancreatic juice to the duodenum through the pancreatic duct.
The exocrine part of the pancreas arises as little grape-like cell clusters, each called an acinus (plural = acini), located at the terminal ends of pancreatic ducts. The main pancreatic duct fuses with the common bile duct (carrying bile from the liver and gallbladder) just before entering the duodenum via a common opening (the hepatopancreatic ampulla). A second and smaller pancreatic duct, the accessory pancreatic duct, runs from the pancreas directly into the duodenum, superior the hepatopancreatic ampulla.
Small patches of pancreatic islet cells, produce the hormones with endocrine function.
The Liver
The liver is the largest gland in the body. It is also one of the most important organs, producing bile, to accomplish the emulsification of lipids in the small intestine. In addition to being an accessory digestive organ, it plays a number of roles in metabolism and regulation. The liver lies inferior to the thoracic diaphragm in the right upper quadrant of the abdominal cavity and receives protection from the surrounding ribs.
The liver is divided into two primary lobes: a large right lobe and a smaller left lobe. The falciform ligament is a remnant of the umbilical vein, and separates the right and left lobes anteriorly.
The porta hepatis (“gate to the liver”) is where the hepatic artery proper and hepatic portal vein enter the liver, and the hepatic ducts exits the liver. As shown in Figure XX, the hepatic artery proper delivers oxygenated blood to the liver. The hepatic portal vein delivers partially deoxygenated blood containing nutrients absorbed from the small intestine and actually supplies more oxygen to the liver than do the much smaller hepatic arteries. In addition to nutrients, drugs and toxins are also absorbed. After processing the bloodborne nutrients and toxins, the liver releases nutrients needed by other cells back into the blood, which drains into the hepatic vein to the inferior vena cava. With this hepatic portal circulation, all blood from the gastrointestinal tract passes through the liver.
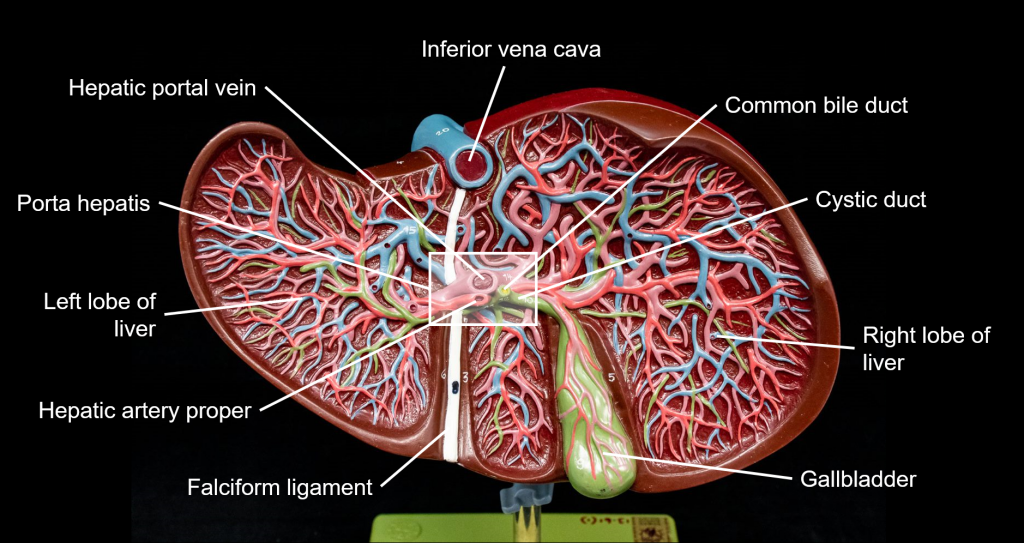
Figure XX The Liver The porta hepatis is considered the gateway to the liver, and contains the hepatic portal vein, the hepatic artery proper and the hepatic ducts.
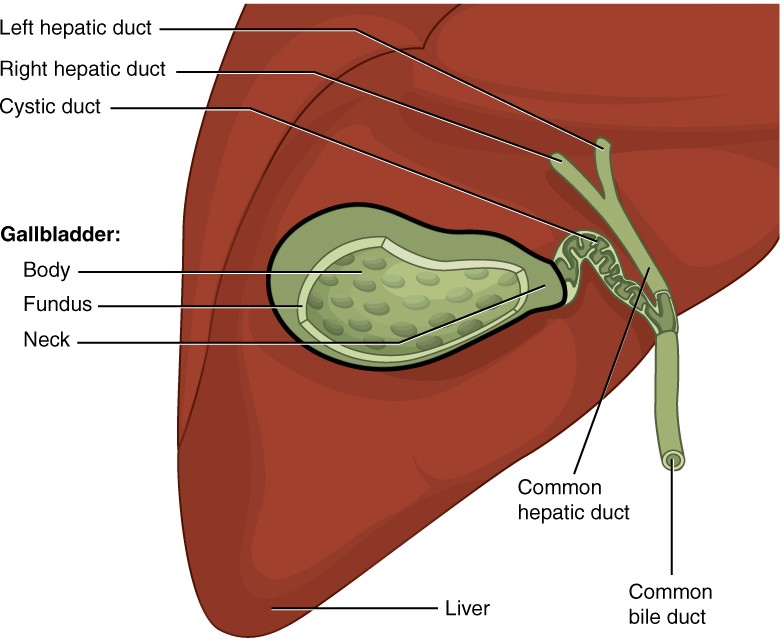
The Gallbladder
The gallbladder is 8–10 cm long and is located on the posterior aspect of the right lobe of the liver. This muscular sac stores, concentrates, and, when stimulated, propels the bile into the duodenum via the common bile duct. The fundus is the widest portion and tapers medially into the body, which in turn narrows to become the neck. The neck angles slightly superiorly as it approaches the hepatic duct. The cystic duct is 1–2 cm long and turns inferiorly as it bridges the neck and hepatic duct.
The simple columnar epithelium of the gallbladder mucosa is organised in rugae, similar to those of the stomach. The gallbladder’s contents are ejected through the cystic duct and into the common bile duct.
Biliary System
In order for bile to reach the duodenum of the small intestine, it travels through a series of ducts. The liver releases bile into either a right or left hepatic duct, which unite to form the common hepatic duct. The bile then travels to the gallbladder via the cystic duct. The cystic duct and common hepatic duct unite to become the common bile duct, which then joins with the main pancreatic duct to form the hepatopancreatic ampulla (which projects through the wall of the duodenum) (Figure XX).
Figure XX Gallbladder The gallbladder stores and concentrates bile, and releases it into the two-way cystic duct when it is needed by the small intestine.
INTERACTIVE ACTIVITY
Key Terms
absorption passage of digested products from the intestinal lumen through mucosal cells and into the bloodstream or lacteals
accessory digestive organ includes teeth, tongue, salivary glands, gallbladder, liver, and pancreas
accessory duct (also, duct of Santorini) duct that runs from the pancreas into the duodenum
acinus cluster of glandular epithelial cells in the pancreas that secretes pancreatic juice in the pancreas
anal canal final segment of the large intestine
ascending colon first region of the colon
bacterial flora bacteria in the large intestine
bile alkaline solution produced by the liver and important for the emulsification of lipids
body mid-portion of the stomach
bolus mass of chewed food
brush border fuzzy appearance of the small intestinal mucosa created by microvilli
caecum pouch forming the beginning of the large intestine
canine (also, cuspid) pointed tooth used for tearing and shredding food
chemical digestion enzymatic breakdown of food
chyme soupy liquid created when food is mixed with digestive juices
colon part of the large intestine between the cecum and the rectum
common bile duct structure formed by the union of the common hepatic duct and the cystic duct of the gallbladder
common hepatic duct duct formed by the mergeing of the two hepatic ducts
cystic duct duct through which bile drains and enters the gallbladder
deciduous tooth one of 20 “baby teeth”
defecation elimination of undigested substances from the body in the form of faeces
deglutition three-stage process of swallowing
dentition set of teeth
descending colon part of the colon between the transverse colon and the sigmoid colon
duodenum first part of the small intestine, which starts at the pyloric sphincter and ends at the jejunum
epiploic appendage small sac of fat-filled visceral peritoneum attached to teniae coli
external anal sphincter voluntary skeletal muscle sphincter in the anal canal
faeces semisolid waste product of digestion
fundus dome-shaped region of the stomach
gallbladder accessory digestive organ that stores and concentrates bile
gastric gland gland in the stomach mucosal epithelium that produces gastric juice
gastric pit narrow channel formed by the epithelial lining of the stomach mucosa
gastrointestinal (GI) tract continuous muscular digestive tube that extends from the mouth to the anus
haustrum small pouch in the colon created by tonic contractions of teniae coli
hepatic artery proper artery that supplies oxygenated blood to the liver
hepatic flexure (right colic flexure) point, at the inferior surface of the liver, where the ascending colon turns abruptly to the left
hepatic portal vein vein that supplies deoxygenated nutrient-rich blood to the liver
hepatic vein vein that drains into the inferior vena cava
hepatopancreatic ampulla bulb-like point in the wall of the duodenum where the common bile duct and main pancreatic duct unite
ileocaecal sphincter sphincter located where the small intestine joins with the large intestine
ileum end of the small intestine between the jejunum and the large intestine
incisor midline, chisel-shaped tooth used for cutting into food
ingestion taking food into the GI tract through the mouth
internal anal sphincter involuntary smooth muscle sphincter in the anal canal
intrinsic factor glycoprotein required for vitamin B12 absorption in the small intestine
jejunum middle part of the small intestine between the duodenum and the ileum
lacteal lymphatic capillary in the villi
large intestine terminal portion of the gastrointestinal tract
laryngopharynx part of the pharynx that functions in respiration and digestion
liver largest gland in the body whose main digestive function is the production of bile
main pancreatic duct duct through which pancreatic juice drains from the pancreas
major duodenal papilla point at which the hepatopancreatic ampulla opens into the duodenum
mastication chewing
mechanical digestion chewing, mixing, and segmentation that prepares food for chemical digestion
microvillus small projection of the plasma membrane of the absorptive cells of the small intestinal mucosa
molar tooth used for crushing and grinding food
mucosa innermost lining of the gastrointestinal tract
muscularis muscle (skeletal or smooth) layer of the gastrointestinal wall
oesophagus muscular tube that runs from the pharynx to the stomach
oral cavity (also, buccal cavity) mouth
oropharynx part of the pharynx continuous with the oral cavity that functions in respiration and digestion
pancreas accessory digestive organ that secretes pancreatic juice
pancreatic juice secretion of the pancreas containing digestive enzymes and bicarbonate
parotid gland one of a pair of major salivary glands located inferior and anterior to the ears
peristalsis muscular contractions and relaxations that propel food through the GI tract
permanent tooth one of 32 adult teeth
pharynx throat
plicae circulares (also, circular folds) deep folds in the mucosa and submucosa of the small intestine
porta hepatis “gateway to the liver” where the hepatic artery proper and hepatic portal vein enter the liver
premolar (also, bicuspid) transitional tooth used for mastication, crushing, and grinding food
propulsion voluntary process of swallowing and the involuntary process of peristalsis that moves food through the digestive tract
pyloric sphincter sphincter that controls stomach emptying
pylorus lower, funnel-shaped part of the stomach that is continuous with the duodenum
rectum part of the large intestine between the sigmoid colon and anal canal
retroperitoneal located posterior to the peritoneum
rugae folds of gastrointestinal mucosa and submucosa in the empty stomach and other organs
saliva aqueous solution of proteins and ions secreted into the mouth by the salivary glands
salivary gland an exocrine gland that secretes a digestive fluid called saliva
segmentation alternating contractions and relaxations of non-adjacent segments of the intestine that move food forward and backward, breaking it apart and mixing it with digestive juices
serosa outermost layer of the alimentary canal wall present in regions within the abdominal cavity
sigmoid colon end portion of the colon, which terminates at the rectum
small intestine section of the alimentary canal where most digestion and absorption occurs
soft palate posterior region of the bottom portion of the nasal cavity that consists of skeletal muscle
splenic flexure (also left colic flexure) point where the transverse colon curves below the inferior end of the spleen
stomach gastrointestinal tract organ that contributes to chemical and mechanical digestion of food from the oesophagus before releasing it, as chyme, to the small intestine
sublingual gland one of a pair of major salivary glands located beneath the tongue
submandibular gland one of a pair of major salivary glands located in the floor of the mouth
submucosa layer of dense connective tissue in the alimentary canal wall that binds the overlying mucosa to the underlying muscularis
submucosal plexus (plexus of Meissner) nerve supply that regulates activity of glands and smooth muscle
tenia coli one of three smooth muscle bands that make up the longitudinal muscle layer of the muscularis in all of the large intestine except the terminal end
tongue accessory digestive organ of the mouth, the bulk of which is composed of skeletal muscle
transverse colon part of the colon between the ascending colon and the descending colon
vermiform appendix coiled tube attached to the caecum
villus projection of the mucosa of the small intestine