Chapter 16: URINARY SYSTEM
Introduction

Bladder Calculus (stone) The large circular structure located in the urinary bladder in this radiograph is an example of a bladder calculus (stone). Urinary calculi can form in the urinary bladder, or can occur from migrated renal calculi (kidney stones). [Case courtesy of Dr Aditya Shetty, Radiopaedia.org, rID: 27089]
Chapter Objectives
After studying this chapter, you will be able to:
- Label structures of the urinary system
- Characterise the roles of each of the parts of the urinary system
- Illustrate the macroscopic and microscopic structures of the kidney
- Outline how blood is filtered in the kidney nephron
The urinary system’s ability to filter the blood resides in about 2 to 3 million tufts of specialised capillaries—the glomeruli—distributed more or less equally between the two kidneys. Because the glomeruli filter the blood based mostly on particle size, large elements like blood cells and platelets are excluded. The glomerulus is the first part of the nephron, which then continues as a highly specialised tubular structure responsible for creating the final urine composition. All other solutes, such as amino acids, vitamins, and wastes, are filtered to create a filtrate composition very similar to plasma. The glomeruli create about 200 litres of this filtrate every day, yet you excrete less than two litres of waste you call urine.
Gross Anatomy of the Kidney
Learning Objectives
By the end of this section, you will be able to:
- Describe the external structure of the kidney, including its location, support structures, and covering
- Identify the major internal divisions and structures of the kidney
- Name structures found in the cortex and medulla
The kidneys are located on either side of the vertebral column in the retroperitoneal space between the parietal peritoneum and the posterior abdominal wall, well protected by muscle, fat, and ribs. They are roughly the size of your fist, and the male kidney is typically a bit larger than the female kidney.
External Anatomy
The right kidney is slightly more inferior than the left kidney due to displacement by the liver. Superior portions of the kidneys are somewhat protected by the eleventh and twelfth ribs (Figure 25.7). They are about 11–14 cm in length, 6 cm wide, and 4 cm thick, and are directly covered by a fibrous capsule composed of dense, irregular connective tissue that helps to hold their shape and protect them. This capsule is covered by a shock-absorbing layer of adipose tissue called perirenal fat, which in turn is encompassed by a tough renal fascia. The fascia and, to a lesser extent, the overlying peritoneum serve to firmly anchor the kidneys to the posterior abdominal wall in a retroperitoneal position.
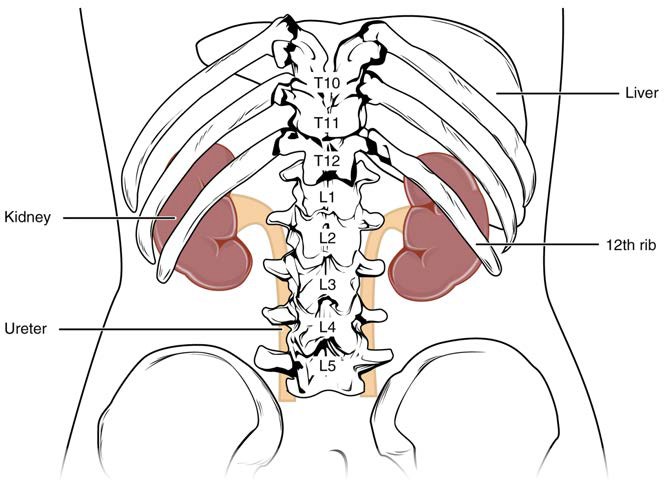
Figure 25.7 Kidneys The kidneys are slightly protected by the ribs and are surrounded by fat for protection (not shown).
On the superior aspect of each kidney is the adrenal gland (suprarenal gland). The adrenal cortex directly influences renal function through the production of the hormone aldosterone to stimulate sodium reabsorption.
Renal Hilum
The renal hilum is the entry and exit site for structures servicing the kidneys: vessels, nerves, lymphatics, and ureters. The medial-facing hila are tucked into the sweeping convex outline of the cortex. Emerging from the hilum is the renal pelvis, which is formed from the major and minor calyces in the kidney. The smooth muscle in the renal pelvis funnels urine via peristalsis into the ureter. The renal arteries are collateral branches of the descending abdominal aorta, whereas the renal veins are tributaries to the inferior vena cava. The artery, vein, and renal pelvis are arranged in an anterior-to-posterior order (Figure 25.8).
Internal Anatomy
A frontal section through the kidney reveals an outer region called the renal cortex and an inner region called the medulla (Figure 25.8). The renal columns are connective tissue extensions that radiate downward from the cortex through the medulla to separate the most characteristic features of the medulla, the renal pyramids and renal papillae. The papillae are bundles of collecting ducts that transport urine made by nephrons to the calyces of the kidney for excretion. The renal columns also serve to divide the kidney into 6–8 lobes and provide a supportive framework for vessels that enter and exit the cortex. The pyramids and renal columns taken together constitute the kidney lobes.
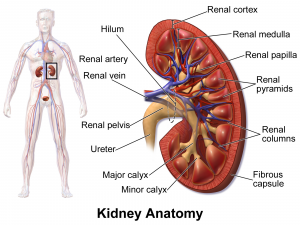
Figure 25.8 Left Kidney The internal anatomy of the kidney consists of a renal cortex and renal medulla. [Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010.]
Microscopic Anatomy of the Kidney
Learning Objectives
By the end of this section, you will be able to:
- Describe the structure of the filtration membrane
- Identify the major structures and subdivisions of the renal corpuscles, renal tubules, and renal capillaries
- Describe the histology of the proximal convoluted tubule, loop of Henle, distal convoluted tubule, and collecting ducts
The renal structures that conduct the essential work of the kidney cannot be seen by the naked eye. Only a light or electron microscope can reveal these structures. Even then, serial sections and computer reconstruction are necessary to give us a comprehensive view of the functional anatomy of the nephron and its associated blood vessels.
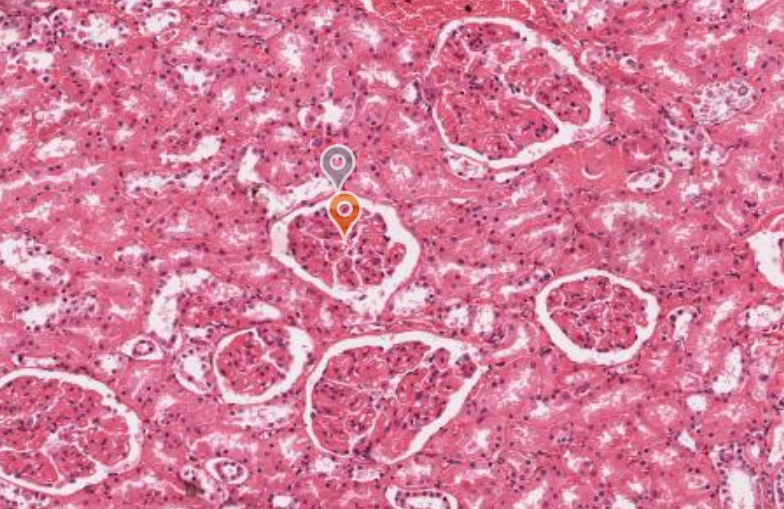
Nephrons and Vessels
Nephrons are the “functional units” of the kidney; they cleanse the blood and balance the constituents of the circulation. The afferent arterioles form a tuft of high-pressure capillaries about 200 µm in diameter, the glomerulus. The rest of the nephron consists of a continuous sophisticated tubule where the proximal end surrounds the glomerulus—this is the Bowman’s capsule (glomerular capsule). The glomerulus and Bowman’s capsule together form the renal corpuscle. These glomerular capillaries filter the blood based on particle size. After passing through the renal corpuscle, the capillaries form a second arteriole, the efferent arteriole. As the glomerular filtrate progresses through the nephron, capillary networks recover most of the solutes and water, and return them to the circulation.
Renal Cortex
In a dissected kidney, it is easy to identify the cortex; it appears lighter in colour compared to the rest of the kidney.
All of the renal corpuscles as well as both the proximal convoluted tubules (PCTs) and distal convoluted tubules (DCTs) are located here. Some nephrons have a short loop of Henle (nephron loop) that does not dip beyond the cortex, about 15% of nephrons have long loops of Henle that extend deep into the medulla.
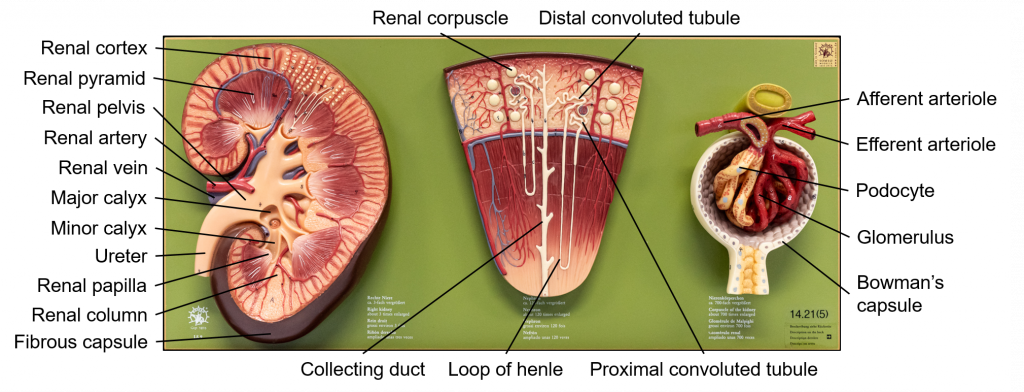
Figure XX Kidney From left to right: macroscopic kidney, anatomy of the nephron and a renal corpuscle.
Nephrons: The Functional Unit
Nephrons take a simple filtrate of the blood and modify it into urine. Many changes take place in the different parts of the nephron before urine is created for disposal. The principle task of the nephron population is to balance the plasma to homeostatic set points and excrete potential toxins in the urine. They do this by accomplishing three principle functions—filtration, reabsorption, and secretion.
Renal Corpuscle
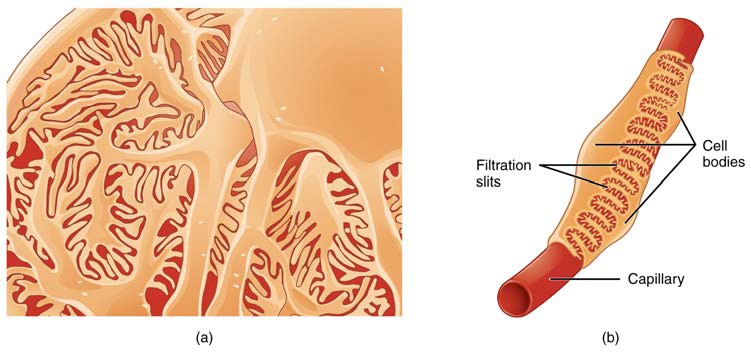
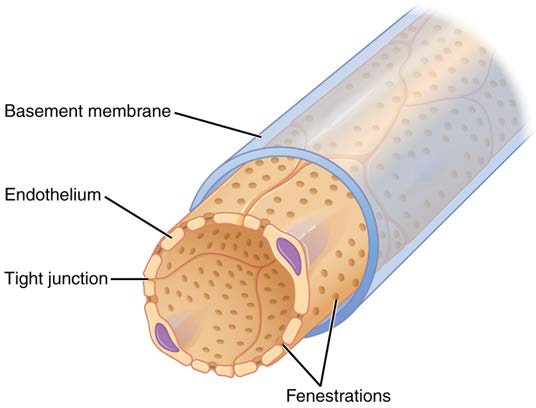
As discussed earlier, the renal corpuscle consists of a tuft of capillaries called the glomerulus that is largely surrounded by Bowman’s (glomerular) capsule. The glomerulus is a high-pressure capillary bed between afferent and efferent arterioles. Bowman’s capsule surrounds the glomerulus to form a lumen, and captures and directs this filtrate to the proximal convoluted tubule (PCT). The outermost part of Bowman’s capsule, the parietal layer, is a simple squamous epithelium. It transitions onto the glomerular capillaries to form the visceral layer of the capsule. Here, the cells are not squamous, but uniquely shaped cells (podocytes) extending finger-like arms to cover the glomerular capillaries (Figure 25.11). These projections interdigitate to form filtration slits, leaving small gaps between the digits to form a sieve. As blood passes through the glomerulus, 10 to 20% of the plasma filters between these sieve-like fingers to be captured by Bowman’s capsule and funneled to the PCT. Where the fenestrae (windows) in the glomerular capillaries match the spaces between the podocyte “fingers,” the only thing separating the capillary lumen and the lumen of Bowman’s capsule is their shared basement membrane (Figure 25.12). These three features comprise what is known as the filtration membrane. This membrane permits very rapid movement of filtrate from capillary to capsule through pores that are only 70 nm in diameter.
The fenestrations prevent filtration of blood cells or large proteins, but allow most other constituents through.
Figure 25.11 Podocytes Podocytes interdigitate and filter substances in a way similar to fenestrations. In (a), the large cell body can be seen at the top right corner, with branches extending from the cell body. (b) This capillary has three podocytes wrapped around it.
Figure 25.12 Fenestrated Capillary Fenestrations allow many substances to diffuse from the blood based primarily on size.
Proximal Convoluted Tubule (PCT)
Filtered fluid collected by Bowman’s capsule enters into the PCT. It is called convoluted due to its tortuous path.
Loop of Henle
The descending and ascending portions of the loop of Henle (sometimes referred to as the nephron loop) are, of course, just continuations of the same tubule. They run adjacent and parallel to each other after having made a hairpin turn at the deepest point of their descent. The descending loop of Henle consists of an initial short, thick portion and long, thin portion, whereas the ascending loop consists of an initial short, thin portion followed by a long, thick portion.
Distal Convoluted Tubule (DCT)
The DCT, like the PCT, is very tortuous, but it is shorter than the PCT.
Collecting Ducts
The collecting ducts are continuous with the nephron but not technically part of it. In fact, each collecting duct collects filtrate from several nephrons for final modification. Collecting ducts merge as they descend deeper in the medulla to form about 30 terminal ducts, which empty at a renal papilla.
INTERACTIVE LINK
Gross Anatomy of Urine Transport
Learning Objectives
By the end of this section, you will be able to:
- Identify the ureters, urinary bladder, and urethra, as well as their location, structure, and function
- Compare and contrast male and female urethras
Urine is a fluid of variable composition that requires specialised structures to remove it from the body safely and efficiently. Blood is filtered, and the filtrate is transformed into urine at a relatively constant rate throughout the day. This processed liquid is stored until a convenient time for excretion. All structures involved in the transport and storage of the urine are large enough to be visible to the naked eye. This transport and storage system not only stores the waste, but it protects the tissues from damage, prevents infection by foreign organisms, and for the male, provides reproductive functions.
Ureters
The kidneys and ureters are retroperitoneal. As urine is formed, it drains into the calyces of the kidney, which merge to form the funnel-shaped renal pelvis in the hilum of each kidney. The renal pelvis narrows to become the ureter of each kidney. As urine passes through the ureter, it does not passively drain into the urinary bladder but rather is propelled by waves of peristalsis. As the ureters enter the pelvis, they sweep laterally, hugging the pelvic walls. As they approach the urinary bladder, they turn medially and enter the bladder wall obliquely. This is important because it creates an one-way valve that allows urine into the urinary bladder but prevents reflux of urine from the urinary bladder back into the ureter (Figure XX).
The ureters are approximately 30 cm long. The inner mucosa is lined with transitional epithelium and scattered goblet cells that secrete protective mucus.
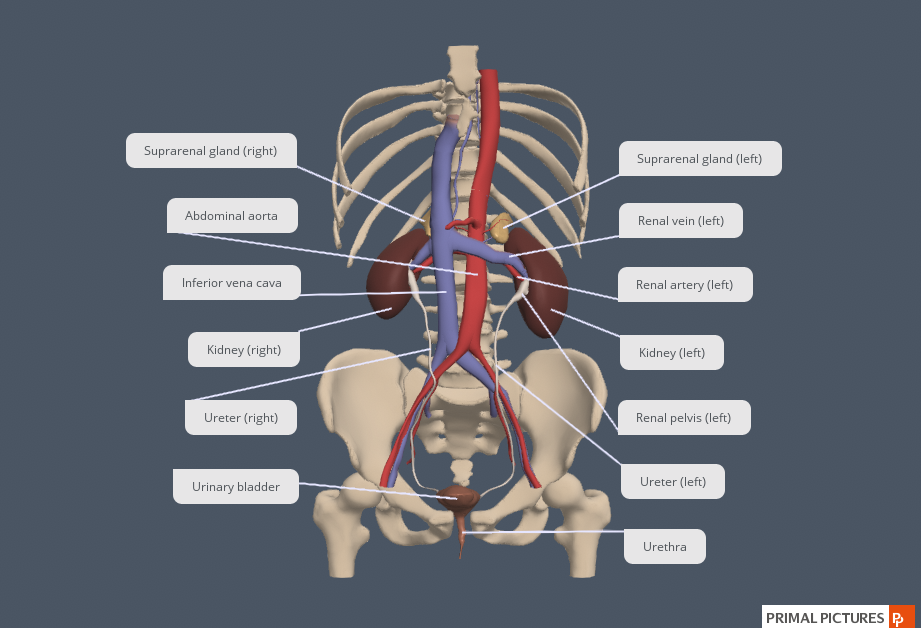
Figure XX Ureters Trace the flow of urine from the left and right kidneys via the ureters to the urinary bladder. [Created in Anatomy.TV, Primal Pictures]
INTERACTIVE ACTIVITY
This video from the QUT anatomy laboratory (3:22 minutes) demonstrates the macroscopic anatomy of the kidney including the perirenal fat, the renal cortex and renal medulla and the ureter. [Elise Pelzer, Queensland University of Technology]
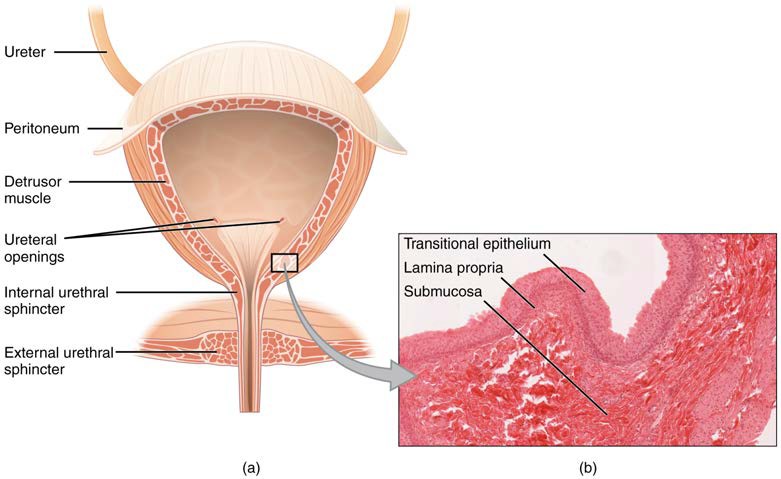
Urinary Bladder
The urinary bladder collects urine from both ureters (Figure 25.4). The urinary bladder lies anterior to the uterus in females, posterior to the pubic bone and anterior to the rectum. During late pregnancy, its capacity is reduced due to compression by the enlarging uterus, resulting in increased frequency of urination. In males, the anatomy is similar, minus the uterus, and with the addition of the prostate gland inferior to the urinary bladder.
The interior surface of the urinary bladder consists of transitional epithelium that is structurally suited for the large volume fluctuations of the bladder. When empty, it resembles columnar epithelia, but when stretched, it “transitions” (hence the name) to a squamous appearance (see Figure 25.4). Rugae (temporal mucosal folds) are also located in the urinary bladder and tend to diminish as the urinary bladder becomes distended.
Figure 25.4 Urinary Bladder (a) Anterior cross section of the urinary bladder. (b) The detrusor muscle of the bladder (source: monkey tissue) LM × 448. [Micrograph provided by the Regents of the University of Michigan Medical School © 2012]
Urethra
The urethra transports urine from the urinary bladder to the outside of the body for disposal. The urethra is the only urologic organ that shows any significant anatomic difference between males and females; all other urine transport structures are identical.
The urethra in both males and females begins inferior and central to the two ureteral openings forming the three points of a triangular-shaped area at the base of the urinary bladder called the trigone (Greek tri- = “triangle” and the root of the word “trigonometry”). The urethra is located posterior and inferior to the pubic symphysis. In both males and females, the proximal urethra is lined by transitional epithelium, whereas the terminal portion is a nonkeratinised, stratified squamous epithelium. In the male, pseudostratified columnar epithelium lines the urethra between these two cell types.
INTERACTIVE ACTIVITY
Review the major anatomical structures of the urinary system in the male pelvis model. This activity requires you to move from one slide to the next. You can do this by clicking either the arrows beside the image, or the buttons below the image to observe the unlabelled [1st panel] and labelled [2nd panel].
INTERACTIVE ACTIVITY
Review the major anatomical structures of the urinary system in the female pelvis model. This activity requires you to move from one slide to the next. You can do this by clicking either the arrows beside the image, or the buttons below the image to observe the unlabelled [1st panel] and labelled [2nd panel].
Key Terms
Bowman’s capsule cup-shaped sack lined by a simple squamous epithelium (parietal surface) and specialised cells called podocytes (visceral surface) that participate in the filtration process; receives the filtrate which then passes on to the PCTs
calyces cup-like structures receiving urine from the collecting ducts where it passes on to the renal pelvis and ureter
distal convoluted tubules portions of the nephron distal to the loop of Henle that receive hyposmotic filtrate from the loop of Henle and empty into collecting ducts
efferent arteriole arteriole carrying blood from the glomerulus to the capillary beds around the convoluted tubules and loop of Henle; portion of the portal system
external urinary sphincter skeletal muscle; must be relaxed consciously to void urine
fenestrations small windows through a cell, allowing rapid filtration based on size; formed in such a way as to allow substances to cross through a cell without mixing with cell contents
filtration slits formed by projections of podocytes; substances filter between the projections based on size
glomerulus tuft of capillaries surrounded by Bowman’s capsule; filters the blood based on size
internal urinary sphincter smooth muscle at the juncture of the bladder and urethra; relaxes as the bladder fills to allow urine into the urethra
loop of Henle descending and ascending portions between the proximal and distal convoluted tubules; those of cortical nephrons do not extend into the medulla, whereas those of juxtamedullary nephrons do extend into the medulla
nephrons functional units of the kidney that carry out all filtration and modification to produce urine; consist of renal corpuscles, proximal and distal convoluted tubules, and descending and ascending loops of Henle; drain into collecting ducts
perirenal fat adipose tissue between the renal fascia and the renal capsule that provides protective cushioning to the kidney
podocytes cells forming finger-like processes; form the visceral layer of Bowman’s capsule; pedicels of the podocytes interdigitate to form a filtration membrane
proximal convoluted tubules (PCTs) tortuous tubules receiving filtrate from Bowman’s capsule; most active part of the nephron in reabsorption and secretion
renal columns extensions of the renal cortex into the renal medulla; separates the renal pyramids; contains blood vessels and connective tissues
renal corpuscle consists of the glomerulus and Bowman’s capsule
renal cortex outer part of kidney containing all of the nephrons; some nephrons have loops of Henle extending into the medulla
renal hilum recessed medial area of the kidney through which the renal artery, renal vein, ureters, lymphatics, and nerves pass
renal medulla inner region of kidney containing the renal pyramids
renal papillae medullary area of the renal pyramids where collecting ducts empty urine into the minor calyces
renal pyramids six to eight cone-shaped tissues in the medulla of the kidney containing collecting ducts and the loops of Henle of juxtamedullary nephrons
renin enzyme produced by juxtaglomerular cells in response to decreased blood pressure or sympathetic nervous activity
retroperitoneal outside the peritoneal cavity; in the case of the kidney and ureters, between the parietal peritoneum and the abdominal wall
trigone area at the base of the bladder marked by the two ureters in the posterior–lateral aspect and the urethral orifice in the anterior aspect oriented like points on a triangle
urethra transports urine from the bladder to the outside environment