Chapter 10: INTEGUMENTARY SYSTEM
Introduction
Chapter Objectives
After studying this chapter, you will be able to:
- Describe the layers of the skin
- Describe the accessory structures of the skin
- Describe the changes that occur in the integumentary system during the aging process
What do you think when you look at your skin in the mirror? Do you think about the fact that the skin belongs to one of the body’s most essential and dynamic systems: the integumentary system? The integumentary system refers to the skin and its accessory structures, and it is responsible for much more than simply lending to your outward appearance. In the adult human body, the skin makes up about 16% of body weight and covers an area of 1.5 to 2 m2. In fact, the skin and accessory structures are the largest organ system in the human body. As such, the skin protects your inner organs and it is in need of daily care and protection to maintain its health.
Layers of the Skin
Learning Objectives
By the end of this section, you will be able to:
- Identify the components of the integumentary system
- Describe the layers of the skin
- Identify and describe the superficial and deep fascia
Although you may not typically think of the skin as an organ, it is in fact made of tissues that work together as a single structure to perform unique and critical functions. The skin and its accessory structures make up the integumentary system, which provides the body with overall protection. The skin is made of multiple layers of cells and tissues, which are held to underlying structures by connective tissue (Figure 25.2). The deeper layer of skin is well vascularised (has numerous blood vessels). It also has numerous sensory, and autonomic and sympathetic nerve fibres ensuring communication to and from the brain.
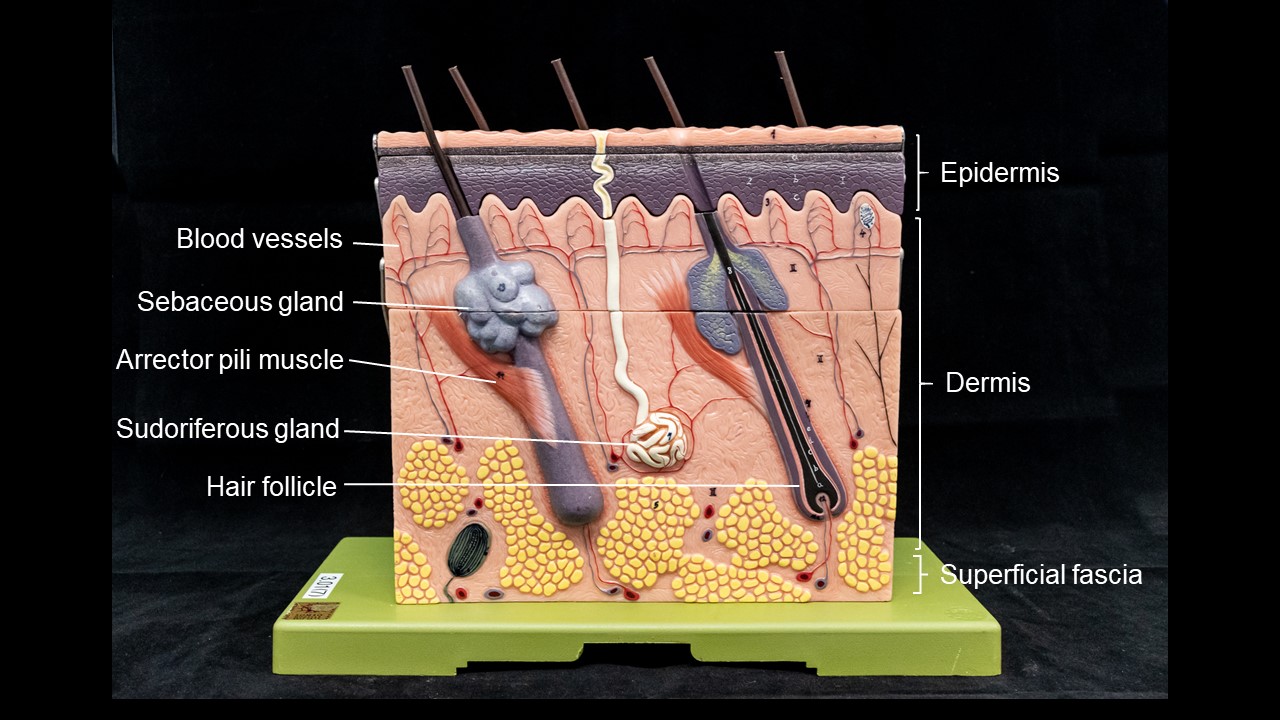
Figure 25.2 Layers of Skin The skin is composed of two main layers: the epidermis, made of closely packed epithelial cells, and the dermis, made of dense, irregular connective tissue that houses blood vessels, hair follicles, sweat glands, and other structures. Deep to the dermis lies the superficial fascia, which is composed mainly of loose connective and fatty tissues.
The Epidermis
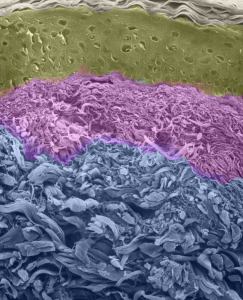
The epidermis is composed of keratinised, stratified squamous epithelium. It is made of four or five layers of epithelial cells, depending on its location in the body. It does not have any blood vessels within it (i.e., it is avascular). Skin that has four layers of cells is referred to as “thin skin (hairy skin)”. From deep to superficial, these layers are the stratum basale, stratum spinosum, stratum granulosum, and stratum corneum. Most of the skin can be classified as thin skin. “Thick skin” is found only on the palms of the hands and the soles of the feet and is hairless. It has a fifth layer, called the stratum lucidum, located between the stratum corneum and the stratum granulosum (Figure 25.5).
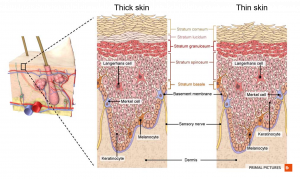
Figure 25.5 Layers of the Epidermis The epidermis of thick skin has five strata: stratum basale, stratum spinosum, stratum granulosum, stratum lucidum, and stratum corneum. Thin skin has only four strata, lacking the stratum lucidum. [Created in Anatomy.TV, Primal Pictures]
INTERACTIVE ACTIVITY
Figure 25.3 Thin Skin versus Thick Skin These slides show cross-sections of the epidermis and dermis of (a) thin and (b) thick skin. Note the significant difference in the thickness of the epithelial layer of the thick skin, LM × 40.
The cells in all of the layers except the stratum basale are called keratinocytes. A keratinocyte is a cell that manufactures and stores the protein keratin. Keratin is an intracellular fibrous protein that gives hair, nails, and skin their hardness and water-resistant properties. The keratinocytes in the stratum corneum are dead and regularly slough away, being replaced by cells from the deeper layers (Figure 25.4).
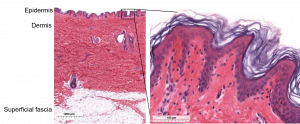
Figure 25.4 Epidermis The epidermis is epithelium composed of multiple layers of cells. The basal layer consists of cuboidal cells, whereas the superficial layers are squamous, keratinised cells, so the whole epithelium is often described as being keratinised stratified squamous epithelium. LM × 2, LM × 20. [Micrographs created in Histologyguide.com]
View the University of Michigan WebScope to explore an epithelial tissue sample in greater detail. If you zoom on the cells at the outermost layer of this section of skin, what do you notice about the cells? Webscope Integumentary system
Dermis
The dermis might be considered the “core” of the integumentary system (derma- = “skin”), as distinct from the epidermis (epi- = “upon” or “over”) and superficial fascia (hypodermis; hypo- = “below”). It contains blood and lymph vessels, nerves, and other structures, such as hair follicles and sweat glands. The dermis is made of two layers of connective tissue that compose an interconnected mesh of elastin and collagenous fibres, produced by fibroblasts (Figure 25.7).

Figure 5.7 Layers of the Dermis This stained slide shows the two components of the dermis—the papillary layer and the reticular layer. Both are made of connective tissue with fibres of collagen extending from one to the other, making the border between the two somewhat indistinct. The dermal papillae extending into the epidermis belong to the papillary layer, whereas the dense collagen fibre bundles below belong to the reticular layer. LM × 10. [credit: modification of work by “kilbad”/Wikimedia Commons]
Superficial fascia
The superficial fascia (also called the hypodermis or subcutaneous layer) is a layer deep to the dermis and serves to connect the skin to the underlying fascia (fibrous tissue) of the bones and muscles. It is not a true layer of the skin, although the border between the superficial fascia and dermis can be difficult to distinguish. The superficial fascia consists of well-vascularised, loose, areolar connective tissue and adipose tissue, which functions as a mode of fat storage and provides insulation and cushioning for the integument.
Pigmentation
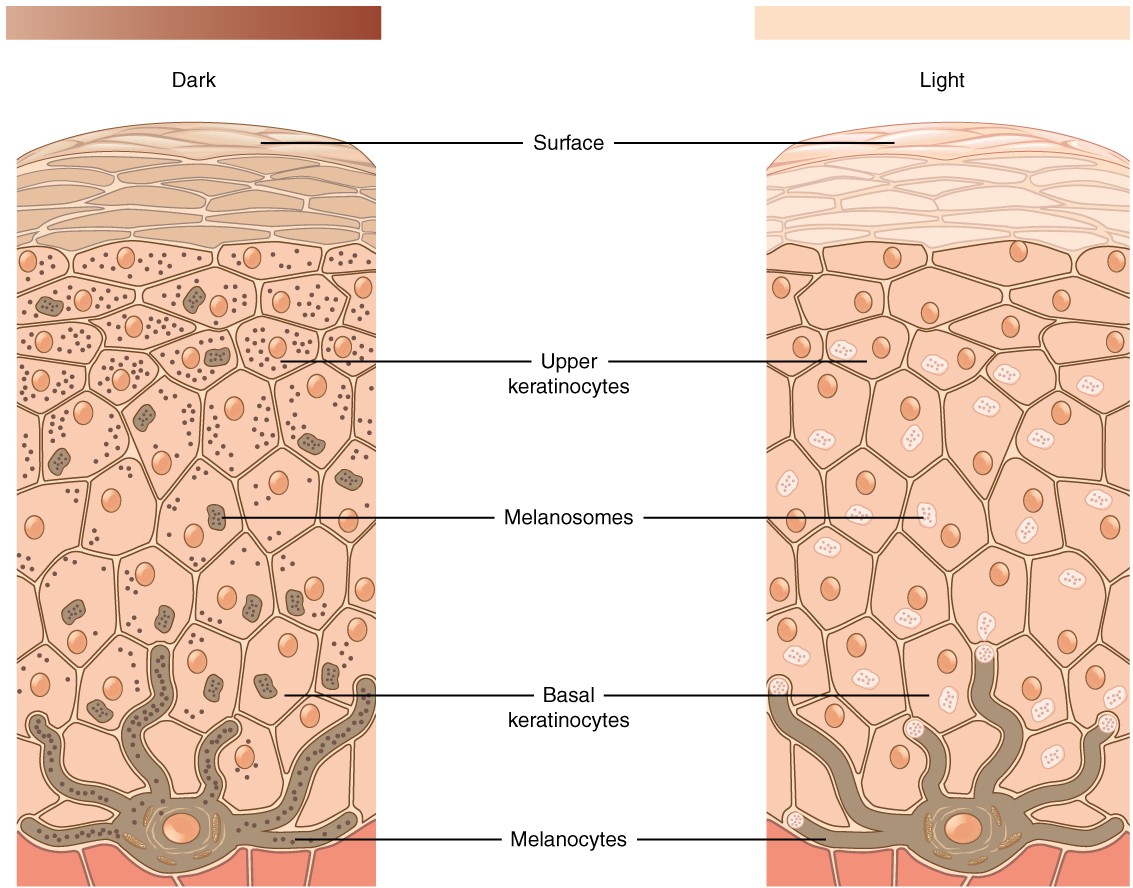
The color of skin is influenced by a number of pigments, including melanin, carotene, and haemoglobin. Recall that melanin is produced by cells called melanocytes, which are found scattered throughout the stratum basale of the epidermis (Figure 25.8).
Figure 25.8 Skin Pigmentation The relative coloration of the skin depends of the amount of melanin produced by melanocytes in the stratum basale and taken up by keratinocytes.
INTERACTIVE ACTIVITY
Skin pigmentation is historically related to Indigenous populations [1st panel]. The concentration of melanin is increased in populations living close to the equator. The melanocytes protect cell nuclei against UV-DNA damage, which is the reason for reduced skin cancer rates in darker skinned people [2nd panel]. Melanin production determines skin colour and is associated with ethnicity [3rd panel].
Accessory Structures of the Skin
Learning Objectives
By the end of this section, you will be able to:
- Identify the accessory structures of the skin
- Describe the structure of sweat glands and sebaceous glands
Accessory structures of the skin include hair, nails, sweat glands, and sebaceous glands.
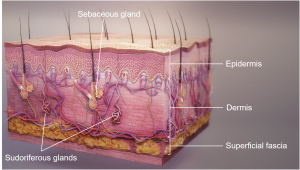
Figure 25.11 Glands of the skin Sudoriferous glands are coiled glands that excrete sweat through ducts opening at the epidermis, and sebaceous glands excrete sebum. [Modified from Scientific Animations]
INTERACTIVE LINK
Age-Associated Changes of Skin
All systems in the body accumulate subtle and some not-so-subtle changes as a person ages. Among these changes are reductions in cell division, metabolic activity, blood circulation, hormonal levels, and muscle strength (Figure 5.17). In the skin, these changes are reflected in decreased mitosis in the stratum basale, leading to a thinner epidermis. The dermis, which is responsible for the elasticity and resilience of the skin, exhibits a reduced ability to regenerate, which leads to slower wound healing. The superficial fascia, with its fat stores, loses structure due to the reduction and redistribution of fat, which in turn contributes to the thinning and sagging of skin. The deeper muscle and bone tissue is also remodeled during the ageing process.Other cells in the skin, such as melanocytes, also become less active, leading to a paler skin tone and lowered immunity.
Wrinkling of the skin occurs due to breakdown of its structure, which results from decreased collagen and elastin production in the dermis, weakening of muscles lying under the skin, and the inability of the skin to retain adequate moisture. The accessory structures also have lowered activity, generating thinner hair and nails, and reduced amounts of sebum and sweat. A reduced sweating ability can cause some elderly to be intolerant to extreme heat.
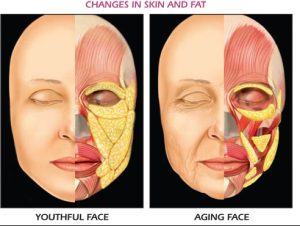
Figure 5.17 Ageing Generally, skin, especially on the face and hands, starts to display the first noticeable signs of aging, as it loses its elasticity over time. [https://doctorain.files.wordpress.com/2017/09/agingfacepicture.png]
Key Terms
apocrine sweat gland type of sweat gland that is associated with hair follicles in the armpits and genital regions
basal cell type of stem cell found in the stratum basale and in the hair matrix that continually undergoes cell division, producing the keratinocytes of the epidermis
dermal papilla (plural = dermal papillae) extension of the papillary layer of the dermis that increases surface contact between the epidermis and dermis
dermis layer of skin between the epidermis and hypodermis, composed mainly of connective tissue and containing blood vessels, hair follicles, sweat glands, and other structures
eccrine sweat gland type of sweat gland that is common throughout the skin surface; it produces a hypotonic sweat for thermoregulation
epidermis outermost tissue layer of the skin
integumentary system skin and its accessory structures
keratinocyte cell that produces keratin and is the most predominant type of cell found in the epidermis
Meissner corpuscle (also, tactile corpuscle) receptor in the skin that responds to light touch
melanin pigment that determines the color of hair and skin
melanocyte cell found in the stratum basale of the epidermis that produces the pigment melanin
Merkel cell receptor cell in the stratum basale of the epidermis that responds to the sense of touch
Pacinian corpuscle (also, lamellated corpuscle) receptor in the skin that responds to vibration
papillary layer superficial layer of the dermis, made of loose, areolar connective tissue
reticular layer deeper layer of the dermis; it has a reticulated appearance due to the presence of abundant collagen and elastin fibers
sebaceous gland type of oil gland found in the dermis all over the body and helps to lubricate and waterproof the skin and hair by secreting sebum
sebum oily substance that is composed of a mixture of lipids that lubricates the skin and hair
stratum basale deepest layer of the epidermis, made of epidermal stem cells
stratum corneum most superficial layer of the epidermis
stratum granulosum layer of the epidermis superficial to the stratum spinosum
stratum lucidum layer of the epidermis between the stratum granulosum and stratum corneum, found only in thick skin covering the palms, soles of the feet, and digits
stratum spinosum layer of the epidermis superficial to the stratum basale, characterized by the presence of desmosomes
sudoriferous gland sweat gland
superficial fascia connective tissue connecting the integument to the underlying bone and muscle