5
Chapter Objectives
- Describe the anatomical variation, population incidence of a range of phenotypes, and Australian and New Zealand context of select examples of the skeletal system, including the:
- bony pelvis
- skull (spheno-occipital synchondrosis and anterior fontanelle)
- Discuss the clinical and/or professional impact of anatomical variation of the skeletal system on patients and/or professional settings
Bony Pelvis
Variation Classification: Morphology
Description of Anatomy
The bony pelvis consists of three articulated bones: the right and left hip bones (os coxae) and the sacrum. The hip bones are irregular bones formed by the fusion of three separate primary ossification centres – the ilium, ischium and pubis. The sacrum is formed by the fusion of five individual sacral vertebrae. The bony pelvis connects the lumbar vertebrae of the back to the femora in the thighs, and functions to protect the inferior internal organs of the abdominopelvic cavity.
Bony pelves are sexually dimorphic, meaning that the morphology is different between males and females. Overall, the male pelvis is heavier and more robust than the female pelvis, which is lighter and more gracile. These sexually dimorphic differences in the pelvis are a result of the heavier build and larger muscles in males, and the adaptation for childbearing in females.
The right and left hip bones are connected anteriorly by the pubic symphysis. Posteriorly, the left and right hip bones are connected to the sacrum via the sacroiliac joint.
Test your knowledge of the anatomy of the pelvis by identifying the major structures in the pelvis image below. Check each of your answers by clicking on the question mark icon.
Examples of Phenotypic Variation
In a male pelvis, prominent markings may be seen in regions of muscle attachment due to the relatively larger muscular build. When comparing the shape of the pelvis between males and females, the female pelvis appears more shallow and wider, while the male pelvis is deeper and narrow. When viewing the pelvic inlet (the superior space contained within the pelvic brim), in a male this appears more circular or heart-shaped, while in a female the opening is oval in shape. The pelvic outlet (inferior space bordered by the coccyx, ischial tuberosities and subpubic angle) is also wider in the female pelvis. These adaptations to the female pelvis allow for the movement of the foetal head through the apertures during labour. A specific region of the pelvis that demonstrates sexual dimorphism is the subpubic angle, which is formed by the left and right ischiopubic rami. Due to the wider pelvis in the female, this angle is typically much larger than what is seen in a male pelvis. The wider orientation of the female pelvis also results in an oval obturator foramen, with a more circular obturator foramen in males.
Four morphological examples of sexual dimorphism are presented in a series of diagrams below. Use the labelled slider tool to move between each diagram.
[Image: A. Kimmorley CC BY-NC]
Phenotypic Variation of the Subpubic angle in Different Populations
| Source | Franklin et al. (2014) | Small et al. (2012) | Karakas et al. (2013) | Setiawati et al. (2023) | Mostafa et al. (2016) | Mohd Ali et al. (2020) | Akhlaghi et al. (2017) | |
| Population | Western Australian | South African (SA) | Eastern Anatolia | Indonesian | Egyptian | Malaysian | Iranian | |
| Sample size | 400
(CT) |
68 SA European
77 SA Zulu/Xhosa (Dry bone) |
109
(CT) |
204
(CT) |
94
(CT) |
100
(CT) |
325
(Pelvic x-ray) |
|
| Male | 69° | 71° in SA European
64° in SA Zulu/Xhosa |
66° | 100° | 76° | 69° | 101° | |
| Female | 89° | 94° in SA European
84° in SA Zulu/Xhosa |
83° | 128° | 107° | 87° | 140° | |
Australian and New Zealand Context
As you can see from the table above, the subpubic angle varies greatly between different populations. Recognising this population variation is important in several professional contexts but is particularly important in the context of forensic identification. This is why researchers around the world perform studies that investigate the morphological features of the pelvis (as well as other bones) within different populations. Unfortunately, there are limited detailed studies available which document the range of phenotypic variation in an Australia population, with none available (to the best of our knowledge) in a New Zealand population.
One study, conducted in 2014 by Franklin et al., have investigated skeletal pelvic dimorphism in a contemporary Western Australian population. Researchers performed this study to confirm the accuracy of using pelvic measurements to estimate sex, and subsequently develop a set of morphometric standards specific to an Australian population. Computed tomography (CT) images of 200 males and 200 females were used within the study, and 24 landmarks were investigated. The subpubic angle had 100% accuracy in discriminating between the male and female pelvis; with the average angle recorded as 89° in females and 69° in males. This means that not only does the subpubic angle differ between different populations, but it also varies significantly between sexes. Compared to other populations, as described within the table above, the subpubic angle of Australian individuals is notably narrow, and similar to that of a South African population.
Refer to part 4 of this textbook (Applying Skeletal Variation to Professional Contexts) for more information on how skeletal variation is used in forensic anthropology to estimate a biological profile!
Case Study on Bony Pelvis: Pelvic Variation and Childbirth

A 27-year-old pregnant patient presents for her first pre-natal visit. After taking a medical history, her physician learns that she suffered from a fractured pelvis in her early twenties. Review the anatomy of the pelvis of the patient in the radiograph on the right.
QUESTION 1: Discuss the morphological features that indicate this patient presents a typical female bony pelvis.
QUESTION 2: Pelvimetry is a technique used to assess the size of the female pelvis to determine whether the patient may be able to deliver vaginally. Consider what diameter measurements may be relevant and where these diameter measurements could be conducted. What bony landmarks could be used when performing pelvimetry?
QUESTION 3: The shape of the bony birthing canal is highly variable between females. What may be the implications of variation in morphology of the pelvic inlet and pelvic outlet? What bony features in this region may impact delivery of a foetus?
References and further reading
Akhlaghi, M., Bakhttavar, K., Mokhtari, T., Mehdizadeh, F., Parsa, V. A., Farahani, M. V., & Sadeghian, M. (2017). Using subpubic angle in sex determination and stature estimation: an anthropometric study on Iranian adult population. International Journal of Medical Toxicology and Forensic Medicine, 7(4), 195-202.
Franklin, D., Cardini, A., Flavel, A., & Marks, M. K. (2014). Morphometric analysis of pelvic sexual dimorphism in a contemporary Western Australian population. International Journal of Legal Medicine, 128(5), 861–872. https://doi.org/10.1007/s00414-014-0999-8
Karakas, H. M., Harma, A., & Alicioglu, B. (2013). The subpubic angle in sex determination: Anthropometric measurements and analyses on Anatolian Caucasians using multidetector computed tomography datasets. Journal of Forensic and Legal Medicine, 20(8), 1004–1009. https://doi.org/10.1016/j.jflm.2013.08.013
Mohd Ali, S. H., Omar, N., Shafie, M. S., Nik Ismail, N. A., Hadi, H., & Nor, F. M. (2020). Sex estimation using subpubic angle from reconstructed three-dimensional computed tomography pelvic model in a contemporary Malaysian population. Anatomy & Cell Biology, 53(1), 27–35. https://doi.org/10.5115/acb.19.135
Mostafa, E. M. A., M. Dessouki, S. K., Hashish, R. K., M. Gad, A. A., & M. Khafagy, A. A. (2016). Adult Sex Identification Using Three-Dimensional Computed Tomography (3D-CT) of the Pelvis: A Study Among a Sample of the Egyptian Population. Arab Journal of Forensic Sciences & Forensic Medicine, 1(3). https://doi.org/10.12816/0026460
Setiawati, R., Rahardjo, P., Ruriana, I., & Guglielmi, G. (2023). Anthropometric study using three-dimensional pelvic CT scan in sex determination among adult Indonesian population. Forensic Science, Medicine, and Pathology, 19(1), 24–33. https://doi.org/10.1007/s12024-022-00526-w
Small, C., Brits, D. M., & Hemingway, J. (2012). Quantification of the subpubic angle in South Africans. Forensic Science International, 222(1), 395.e1–395.e6. https://doi.org/10.1016/j.forsciint.2012.06.002
Skull (Spheno-Occipital Synchondrosis and Anterior Fontanelle)
Variation Classification: Developmental timing
Description of Anatomy
The spheno-occipital synchondrosis is a cartilaginous joint located between the sphenoid and occipital bone at the base of the skull. Also known as the basicranial synchondrosis, it is located anterior to the foramen magnum. It is considered a hyaline cartilaginous joint and is only present during growth of the skeleton, where the cartilage progressively disappears until it completely ossifies during skeletal maturation.
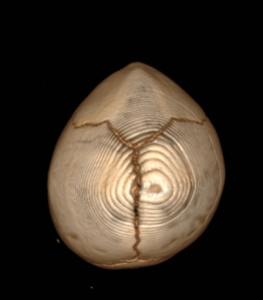
The anterior fontanelle forms through a connective tissue juxtaposition of the two frontal and two parietal bones in the neonatal skull. It is the largest of six fontanelles, known in layperson terminology as ‘soft spots’. The anterior fontanelle is diamond-shaped and characteristically flat, with the superior sagittal sinus coursing deep to it. This membranous structure will eventually close with ossification of the cranial bones.
Examples of Phenotypic Variation
Results of studies on skeletal growth have demonstrated evidence of interpopulation variation, which is the variance between populations, indicating that standards should not be extrapolated between populations. Secular change, which is the biological change over time, has also resulted in accelerated growth and development, emphasising the need for contemporary population-specific studies. The age of skeletal maturation of the spheno-occipital synchondrosis is variable between studies. Fusion is likely to occur during adolescence, and is associated with maturational events such as the adolescent growth spurt and hormonal fluctuations. Fontanelle size has also been shown to vary between geographically-different populations. The anterior fontanelle is likely to close during the first two years of life.
Four stages of skeletal maturation of the spheno-occipital synchondrosis are presented in a series of diagrams below. Use the slider tool to move between each developmental stage and read the text underneath that describes each stage. By dragging the slider tool you can view the transition between each developmental stage.
[Images: M. Reynolds CC BY-NC 4.0]
Five stages of temporal closure of the anterior fontanelle are presented in a series of diagrams below. Use the slider tool to move between each developmental stage and note the age at each stage. By dragging the slider tool you can view the transition between each developmental stage.
[Image: © K. Andrew 2022. Reproduced with permission]
Developmental Timing of Phenotypic Variation in Different Populations
|
Anterior Fontanelle |
||||||
| Source | Lottering et al. (2020) | Kirkpatrick et al. (2019) | Noble et al. (2017) | Esmaeili et al. (2015) | Pindrik et al. (2014) | |
| Population | Australian (Queensland) | New Zealand | Australian (Western Australia) | Iranian | USA | |
| Sample size | 256
(CT) |
116 Maori/Pasifika
47 NZ European (CT) |
68
(CT) |
550
(Clinical) |
464
(CT) |
|
| Complete closure | By 20 months in males
By 24 months in females |
By 23 months in Maori/Pasifika
By 24 months in NZ European |
By 28 months | By 15-18 months | 90% of individuals by 24 months | |
|
Spheno-Occipital Synchondrosis |
||||||
| Source | Lottering et al. (2014) | Franklin and Flavel (2014) | Langley-Shirley and Jantz (2011) | Bassed et al. (2010) | Coqueugniot and Weaver (2007) | |
| Population | Australian (Queensland) | Australian (Western Australia) | USA | Australian (Victorian) | Portuguese | |
| Sample size | 864
(CT) |
312
(CT) |
162
(Dry bone) |
527
(CT) |
137
(Dry bone) |
|
| Complete closure | By 15.6 years in males
By 13.8 years in females |
By 19.3 years in males
By 16.3 years in females |
By 22.8 years in males
By 20.1 years in females |
By 17 years | By 23 years | |
Australian and New Zealand Context
As you can see from the table above, complete closure of the anterior fontanelle occurs at different ages between populations. In a Queensland, Australian population, it was shown that anterior fontanelle surface area progressively declined from birth. Lottering et al. (2020) mapped the closure of the anterior fontanelle using computed tomography images, and observed that within a Queensland paediatric population (n=256), anterior fontanelle surface area (normalised for variation in head size) underwent the greatest velocity of change between 3-6 and 6-9 months. Lottering et al. (2020) further reports that the most significant growth changes to the neurocranium occur within the first 8 months after birth. It has been assumed that the anterior fontanelle is consistent with the shape of a quadrilateral, however the research has shown that the metopic and coronal sutures are the first to ossify, and that the sagittal diameter of the anterior fontanelle is significantly longer than the coronal diameter in the first 6 months. Interestingly, the dimensions of the anterior fontanelle reach equal proportions in the 6-9 month cohort (Lottering et al., 2020), resulting in the expected diamond-shaped morphology. Normative values for anterior fontanelle size are provided for modern infants in this Australian study (Lottering et al., 2020). Timing of anterior fontanelle closure has also been quantified in a Western Australian population (n=68). This study showed that the greatest proportion of fusion occurred before 12 months, and also provided mean anterior fontanelle area values (Noble et al., 2017).
One study conducted in 2019 investigated closure of the anterior fontanelle in a New Zealand (NZ) population (Kirkpatrick et al., 2019). The investigation of computed tomography images identified that in the Maori/Pasifika group (n=116), the earliest closure of the anterior fontanelle occurred at 6 months, while in the NZ European group (n=47), the earliest closure of the anterior fontanelle occurred at 8 months. In the Maori/Pasifika group, anterior fontanelle closure increased to 60% by 13-18 months, and in the NZ European group, the anterior fontanelle was closed in 50% at 13-18 months (Kirkpatrick et al., 2019). The researchers found that the mean surface area of the anterior fontanelle in the Maori/Pasifika 1-3 month cohort was 606mm2, while in the NZ European 1-3 month cohort, the mean surface area was 854mm2. In the Maori/Pasifika group, the anterior fontanelle surface area decreased to a mean of 487mm2 in the 4-6 month cohort, while in the NZ European group, the anterior fontanelle surface area decreased to a mean of 603mm2 in the 4-6 month cohort.
Development of the spheno-occipital synchondrosis was also investigated in a modern Queensland, Australian population (n=864) using computed tomography (Lottering et al., 2014). This study found that females are likely to transition to complete fusion of the spheno-occipital synchondrosis at 13.1 years, and males at 15.6 years (Lottering et al., 2014). Complete fusion of the synchondrosis was seen in all females over 13.8 years, and all males over 16.3 years (Lottering et al., 2014). In comparison, in a Victorian, Australian population (n=527), complete closure of the spheno-occipital synchondrosis was observed in both females and males by the age of 17 years (Bassed et al., 2010). In a Western Australian population (n=312), complete fusion of the synchondrosis was documented in all females over 16.3 years, and all males over 19.3 years (Franklin and Flavel, 2014).
Case Study on Skeletal Growth and Fusion: Craniosynostosis
A mother and father attend the medical imaging department with their 7 month old son, who presents with an abnormal head shape. A computed tomography (CT) scan of the head was performed to assess the skull sutures. Review the 3D reconstruction of the patient’s skull on the right.
QUESTION 1: Fusion of the metopic suture was identified, with bony ridging in the midline of the frontal bone. Consider the impact of premature fusion of cranial sutures on the development of the nervous system. How could craniosynostosis (premature fusion) impact brain development?
QUESTION 2: Compare this patient’s scan with the anterior fontanelle diagrams above, and identify if this patient has presented with premature fusion of the anterior fontanelle. If premature closure of the fontanelles occurred in-utero, what impact would this have on parturition?
QUESTION 3: In most cases, craniosynostosis requires surgery for aesthetic and psychosocial reasons. How may a surgeon remodel cranial bones to treat skull malformation?
References and Further Reading
Bassed, R. B., Briggs, C., & Drummer, O. H. (2010). Analysis of time of closure of the spheno-occipital synchondrosis using computed tomography. Forensic Science International, 200(1), 161–164. https://doi.org/10.1016/j.forsciint.2010.04.009
Coqueugniot, H., & Weaver, T. D. (2007). Brief communication: Infracranial maturation in the skeletal collection from Coimbra, Portugal: New aging standards for epiphyseal union. American Journal of Physical Anthropology, 134(3), 424–437. https://doi.org/10.1002/ajpa.20683
Esmaeili, M., Esmaeili, M., Sharbaf, F. G., & Bokharaie, S. (2015). Fontanel size from birth to 24 months of age in Iranian children. Iranian Journal of Child Neurology, 9(4), 15–23. https://doi.org/10.22037/ijcn.v9i4.7754
Franklin, D., & Flavel, A. (2014). Brief Communication: Timing of spheno-occipital closure in modern Western Australians. American Journal of Physical Anthropology, 153(1), 132–138. https://doi.org/10.1002/ajpa.22399
Kirkpatrick, J., Bowie, S., & Mirjalili, S. A. (2019). Closure of the anterior and posterior fontanelle in the New Zealand population: A computed tomography study. Journal of Paediatrics and Child Health, 55(5), 588–593. https://doi.org/10.1111/jpc.14253
Lottering, N., MacGregor, D. M., Alston, C. L., & Gregory, L. S. (2014). Ontogeny of the spheno-occipital synchondrosis in a modern Queensland, Australian population using computed tomography. American Journal of Physical Anthropology, 157(1), 42–57. https://doi.org/10.1002/ajpa.22687
Lottering, N., Alston, C. L., Barry, M. D., MacGregor, D. M., & Gregory, L. S. (2020). Temporal mapping of the closure of the anterior fontanelle and contiguous sutures using computed tomography, in silico models of modern infants. Journal of Anatomy, 237(2), 379–390. https://doi.org/10.1111/joa.13200
Noble, J., Flavel, A., & Franklin, D. (2017). Quantification of the timing of anterior fontanelle closure in a Western Australian population. Australian Journal of Forensic Sciences, 49(2), 142–153. https://doi.org/10.1080/00450618.2016.1153150
Pindrik, J., Ye, X., Ji, B. G., Pendleton, C., & Ahn, E. S. (2014). Anterior Fontanelle Closure and Size in Full-Term Children Based on Head Computed Tomography. Clinical Pediatrics, 53(12), 1149–1157. https://doi.org/10.1177/0009922814538492
Shirley, N. R., & Jantz, R. L. (2011). Spheno-Occipital Synchondrosis Fusion in Modern Americans. Journal of Forensic Sciences, 56(3), 580–585. https://doi.org/10.1111/j.1556-4029.2011.01705.x

